Health systems strengthening


Feature Story
Egyptian medical students meet to address stigma and discrimination in health-care settings
25 April 2018
25 April 2018 25 April 2018Stigma and discrimination and other human rights violations occur in health-care settings worldwide, barring people from accessing health services or enjoying quality health care. Such stigma and discrimination further increases the vulnerability of people living with and affected by HIV.
To discuss this problem, nearly 300 Egyptian medical students, representing 18 universities across Egypt, met with representatives of academia, civil society, the government and the Egyptian Medical Syndicate. With support from UNAIDS, the Egyptian branch of the International Federation of Medical Students’ Associations held a one-day consultation on HIV-related stigma and discrimination in health-care settings on 21 April in Cairo, Egypt.
“People living with HIV should have equal rights and opportunities. Denial of access to health-care services is unacceptable. Through this consultation, we aim to inform our national strategy with new interventions for addressing stigma and discrimination,” said Walid Kamal, the National AIDS Programme Manager for Egypt.
During the consultation, the participants took stock of the progress made in addressing stigma and discrimination and decided to hold an ongoing dialogue to identify actions to address stigma and discrimination in health-care settings.
“We are witnessing an unprecedented opportunity for addressing discrimination in health-care settings with political support and programmatic vision. While resources are scarce, we count on the support of medical students as leaders of tomorrow and the power of volunteerism to address this issue,” said Ahmed Khamis, the UNAIDS Country Manager for Egypt.
The participants agreed that accountability mechanisms need to be in place to monitor and evaluate interventions, ensuring that proper actions are taken by the relevant authorities to address rights violations in health-care settings.
“Medical ethics is a must among health-care providers. The Egyptian Medical Syndicate is organizing workshops and conferences to enforce ethics among health-care providers. I would like to remind you all of the rights of patients,” said Sherine Ghaleb, representative of the Egyptian Medical Syndicate.
The participants agreed to prioritize launching the Ministry of Health and Population’s stigma-free policy and integrating HIV-related stigma and discrimination in the module on ethics taught to all doctors who graduate in Egypt. They also agreed to give access to the accountability and investigation mechanism of the Egyptian Medical Syndicate to civil society organizations and people living with HIV in order to report violations and to roll out information on post-exposure prophylaxis in the curricula of medical schools.
The recommendations made during the consultation were endorsed by the National AIDS Programme and will be included in Egypt’s road map for addressing HIV stigma and discrimination in health-care settings. Progress of the road map will be monitored by a group that includes a strong representation from people living with HIV.
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Feature Story
Mobile phones provide massive potential to move towards e-health systems
26 April 2018
26 April 2018 26 April 2018Shiv Kumar, from Swasti Health Catalyst in India, decided to build a mobile and web application called Taaras (rapid progress). He had watched peer educators work with sex workers in Bangalore, India, and realized that he could make their jobs a lot simpler and more efficient. The south-east Indian city has become a major hub and, as a result, the population has boomed, as have sex workers.
After seeing outreach workers, mostly former sex workers, lugging notebooks and jotting down information and recalling appointments and treatment pickups, he created an app that helps with data collection. “Icons and swipes allow outreach workers to enter all sorts of stuff and swipe and pick up where they left off,” Mr Kumar said. They can also text multiple recipients with reminders and invitations.
“Outreach can no longer be a one-way street. You have to engage the patient,” he said.
The app rolled out in five Indian states in English as well as four regional languages. Since its debut in March 2016, there are now more than 400 users following about 120 000 sex workers.
Bangalore outreach worker Natranity said that she has a lot less paperwork to deal with. “All the data of a particular person is now in one place, versus five or six registers that I had to consult,” she said. Her colleague, Abdul, agreed, “I see about 10 to 15 people a day and what saves me a lot of time is not asking the same questions over and over again, because I can consult their profile.”
The phones had their limits, they explained. “At the initial stage, it’s important to build trust to avoid any discomfort in case they think we are taking photos or recording them,” Natranity said.
Prachi Patel, a technology developer at Swasti, sees Taaras as a bridge to an overall solution. “The app is a helper; outreach workers still do all the talking,” she said. A by-product of the app has been higher engagement with sex workers and an increase in reporting incidents of violence. For confidentiality, the app has a stress password that scrambles the data in the event that someone tries to access the information.
UNAIDS Senior Adviser Philippe Lepère commends such efforts and believes e-health has a huge potential. Not only can it strengthen health systems, it also empowers people to manage their own care. Referring to the World Health Organization’s Guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach, he said that they advocate using text messages to remind people to take their treatment and encourage newly diagnosed people to seek out services.
For this to work, however, he stressed the importance of confidentiality and respect of the user. “Receiving an HIV-related SMS can have drastic consequences in some communities,” he explained. That's why, he said, the content and the frequency have to be ironed out beforehand. “Most importantly, it’s urgent to shift from pilot studies to a larger implementation of programmes at a sufficient scale that can then be integrated within health systems,” Mr Lepère said.
“In certain countries, digital apps have flooded the market and the government has no way of accessing the data or doing any quality control,” he said.
Hani Eskandar, from the International Telecommunications Union, definitely sees mobile phones as paving the way towards universal health coverage.
But, in his view, e-health systems are far from a reality. “Countries have not yet grasped the benefits of this, because they are still focused on vaccines and building hospitals rather than outreach,” he said. He is pushing for governments to rebuild infrastructures that integrate digital platforms.
“It's simple,” he said. “We need for mentalities to change at all levels and stop thinking that the phone is just a gadget.”
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025



Feature Story
A united rallying cry: Time to make health care systems more flexible and innovative
16 April 2018
16 April 2018 16 April 2018Seven months after launching the catch-up plan in western and central Africa, progress on increasing the numbers of people on antiretroviral treatment continues to lag in the region. Many countries will not reach key targets by 2020 if the current systems remain unchanged.
"Overall we saw a 10% percent increase of people on treatment, which is not enough," said UNAIDS Executive Director Michel Sidibé. "Now, there is even more a sense of urgency."
Mr Sidibé, however, pointed to the success in the Democratic Republic of Congo where there was a clear increase in the number of people living with HIV accessing ARVs. The reasons for the positive trend included civil society and political leadership working closely together as well as community HIV testing and the training of 11 000 health care workers.
"More than ever there is a need to rethink health systems and alternatives for people to access health care," he said.
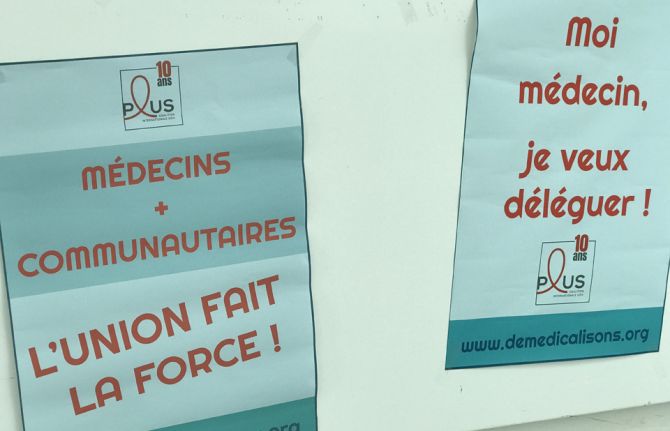
The call to delegate patient care to communities was a major rallying call during AFRAVIH, the international francophone HIV and hepatitis conference held in Bordeaux, France, early April. Mr Sidibé briefly shared the stage at the opening ceremony with the civil society organisation Coalition PLUS. They declared that the key to success in ending AIDS involved joining forces between doctors and community health workers and giving more leeway to communities to respond to the local needs of their own people.
Under the banner, "De-medicalize" the organisation explained that doctors will never be replaced but that there were too few of them and people living with HIV didn't require acute care.
Coalition Plus' recent report states that governments and the medical practitioners should delegate more tasks to nurses and community health workers. In addition to allowing for more targeted prevention and faster access to treatment, delegation of non-medical tasks would lighten the load on overburdened health systems. West and central Africa represent 17% of the total population living with HIV but 30% of deaths in the region are from AIDS-related illnesses. This is a region, according to UNAIDS and its partners, that can truly benefit from community models of care.
What worries Médecins Sans Frontières (MSF) is the risk of a significant drop in resources for treatment will hamper recent improvements in west and central Africa. This concern stems from the fact that Global Fund estimates a 30% drop in fund allocations to the region for 2018 – 2020 compared to signed HIV grants in the previous allocation period. In 2016, MSF was among the first to sound alarm bells regarding the region's high HIV death toll and the up to 80% of children unable to access antiretroviral therapy. MSF HIV Policy Advisor and Advocacy Officer Nathalie Cartier said that they supported the west and central Africa catch-up plan but that it needed to be fully implemented. "Political will has been promising but now it's time to make it a reality on the ground so that people living with HIV can reap the benefits," she said.
Global Fund supported the catch-up plan and works closely with countries in order to maximize the impact of the investments. They believe that leveraging additional domestic financing for health is crucial to increase country ownership and build sustainable programs.
All the more reason to decentralize healthcare systems and capitalize on innovations to keep health costs down. HIV self-testing, new medicines and high impact strategies involving communities are critical to improving efficiencies. "With point-of-care (POC) testing in communities and homes, delays are minimal between diagnosis and initiating treatment," said Cheick Tidiane Tall, Director of Réseau EVA, a network of pediatric doctors specialized in HIV care. “In the long run, that's a lot of people and resources saved,” he added.
Côte d'Ivoire Infectious and Tropical Diseases professor Serge Eholié couldn't agree more. "Flexible health care systems capitalizing on various innovations makes a lot of sense," he said. Turning to the Minister of Health in the Central African Republic, Pierre Somse, he asked, 'How do you respond?'
Mr Somse, also a trained doctor, said, "We doctors will stay doctors. However, there is a need for us to lean on communities and vice versa." He added, "at the heart of the issue are patients and they are and should always be the priority."
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025




Feature Story
Communities at the heart of the AIDS response in Zambia
07 March 2018
07 March 2018 07 March 2018Zambia has made good progress in its AIDS response. In 2016, the country had more than 800 000 people on HIV treatment, with 83% of pregnant women living with HIV accessing it. To better understand the progress, and the challenges, Michel Sidibé, UNAIDS Executive Director, visited the Chilenje health facility in Lusaka, Zambia, during a visit to the country from 5 to 7 March.
The Chilenje facility offers HIV treatment, a prevention of mother-to-child transmission of HIV programme and tailored services for adolescents and young people. At the facility’s youth-friendly space, peer educators facilitate service uptake by young people and reach out to schools and other groups within their community with counselling and sensitization.
“We need to build cities of the future where services are not only available to people, but they are also tailored to their needs. This is the rationale behind the Fast-Track cities initiative, of which Lusaka is an excellent example,” said Mr Sidibé during his visit.
The facility offers extended hours in the evening and weekends so that people who are unable to access health services outside of standard operating hours can access HIV treatment and other services.
“Young people often fall through the cracks of the health system for fear of judgement or stigma. Owing to the large number of adolescents and young people in our community, we have set up a youth-friendly space,” said Malinba Chiko, the Superintendent of the Chilenje health facility.
Earlier in the day, Mr Sidibé met with members of civil society, who raised the issue of access to HIV and sexual and reproductive health services for key populations, especially gay men and other men who have sex with men and sex workers. Mr Sidibé reiterated that civil society is at the heart of the AIDS response and, for it to be sustainable, the voice and decision-making of civil society are essential.
Region/country
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025
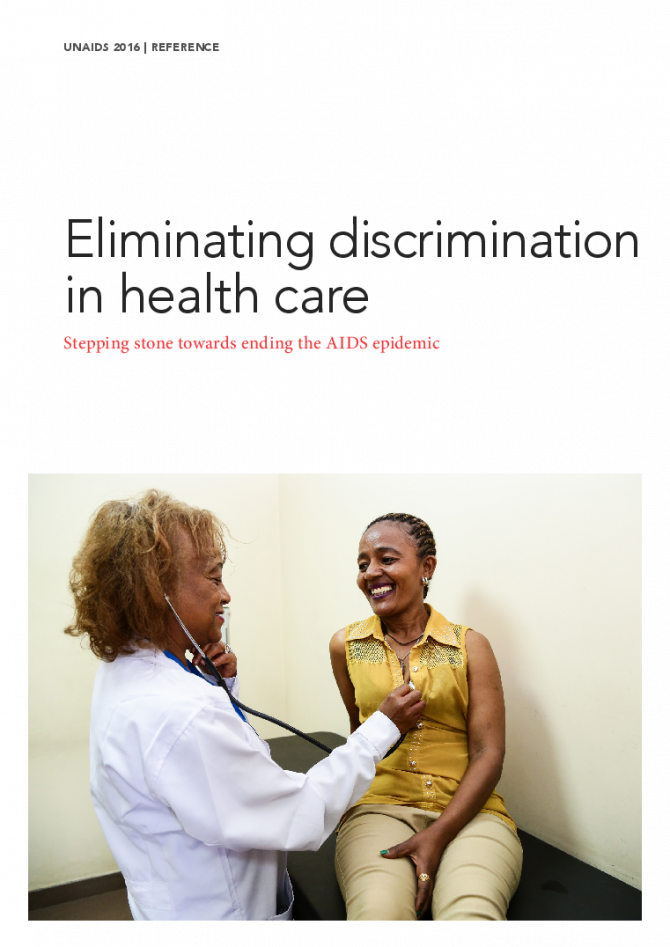
Documents
Eliminating discrimination in health care — Stepping stone towards ending the AIDS epidemic
10 December 2016
This report briefly describes and defines the challenges and impacts of discrimination in health-care settings. Such discrimination affects people seeking access to HIV prevention, testing, treatment, care and support measures, as well as health-care workers in their workplace. International human rights standards provide the rationale for catalysing global action to eliminate such discrimination. This report aims to serve as a reference for policy-makers and other key stakeholders engaged in shaping policies and programmes to regulate health care, and eliminate discrimination and other structural barriers to achieving healthy lives for all.
Related
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
UNAIDS data 2024
02 December 2024
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
01 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Evelyn Siula: A journey of strength and solidarity
Evelyn Siula: A journey of strength and solidarity
18 November 2024
Documents
Confronting discrimination
02 October 2017
This report compiles the latest body of evidence on how stigma and discrimination create barriers across the HIV prevention, testing and treatment cascades and reduce the impact of the AIDS response. The report also brings together best practices on confronting stigma and discrimination, providing a valuable resource for programme managers, policy-makers, health-care providers and communities. The evidence shows that the establishment of people-centred service delivery models, supportive legal and policy frameworks, monitoring and enforcement mechanisms, and sensitization training for health-care workers and other duty bearers can promote inclusion and increase access to services.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
UNAIDS data 2024
02 December 2024
Documents
Confronting discrimination advancing health
02 October 2017
Everywhere in the world, human rights violations, fear, prejudice, stigma and discrimination persist, including in health-care settings. Today, I am launching a UNAIDS report entitled Confronting discrimination, which describes the magnitude and impact of stigma and discrimination in health care and gives concrete examples for addressing it.
Related
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
55th meeting of the UNAIDS Programme Coordinating Board
10 December 2024
UNAIDS data 2024
02 December 2024
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
01 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Evelyn Siula: A journey of strength and solidarity
Evelyn Siula: A journey of strength and solidarity
18 November 2024




Update
Discussing global health at the Johns Hopkins Bloomberg School of Public Health
15 September 2017
15 September 2017 15 September 2017UNAIDS Executive Director Michel Sidibé met with students and staff during a visit to the Johns Hopkins Bloomberg School of Public Health in Baltimore, United States of America, on 15 September.
During an open dialogue in the school’s Sheldon Hall, Mr Sidibé and the Dean of the school, Michael Klag, joined with students, faculty, researchers, global health leaders and alumni to discuss global health, systems for health, leaving no one behind and social justice. Mr Sidibé expressed his concerns about the fragmented global health system and introduced his vision of systems for health that engage all relevant constituencies, including civil society, governments and scientists, and a global health financing institution that goes beyond HIV, tuberculosis and malaria. In addition, he said, there is an urgent need for an instrument for global health advocacy and accountability.
The visit also saw Mr Sidibé meet with a group of Sommer Scholars to discuss their future contributions to global public health and with members of the Johns Hopkins University Center for AIDS Research.
Quotes
“The future of UNAIDS is being a global health advocacy and accountability organization that integrates HIV with reproductive health and other important health issues. Achieving this will help the organization transform itself and reduce the fragmentation that’s too common in global health.”
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Update
Call to break down silos between HIV and cervical cancer prevention
03 October 2017
03 October 2017 03 October 2017The Executive Director of UNAIDS, Michel Sidibé, has highlighted the urgent need to break down silos and integrate HIV and sexual and reproductive health services, including for the prevention and control of cervical cancer, which is an AIDS-defining illness. Mr Sidibé delivered his message at the International Agency for Research on Cancer in Lyon, France, on 3 October.
Leveraging the experience of more than three decades of the AIDS response, Mr Sidibé called for greater mobilization and the breaking down of silos between programmes, movements and services to deliver comprehensive sexual and reproductive health services for women and girls. He also reiterated the need to engage with civil society.
Women living with HIV have an up to five times greater risk of developing cervical cancer, which is the second most common cancer among women living in low- and middle-income countries. Despite cervical cancer being highly preventable with the human papillomavirus vaccine and generally curable with early diagnosis and treatment, more than 528 000 women are diagnosed with it every year and around 266 000 die needlessly, almost 90% of whom live in low- and-middle-income countries.
During his speech, Mr Sidibé highlighted the immense opportunities provided by the Sustainable Development Goals and the 2016 United Nations Political Declaration on Ending AIDS, as well as the resources made available through the Global Fund to Fight AIDS, Tuberculosis and Malaria, which reflect strong global commitment to scaling up integrated services to address coinfections and comorbidities.
Quotes
“It is an unacceptable tragedy that women are dying from cervical cancer because of where they are born, because they are poor and because they do not have access to the life-saving vaccines, diagnostics and treatment available to girls and women in high-income countries.”
“Chronic infections are associated with around one in six cancers worldwide and more than one in three in sub-Saharan Africa. Working collaboratively in a strategic manner across the HIV and cancer fields offers many potential opportunities to reduce the disease burden in some of the world’s most vulnerable populations.”


Press Release
UNAIDS warns that HIV-related stigma and discrimination is preventing people from accessing HIV services
03 October 2017 03 October 2017New report from UNAIDS gives evidence and highlights best practices on confronting stigma and discrimination to ensure access to health services
GENEVA, 3 October 2017—UNAIDS has released a new report showing how stigma and discrimination is creating barriers to accessing HIV prevention, testing and treatment services and putting lives at risk.
The report, Confronting discrimination: overcoming HIV-related stigma and discrimination in health-care settings and beyond, was launched by the Executive Director of UNAIDS, Michel Sidibé, during the Human Rights Council Social Forum. It shows that people living with HIV who experience high levels of HIV-related stigma are more than twice as likely to delay enrolment into care than people who do not perceive HIV-related stigma.
“When people living with, or at risk of, HIV are discriminated against in health-care settings, they go underground. This seriously undermines our ability to reach people with HIV testing, treatment and prevention services,” said Mr Sidibé. “Stigma and discrimination is an affront to human rights and puts the lives of people living with HIV and key populations in danger.”
Often, people living with HIV avoid going to clinics for fear of having their status disclosed or of suffering further stigma and discrimination based on their HIV status. Across 19 countries with available data, one in five people living with HIV avoided going to a clinic or hospital because they feared stigma or discrimination related to their HIV status. When people living with HIV wait until they are very ill before seeking help, they are less likely to respond well to antiretroviral therapy.
The report highlights that these fears are not unfounded. Across 19 countries with available data, one in four people living with HIV have experienced discrimination in health-care settings and one in three women living with HIV have experienced at least one form of discrimination in health-care settings related to their sexual and reproductive health.
Where programmes have been put in place to respond to stigma and discrimination, access to services for HIV prevention, testing and treatment has improved. In one clinic in Namibia, a shift towards integrated health service delivery led to a 20% reduction in deaths among people with HIV.
The report highlights that, in order to reach all people living with, or at risk of, HIV and to link them with HIV prevention and treatment services, the world must step forward and confront discrimination.
The Human Rights Council Social Forum is taking place in Geneva, Switzerland, from 2 to 4 October under the theme of Promotion and protection of human rights in the context of the HIV epidemic and other communicable diseases and epidemics.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.