HIV Treatment




Feature Story
Peru approves groundbreaking law to extend health coverage for migrants with HIV and TB
21 October 2024
21 October 2024 21 October 2024In a milestone decision, the Peruvian Congress has passed legislation that extends temporary health insurance coverage to migrants diagnosed with HIV and tuberculosis (TB). This law allows non-resident foreigners to access healthcare services through the public health insurance system (known by the Spanish acronym SIS) while they complete their immigration processes.
This law, which incorporates proposals from Law Bills 5253, 5554, and 7260, represents a significant step in reducing barriers for migrant populations, ensuring timely medical attention without the need for official residency documentation. Now, migrants affected by HIV or TB can receive vital healthcare services, including medical consultations and diagnostic exams, regardless of their immigration status.
The legislative breakthrough follows over two years of advocacy led by the Grupo Impulsor, a coalition that includes UNAIDS, alongside partners such as USAID’s flagship initiative Local Health System Sustainability Project (LHSS), IOM, UNHCR, the Peruvian Observatory of Migration and Health of the Peruvian University Cayetano Heredia (OPEMS-UPCH), Colectivo GIVAR, VENEACTIVA, the Peruvian TB Social Observatory, and Partners in Health.
Likewise, providing timely treatment for migrants with HIV or TB not only improves their quality of life but also reduces the risk of transmission, making it a crucial public health measure benefiting everyone. It also saves money: early care is far more cost-effective, preventing advanced cases that strain the health system.
A cost-benefit analysis reveals that Peru could save around 5 million soles ($1.33 million USD) annually by preventing new infections and another 54 million soles ($14.58 million USD) through avoiding productivity losses linked to AIDS and TB-related deaths.
Migrants living with HIV in Peru remain among the most discriminated groups in the country, with 70.7% reporting stigma, according to the Ministry of Justice and Human Rights. They also face heightened vulnerability due to xenophobia, violence, and exploitation—nearly half of them have experienced physical violence or sexual exploitation. Accessing healthcare is a major challenge, with only 2% of migrants with HIV covered by public health insurance, leaving the rest to pay out-of-pocket costs that many cannot afford.
“By extending health insurance to migrants, Peru is not only addressing these barriers but also aligning with global commitments, like the Sustainable Development Goals (SDGs), aimed at eradicating epidemics such as AIDS and TB by 2030”, says Luisa Cabal, UNAIDS Regional Director for Latin America and the Caribbean. “This legislative victory not only marks a turning point in health policy but also sets a precedent for future reforms, ensuring a more inclusive and equitable healthcare system for all.”
Protecting everyone’s rights protects public health.
Region/country
Related






Feature Story
Can this innovation change the way people think about HIV?
16 October 2024
16 October 2024 16 October 2024In 2020, a gay Thai man living with HIV sparked controversy with a Facebook post. He was on antiretroviral therapy and had gotten lab tests to check the level of virus in his blood. Since his viral load was undetectable, he wrote, he was going to stop using condoms.
The public responded with a mix of contempt and disbelief. How could he? So selfish! So reckless! The resulting debate spilled from social media onto national radio and TV.
“There was a huge backlash,” remembered Dr Nittaya Phanuphak, the Executive Director of the Institute of HIV Research and Innovation (IHRI). She was telling the story from IHRI’s sunlit offices to teams from Botswana, Ghana, Ivory Coast, Jamaica, Mozambique, South Africa and Zambia. They’d come to Bangkok as part of a learning exchange coordinated by the Global Partnership for Action to Eliminate all Forms of HIV-related Stigma and Discrimination.
Dr Nittaya said that she and her father, Professor Praphan Phanuphak, thought it was their duty to contribute to the public discourse. While the man’s approach might have been unconventional, the science behind his statement was sound.
They would know. Professor Praphan diagnosed Thailand’s first HIV case in 1985 and dedicated his life to HIV research, service delivery and advocacy. He co-founded the Thai Red Cross AIDS Research Centre which in 2014 conducted cutting-edge research as part of the Opposites Attract Study. Done in Australia, Brazil and Thailand, that study tracked couples in which one person was HIV-negative and the other was living with HIV but had achieved an undetectable viral load through successful HIV treatment. It confirmed that after two years of unprotected sex, there were no cases of HIV transmission between more than 300 couples.
“It’s a scientific fact,” Dr Nittaya said. “For me, I felt like we really needed to do something. We cannot just wait 50 years for this knowledge to gradually seep into Thai society.”
The “knowledge” to which she refers is the concept of undetectable = untransmittable, or U=U for short. Last year the World Health Organization further endorsed the principle, stressing that when a person’s viral load is undetectable there is zero chance of sexual transmission.
“Before, HIV treatment just meant longevity,” said Pan (not his real name), a person living with HIV. “But with U=U, now it is love without fear.”
Within three to six months a person who takes their HIV treatment as prescribed and receives viral load monitoring can confirm that they have achieved an undetectable viral load. This removes the self-stigma associated with having an “infectious” disease. For Thai HIV response stakeholders, this concept can also transform the public’s attitudes about people living with HIV, making it easier for them to live full, happy lives.
“If social perceptions can be brought in line with the reality of HIV treatment, we can remove the stigma around getting an HIV test or diagnosis,” said Eamonn Murphy, Regional Director of UNAIDS Asia Pacific and Eastern Europe Central Asia. “The more supportive the society, the more people we successfully treat and the fewer new infections.”
But for the U=U strategy to be fully utilized, work must be done to dispel myths and bolster confidence in science.
According to UNAIDS Country Director for Thailand, Dr Patchara Benjarattanaporn, a key step in the national process was bringing decision-makers together with relevant stakeholders, including voices from communities.
“They considered both global and local evidence,” she explained. “Now there is consensus about the science. U=U also conveys the message ‘you=you’, affirming that all individuals are equal and that people are more than their HIV status. It emphasizes the importance of ensuring people are fully informed about their options and respecting their right to make choices about their sexual health depending on their realities.”
At the opening ceremony of the eight-country learning exchange, Dr Niti Haetanurak, Department of Disease Control Deputy Director, noted that the U=U concept is a key element of Thailand’s “all of society” strategy to address the prejudice and rights violations people living with HIV face. Thailand has a National Costed Action Plan to Eliminate all forms of HIV-related Stigma and Discrimination. The Ministry of Public Health and Sub-National Committee on AIDS Rights Promotion and Protection under National AIDS Committee coordinate the effort. Community organizations play a leading role.
During the exchange the country teams visited the Service Workers in Group (SWING) Foundation which serves sex workers and IHRI’s Tangerine Clinic which primarily serves transgender people. Both have come up with innovative approaches to ensure groups that usually find it challenging to receive healthcare at state-run facilities can get HIV and sexually transmitted infection (STI) testing and treatment in a friendly environment.
A key strategy is training members of those very communities to provide certain services themselves. They can even start clients on treatment for HIV and some other conditions the same day they are diagnosed. This approach makes it less likely for people to disappear into the shadows after diagnosis, with a high chance of infecting others and eventually becoming ill.
“This community-led health model can be applied to any health condition or population. But this does not really address stigma and discrimination. It just bypasses it by opening up alternative service delivery outlets for people who want to avoid negative experiences elsewhere,” Dr. Nittaya said. “We need to address the heart of the stigma as well. That is why we are working on using U=U as a tool to explore how we can shift attitudes.”
The Bangkok Metropolitan Administration (BMA) is integrating this concept into its work in healthcare settings and the workplace. A masterplan is in the works. One branch of the strategy will tackle employers requiring HIV testing in the pre-employment phase or targeting employees they find out are living with HIV. Another aspect of the approach is the integration U=U into all levels of HIV service delivery and ongoing healthcare worker sensitization. All staff in clinics and hospitals are trained, not just nurses and doctors.
The work doesn’t stop there, though. Describing the Bangkok society as “open”, Dr Tavida Kamolvej, Deputy Governor of Bangkok, said that the whole of society was ready for deeper conversations about inclusion and HIV. But how could these approaches be applied in other countries and cities that are not quite as tolerant or accepting, she was asked.
“If you are confronted with beliefs that might not allow open conversations about HIV, sexuality and sex, you can strategically make it about health literacy, dignity and care for all people. I think this is soft enough to make people aware about health and wellbeing,” Dr Tavida advised.
Click here to learn more about the recent eight-country learning exchange to eliminate all forms of HIV-related stigma and discrimination.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Documents
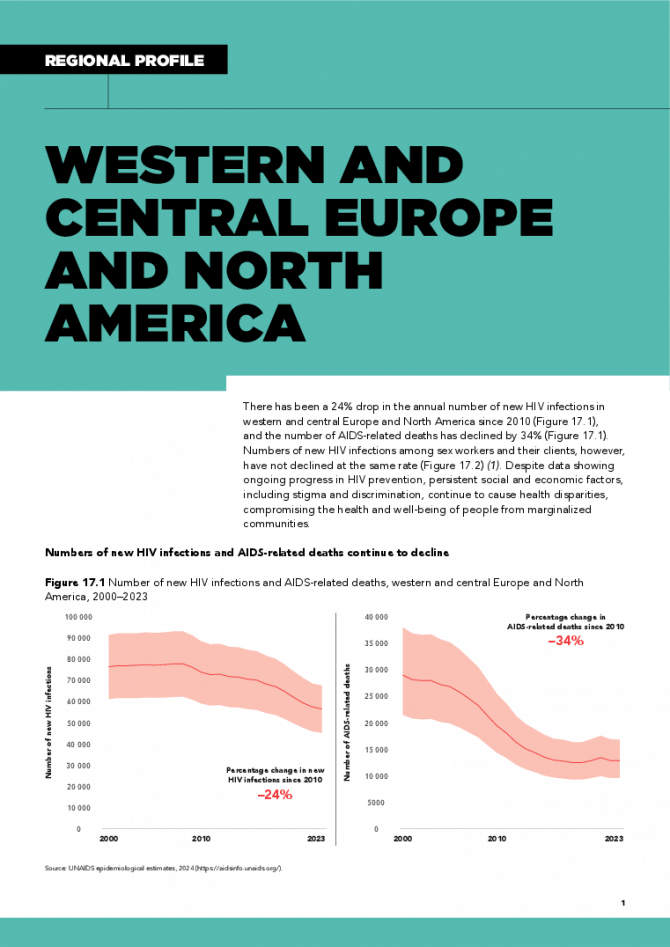
Western and Central Europe and North America regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
There has been a 24% drop in the annual number of new HIV infections in western and central Europe and North America since 2010, and the number of AIDS-related deaths has declined by 34%. Numbers of new HIV infections among sex workers and their clients, however, have not declined at the same rate. Despite data showing ongoing progress in HIV prevention, persistent social and economic factors, including stigma and discrimination, continue to cause health disparities, compromising the health and well-being of people from marginalized communities. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025
Documents
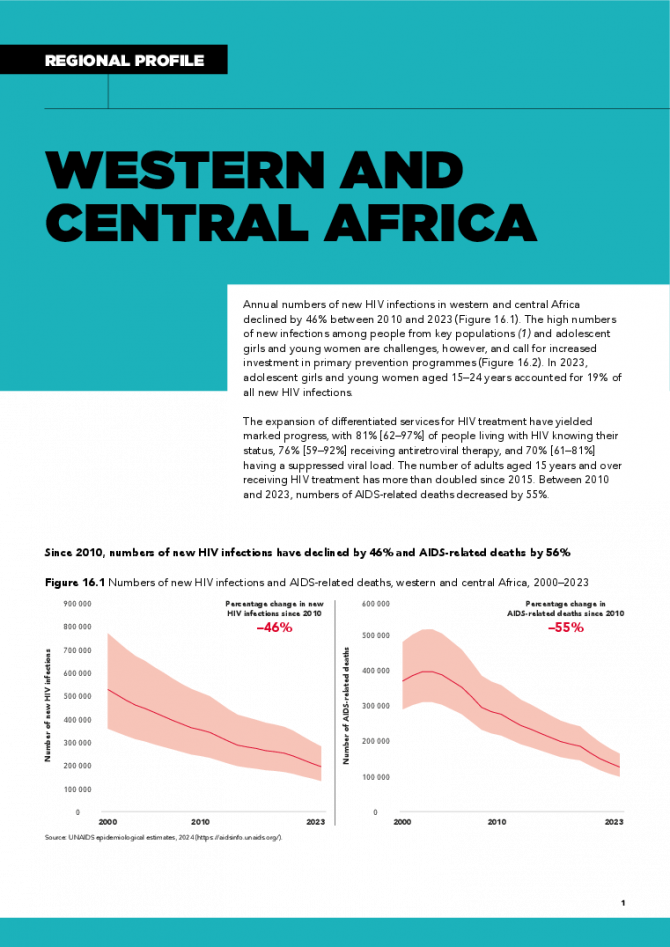
Western and Central Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Annual numbers of new HIV infections in western and central Africa declined by 46% between 2010 and 2023. The high numbers of new infections among people from key populations and adolescent girls and young women are challenges, however, and call for increased investment in primary prevention programmes. In 2023, adolescent girls and young women aged 15–24 years accounted for 19% of all new HIV infections. The expansion of differentiated services for HIV treatment have yielded marked progress, with 81% [62–97%] of people living with HIV knowing their status, 76% [59–92%] receiving antiretroviral therapy, and 70% [61–81%] having a suppressed viral load. The number of adults aged 15 years and over receiving HIV treatment has more than doubled since 2015. Between 2010 and 2023, numbers of AIDS-related deaths decreased by 55%. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
Documents
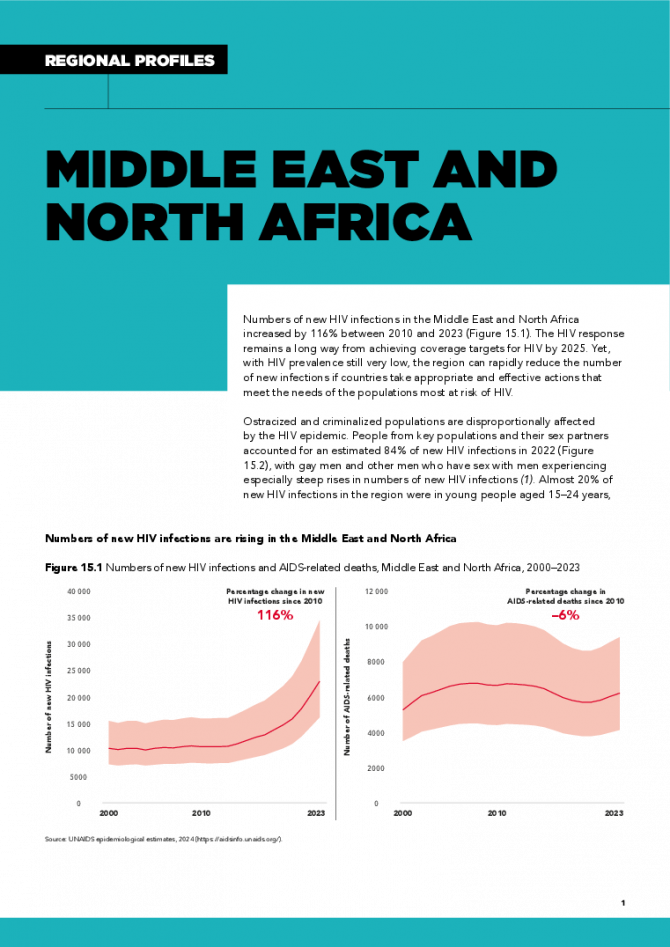
Middle East and North Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Numbers of new HIV infections in the Middle East and North Africa increased by 116% between 2010 and 2023. The HIV response remains a long way from achieving coverage targets for HIV by 2025. Yet, with HIV prevalence still very low, the region can rapidly reduce the number of new infections if countries take appropriate and effective actions that meet the needs of the populations most at risk of HIV. Ostracized and criminalized populations are disproportionally affected by the HIV epidemic. People from key populations and their sex partners accounted for an estimated 84% of new HIV infections in 2022, with gay men and other men who have sex with men experiencing especially steep rises in numbers of new HIV infections. Almost 20% of new HIV infections in the region were in young people aged 15–24 years, the majority of them male (55%). These epidemic patterns underscore the need for scaled-up HIV interventions for people from key populations and especially young people, and for reducing the societal and structural barriers that limit their access to needed services. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
Documents
Latin America — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
The annual number of new HIV infections in Latin America increased by 9% between 2010 and 2023, with eight countries experiencing increases since 2015. In 2022, a significant proportion (66%) of new HIV infections were among people from key populations and their sex partners. In 2022, numbers of new HIV infections were 20% higher than in 2010 among gay men and other men who have sex with men, 42% higher among sex workers, and 19% higher among transgender women. Numbers of AIDS-related deaths have decreased by 28% since 2010 overall, but increased among women in Costa Rica, El Salvador, Mexico, Panama, Paraguay and Peru. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 The critical impact of the PEPFAR funding freeze for HIV across Latin America and the Caribbean
The critical impact of the PEPFAR funding freeze for HIV across Latin America and the Caribbean
19 February 2025
Documents
Eastern and Southern Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
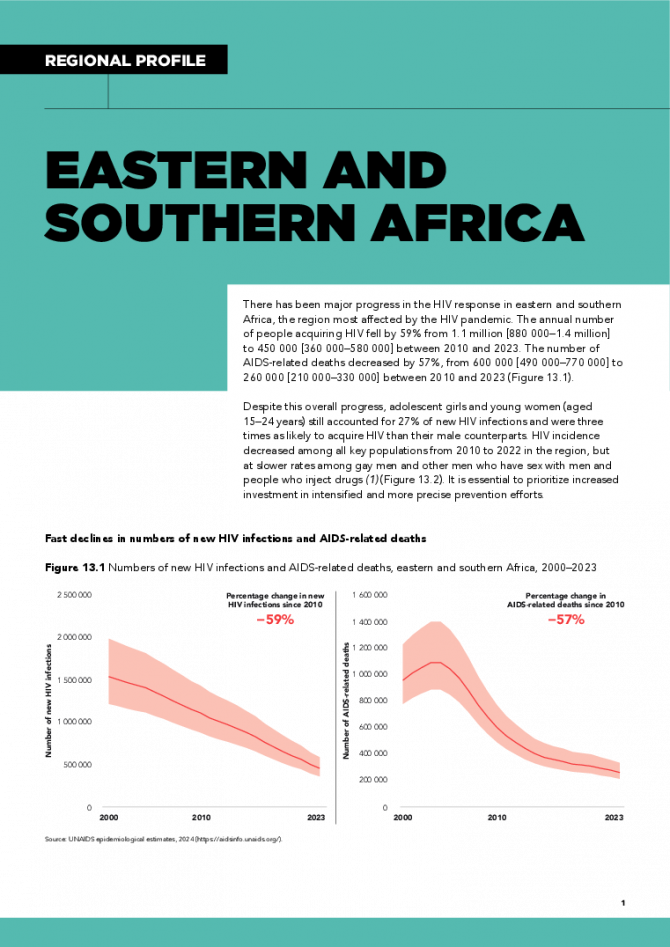
There has been major progress in the HIV response in eastern and southern Africa, the region most affected by the HIV pandemic. The annual number of people acquiring HIV fell by 59% from 1.1 million [880 000–1.4 million] to 450 000 [360 000–580 000] between 2010 and 2023. The number of AIDS-related deaths decreased by 57%, from 600 000 [490 000–770 000] to 260 000 [210 000–330 000] between 2010 and 2023. Despite this overall progress, adolescent girls and young women (aged 15–24 years) still accounted for 27% of new HIV infections and were three times as likely to acquire HIV than their male counterparts. HIV incidence decreased among all key populations from 2010 to 2022 in the region, but at slower rates among gay men and other men who have sex with men and people who inject drugs. It is essential to prioritize increased investment in intensified and more precise prevention efforts. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025
Documents
Eastern Europe and Central Asia regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
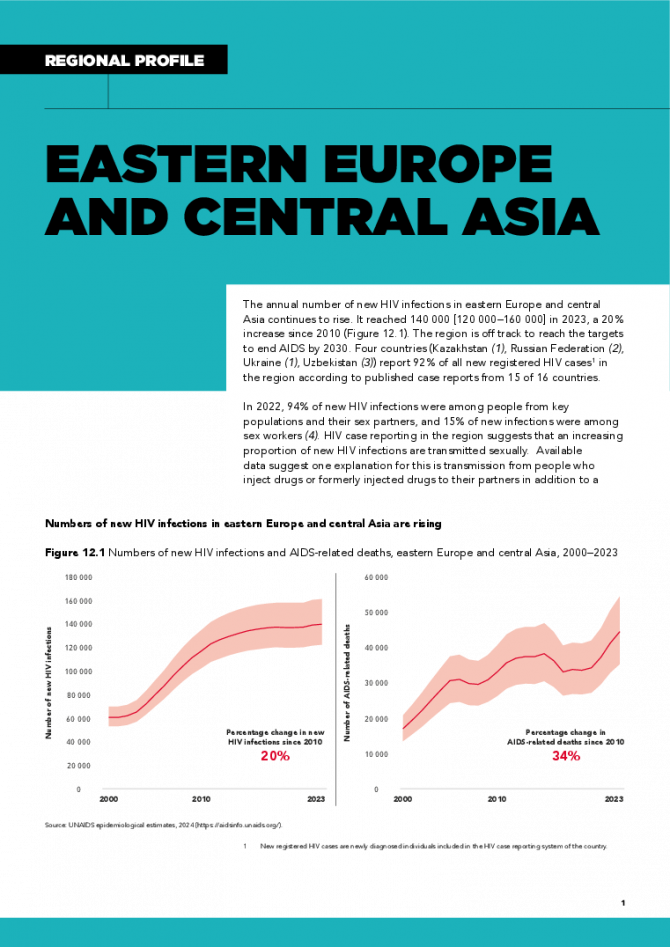
The annual number of new HIV infections in eastern Europe and central Asia continues to rise. It reached 140 000 [120 000–160 000] in 2023, a 20% increase since 2010 . The region is off track to reach the targets to end AIDS by 2030. Four countries (Kazakhstan, Russian Federation, Ukraine, Uzbekistan) report 92% of all new registered HIV cases in the region according to published case reports from 15 of 16 countries. In 2022, 94% of new HIV infections were among people from key populations and their sex partners, and 15% of new infections were among sex workers. HIV case reporting in the region suggests that an increasing proportion of new HIV infections are transmitted sexually. Available data suggest one explanation for this is transmission from people who inject drugs or formerly injected drugs to their partners in addition to a growing recognition of transmission among men who have sex with men. Unsafe drug injecting practices are a key factor in the region’s epidemic, representing 27% of new HIV infections. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
Documents
Caribbean regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
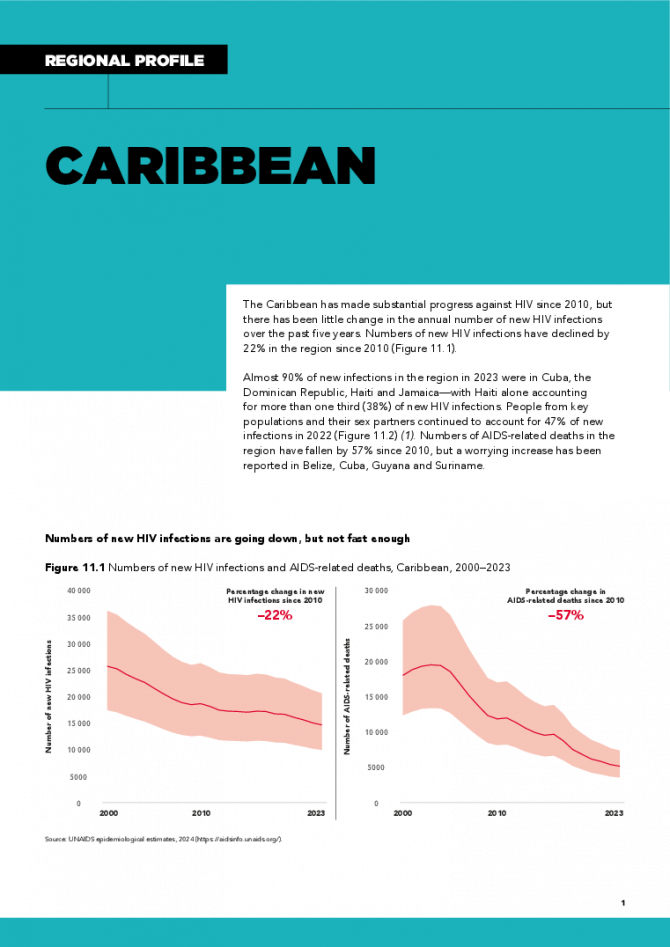
The Caribbean has made substantial progress against HIV since 2010, but there has been little change in the annual number of new HIV infections over the past five years. Numbers of new HIV infections have declined by 22% in the region since 2010. Almost 90% of new infections in the region in 2023 were in Cuba, the Dominican Republic, Haiti and Jamaica—with Haiti alone accounting for more than one third (38%) of new HIV infections. People from key populations and their sex partners continued to account for 47% of new infections in 2022. Numbers of AIDS-related deaths in the region have fallen by 57% since 2010, but a worrying increase has been reported in Belize, Cuba, Guyana and Suriname. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
Documents
Asia and the Pacific regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
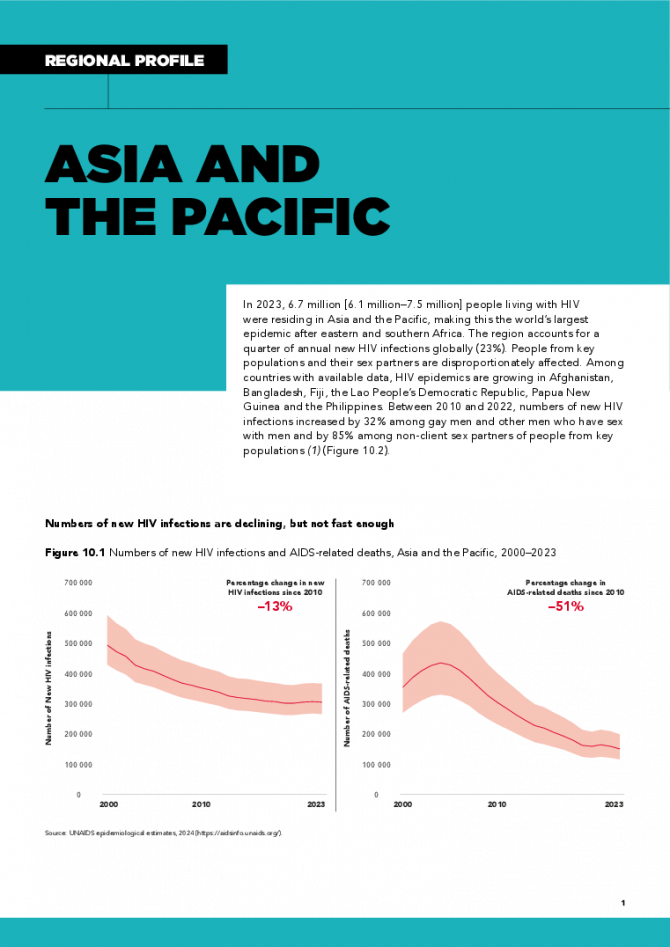
In 2023, 6.7 million [6.1 million–7.5 million] people living with HIV were residing in Asia and the Pacific, making this the world’s largest epidemic after eastern and southern Africa. The region accounts for a quarter of annual new HIV infections globally (23%). People from key populations and their sex partners are disproportionately affected. Among countries with available data, HIV epidemics are growing in Afghanistan, Bangladesh, Fiji, the Lao People’s Democratic Republic, Papua New Guinea and the Philippines. Between 2010 and 2022, numbers of new HIV infections increased by 32% among gay men and other men who have sex with men and by 85% among non-client sex partners of people from key populations. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025