HIV Treatment








Feature Story
South-to-south — Indonesia and Thailand exchange learning on responding to HIV
15 September 2023
15 September 2023 15 September 2023Thailand’s HIV response can provide important learning for other Southeast Asian countries, with the experience of having already reached 90-90-97 in the treatment cascade in 2022, on the way to the achieving the “triple 95s”. The country was first in the region to eliminate mother-to-child HIV transmission. AIDS-related deaths have declined by 65% since 2010. With support from Australia’s Department of Foreign Affairs and Trade (DFAT), UNAIDS helped organise for Thailand to share lessons it has learned in its HIV response with Indonesia through a south-to-south learning exchange mission of Indonesian delegates to Thailand.
On day one, the Indonesian Ministry of Health and Thai Ministry of Public Health delegates discussed the HIV epidemic, trends, and challenges in each country. They shared insights on HIV prevention, treatment and stigma reduction in the HIV response. The following day, the mission team visited community organisations— including the Service Worker in Group Foundation (SWING), a non-governmental organization working for sex worker rights, and the Rainbow Sky Association of Thailand (RSAT), an organization that offers sexual healthcare for men who have sex with men, migrants, people who use drugs, sex workers and transgender people.
Multidisciplinary care is provided in Thailand to people living with HIV and to key populations through community service providers, incorporating certified community counsellors, medical technicians and caseworkers at the community facilities, and through doctors, nurses, pharmacists and laboratory scientists through the telehealth system.
Indonesia’s delegates on the visit highlighted that they had found helpful areas to improve community engagement in their national HIV programme, with a focus on effectively addressing the barriers and limitations in the HIV response that are interlaced with stigma and discrimination across Indonesia.
“We learned how Thailand prioritised zero discrimination, one of which is developing an e-learning curriculum for healthcare workers to minimise stigma and discrimination in healthcare facilities,” said Dr Endang Lukitosari, who heads the National AIDS Programme of Indonesia’s Ministry of Health.
Thailand’s delegates shared experiences from their community complaint support and crisis response system. Health workers, communities and clients can use QR codes at various locations to report rights violations, promoting accountability and coordination between health facilities and community organisations.
The Ministry of Public Health of Thailand noted that community workers are actively involved in the HIV response throughout a robust system of accreditation for both individual community health workers and community organisations. There are health insurance options for all users, including three that can be accessed by migrants. These initiatives help create an enabling environment, led by the government, to connect communities with marginalised groups and tackle issues such as loss to follow-up.
Indonesia’s delegates noted the significance of community mobilisation in the HIV response and envisaged that by putting community in the centre they would reach the most marginalised and underserved groups across different islands and highlands in Indonesia.
“Thailand's comprehensive service delivery inspired me, especially through the Ministry of Public Health's accreditation and certification system for communities. This cooperative mechanism across the government and community stakeholders is the one we haven’t sufficiently addressed in Indonesia. Perhaps by applying this approach, we can minimise the gaps in the treatment cascade by ensuring we leave no one behind”, said Irfani from GWL-INA, Indonesia’s network of men who have sex with men and transgender people.
Over the five days, Indonesian delegates explored public HIV service centres and treatment facilities in Bangkok, Thailand and learned about how efforts of communities and government in HIV prevention and control could be streamlined and coordinated by enhancing the continuum of care and minimising loss to follow up. Notably, Thailand emphasised integrated, One-Stop, services as pivotal for a successful HIV response. Indonesia’s delegates sought a pathway for sustainability in the HIV programme through lessons from the continuity of HIV treatment services in Bangkok, which connects clients with community clinics and public health facilities through referral system and telehealth.
Delegates agreed that this learning mission highlighted key features in efforts to reduce stigma and discrimination, mobilise communities in HIV response, and improve access to quality healthcare by tackling barriers. In addition, the mission underscored efforts to support the delivery of client-centred services for key populations. The debriefing concluded with a commitment to continue the technical partnership on HIV between the two countries.
"I believe Indonesia can do it," said Krittayawan Boonto, UNAIDS Country Director of Indonesia. "Indonesia is in a similar situation to the one Thailand faced a few years ago. Thailand's strategies contributed to getting closer to their goals. I see potential in Indonesia to accelerate progress towards triple 95s. I hope these learnings from Thailand mission can advance the HIV response in Indonesia. UNAIDS Indonesia will keep supporting efforts to end AIDS by 2030."
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Young role models combat HIV stigma in Central Asia
22 June 2023
22 June 2023 22 June 2023Last year, Elina Kruglova made a bold decision. She disclosed her HIV status during the casting of a popular reality TV show in Uzbekistan.
“I disclosed my status right at the casting because the project lasted for several months, and I needed to take medicine daily,” she said. “I made the decision to be honest and mustered up the courage. I thought they wouldn't accept me, but I passed the casting," Ms Kruglova explained.
In her second-year student in the Faculty of Agricultural Economics at Tashkent State Agrarian University in Uzbekistan, she grew up in an orphanage. She was the first child living with HIV in her country to start antiretroviral (ARV) therapy seventeen years ago. Despite facing stigma, she has been taking life-saving medicine daily.
Uzbekistan struggles with HIV-related stigma and discrimination.
According to the recent Multiple Indicator Cluster Survey (MICS) in Uzbekistan, 76% of women aged 15-49 in the country would refuse to purchase vegetables from a vendor living with HIV and would not accept children living with HIV attend school with other children. Prejudice is fuelled by a lack of knowledge; only 14% of women in the same age group possess comprehensive information about HIV. Uzbekistan's HIV cases have steadily risen by 44 % in the last six years (31,088 in 2016 to an estimated 45,000 in 2022.)
Throughout the TV show, Ms Kruglova shared her experiences of being an orphan and living with HIV. Over time she became an inspiration for young people and those living with HIV.
"When the TV episode aired, I started contemplating how people would perceive me, what they would say, and how they would react,” she recalled. “Psychologists were working with us during the project, which made it easier for me to handle the pressure."
To her surprise, people positively reacted when they recognized her on the streets, and she received numerous supportive messages from people living with HIV via Instagram.
"I am grateful for the trust they placed in me " she said.
For her, the Tashkent day-care center for children and families affected by HIV supported by UNICEF and UNAIDS played a crucial role in her life. It provided a safe haven, gave guidance throughout her childhood and teenage years. The center's support group, the professional consultations, and master classes helped her develop practical life skills. She is optimistic about the future and believes that people can change their attitudes towards HIV with the right information and education. In her mind, hiding only makes things worse.
Aida Muravyova knows all about the power of disclosing her HIV status.
She is a 16-year-old school student in Kazakhstan and learned about her HIV status when she was 6 years old. Although advised against disclosing her status at school and extracurricular activities, Aida chose a different path. She shared her HIV status with her classmates in school and took on the role of breaking down the myths and misconceptions surrounding HIV in front of her peers and adults.
“When I was told about my HIV diagnosis, I thought to myself, 'Okay, I have red hair, I have HIV, I take pills... what else?!'"
Ms Muravyova found solace through the Teenergizer Movement, a youth-led initiative supported by the Kazakhstan Government, UNICEF, UNAIDS and other donors. Teenergizer aims to empower young people living with HIV. It created a safe space for young women like her to connect, have fun, and share experiences without shame or stigma. The movement has reached many young people in the country, creating a ripple effect of reliable information and support.
When Teenergizer came along, Ms Muravyova invited classmates to join. "They got valid information, learned with me, and even conducted training sessions,” she said. “The most gratifying part was when one of my classmates' mothers, initially frightened by my HIV status, learned about HIV through her child's participation in Teenergizer.”
Her friend told her that her family had an open conversation, hashed out concerns, and now everything is okay.
Gender assessments conducted in several countries of Central Asia, including Kazakhstan, confirmed that gender inequality, stereotypes, customs and practices increase women’s vulnerability to HIV as well as limit their choices and expose them to socioeconomic and health difficulties.
Ms Muravyova refuses to let her HIV status define her or limit her dreams.. "I have seen many people living with HIV, but never in my field of Electrical and Aerospace Engineering... I want to change that perception and demonstrate that living with HIV can be different, cool, and interesting."
The UNAIDS Regional Policy and Equality Officer in Central Asia, Elena Kiryushina, sees role models like Elina and Aida as well as community networks as key.
“Promoting leadership among adolescent girls and young women, fostering positive masculinities in boys and men, providing care and support to adolescents living with HIV, especially those who lost parents and access to comprehensive sexuality education in and out of schools, and supporting gender-transformative approaches are essential steps to address HIV and gender-related stigma and to build foundation for the gender equality in Central Asia and beyond,” she said.
UNAIDS and partners believe empowering women and girls and challenging cultural norms is crucial to address HIV stigma and ensure equal access to support and health services.
Ms Muravyova has one mantra. “Speak, and don't be afraid!,” she said. “We are together, and together we'll make it through.”
Region/country
Related




Feature Story
Future doctors take active role in HIV response to end AIDS
28 August 2023
28 August 2023 28 August 2023Medical student Anaïs Maillat, 21, joined METIS (Movement of The Students Against Inequalities in Health Access) for a simple reason. The children’s beaming smiles drew her in.
As a member organization of the International Federation of Medical Students Association (IFMSA), the Swiss Medical Students Association (SWIMSA) Switzerland, launched the program CALWHA which works with children and adolescents living with HIV and AIDS in Tanzania.
Ms. Maillat focused on the Mwanza region where the rate of HIV infection is higher than the national average as its project coordinator.
“Our project is currently helping more than 400 children living with HIV and AIDS,” she said. “We organize activity days in hospitals where children and adolescents get check-ups, medicine, a meal, educational activities, and a safe space to play,” she added.
Activity days are held on three Saturdays of each month for children and adolescents aged 0 – 19 years old to improve clinic attendance and treatment adherence. “For many children, the hospital is far, so parents miss work, which has a cost,” Ms. Maillat explained. The project pays for people’s transportation to the hospital and that help allows many children to stay on treatment, according to CALWHA.
Like Ms. Maillat, medical students worldwide are taking an active role in the HIV response in their native countries.
Ana Laura Nascimento, a 21-year-old medical student and member of IFMSA Brazil, became an advocate for sexual and reproductive health rights through Pense Positivo, a project that organizes HIV awareness activities for houseless individuals and sex workers.
During her school years, Ms. Nascimento said she realized there was a clear demand to educate her peers about sex due to sexually transmitted infection (STI) outbreaks. “We organized Testar é Saber (“testing is knowing”), a campaign to encourage students to get tested for HIV, syphilis, hepatitis B and C,” she said.
That led to information sessions at the university including doctors, public health professionals, and the municipality. As a result, the school now offers testing events twice a year.
Ms. Nascimento went on to lead and become a member of IFMSA Brazil’s National Officers for Sexual and Reproductive Health (NORA).
In Malaysia, another NORA leader, Joseph Hamzah Anwar, is a 25-year-old medical student and a member of Society of MMA Medical Students. He became an outreach worker for People Like Us Hang Out (PLUHO) - an LGBTQ organization based in Kuala Lumpur, Malaysia that focuses on mental health.
“I met doctors who are not sensitized to issues that HIV comes with and this discourages clients from seeking treatment,” he said. In his view, the younger generation of doctors need to be aware and knowledgeable, so people stay on HIV treatment and live their lives like any other person.
As members of IFMSA, these future doctors have been organizing activities with communities as part of the organization’s aim to strengthen its involvement in the HIV response. They also seek to educate the public about HIV and AIDS and reduce stigma and discrimination in all healthcare facilities.
Representing more than a million medical students as their members, IFMSA also contributes to the Global Partnership to End All Forms of HIV-Related Stigma and Discrimination and holds a leadership role in The PACT, a global coalition of youth-led organizations advocating for sexual and reproductive health rights.
On August 24, IFMSA, with the International Pharmaceutical Students’ Federation (IPSF) launched a Declaration of Commitment to HIV and AIDS. The Declaration will guide IFMSA and IPSF in their future efforts to contribute to the AIDS response.
All three future doctors hope that the declaration will encourage others to join the global youth movement to end AIDS. “With the activities outlined in the declaration, I believe we are on the right track to end AIDS by 2030,” Mr. Anwar said.
“I truly believe that young people have the potential to unite to end AIDS,” Ms. Maillat said. “We are the generation of unity. Let’s do this. You and me.”
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Documents
Executive summary — The path that ends AIDS: UNAIDS Global AIDS Update 2023
13 July 2023
This report makes clear that there is a path to end AIDS. Taking that path will help ensure preparedness to address other pandemic challenges, and advance progress across the Sustainable Development Goals. The data and real-world examples in the report make it very clear what that path is. It is not a mystery. It is a choice. Some leaders are already following the path—and succeeding. It is inspiring to note that Botswana, Eswatini, Rwanda, the United Republic of Tanzania and Zimbabwe have already achieved the 95–95–95 targets, and at least 16 other countries (including eight in sub-Saharan Africa) are close to doing so. Also available: Additional resources (regional and thematic factsheets) | Annex 1: Progress towards the 2025 targets | Annex 2: Methods | Slide set | Press release | Microsite
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
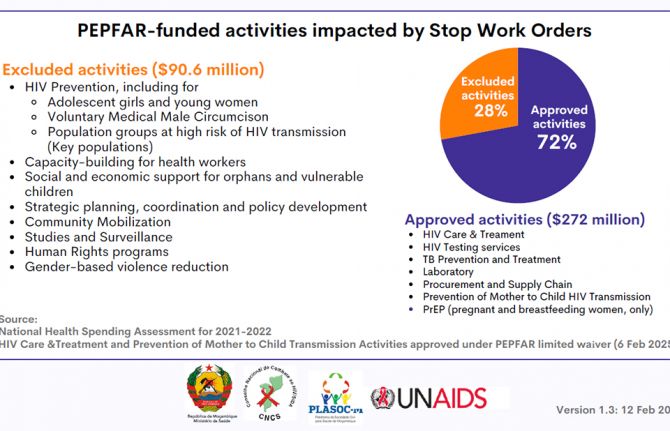
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025


Press Release
New report from UNAIDS shows that AIDS can be ended by 2030 and outlines the path to get there
13 July 2023 13 July 2023GENEVA, 13 July 2023—A new report released today by UNAIDS shows that there is a clear path that ends AIDS. This path will also help prepare for and tackle future pandemics and advance progress towards achieving the Sustainable Development Goals. The report, ‘The Path that Ends AIDS’, contains data and case studies which highlight that ending AIDS is a political and financial choice, and that the countries and leaders who are already following the path are achieving extraordinary results.
Botswana, Eswatini, Rwanda, the United Republic of Tanzania, and Zimbabwe have already achieved the “95-95-95” targets. That means 95% of the people who are living with HIV knowing their HIV status, 95% of the people who know that they are living with HIV being on lifesaving antiretroviral treatment, and 95% of people who are on treatment being virally suppressed. A further 16 other countries, eight of them in sub-Saharan Africa, the region which accounts for 65% of all people living with HIV, are also close to doing so.
“The end of AIDS is an opportunity for a uniquely powerful legacy for today’s leaders,” said Winnie Byanyima, Executive Director of UNAIDS. “They could be remembered by future generations as those who put a stop to the world’s deadliest pandemic. They could save millions of lives and protect the health of everyone. They could show what leadership can do.”
The report highlights that HIV responses succeed when they are anchored in strong political leadership. This means following the data, science, and evidence; tackling the inequalities holding back progress; enabling communities and civil society organizations in their vital role in the response; and ensuring sufficient and sustainable funding.
Progress has been strongest in the countries and regions that have the most financial investments, such as in eastern and southern Africa where new HIV infections have been reduced by 57% since 2010.
Thanks to support for and investment in ending AIDS among children, 82% of pregnant and breastfeeding women living with HIV globally were accessing antiretroviral treatment in 2022, up from 46% in 2010. This has led to a 58% reduction in new HIV infections among children from 2010 to 2022, the lowest number since the 1980’s.
Progress in the HIV response has been strengthened by ensuring that legal and policy frameworks do not undermine human rights, but enable and protect them. Several countries removed harmful laws in 2022 and 2023, including five (Antigua and Barbuda, the Cook Islands, Barbados, Saint Kitts and Nevis, and Singapore) that have decriminalized same-sex sexual relations.
The number of people on antiretroviral treatment worldwide rose almost fourfold, from 7.7 million in 2010 to 29.8 million in 2022.
However, the report also sets out that ending AIDS will not come automatically. AIDS claimed a life every minute in 2022. Around 9.2 million people still miss out on treatment, including 660 000 children living with HIV.
Women and girls are still disproportionately affected, particularly in sub-Saharan Africa. Globally, 4,000 young women and girls became infected with HIV every week in 2022. Only 42% of districts with HIV incidence over 0.3% in sub-Saharan Africa are currently covered with dedicated HIV prevention programmes for adolescent girls and young women.
Almost one quarter (23%) of new HIV infections were in Asia and the Pacific where new infections are rising alarmingly in some countries. Steep increases in new infections are continuing in eastern Europe and central Asia (a rise of 49% since 2010) and in the Middle East and North Africa (a rise of 61% since 2010). These trends are due primarily to a lack of HIV prevention services for marginalized and key populations and the barriers posed by punitive laws and social discrimination.
Funding for HIV also declined in 2022 from both international and domestic sources, falling back to the same level as in 2013. Funding amounted to US$ 20.8 billion in 2022, far short of the US$ 29.3 billion needed by 2025.
There is an opportunity now to end AIDS by increasing political will by investing in a sustainable response to HIV through financing what matters most: evidence-based HIV prevention and treatment, health systems integration, non- discriminatory laws, gender equality, and empowered community networks.
“We are hopeful, but it is not the relaxed optimism that might come if all was heading as it should be. It is, instead, a hope rooted in seeing the opportunity for success, an opportunity that is dependent on action,” said Ms Byanyima. “The facts and figures shared in this report do not show that as a world we are already on the path, they show that we can be. The way is clear.”
In 2022, an estimated:
- 39.0 million people globally were living with HIV
- 29.8 million people were accessing antiretroviral therapy
- 1.3 million people became newly infected with HIV
- 630 000 people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Watch: roundtable discussion
Quote sheet for media
Social media assets
Documents
The path that ends AIDS: UNAIDS Global AIDS Update 2023
13 July 2023
The 2024 global AIDS report The Urgency of Now: AIDS at a Crossroads, released 22 July 2024, is available here.
This report makes clear that there is a path to end AIDS. Taking that path will help ensure preparedness to address other pandemic challenges, and advance progress across the Sustainable Development Goals. The data and real-world examples in the report make it very clear what that path is. It is not a mystery. It is a choice. Some leaders are already following the path—and succeeding. It is inspiring to note that Botswana, Eswatini, Rwanda, the United Republic of Tanzania and Zimbabwe have already achieved the 95–95–95 targets, and at least 16 other countries (including eight in sub-Saharan Africa) are close to doing so. Also available: Additional resources (regional and thematic factsheets) | Annex 1: Progress towards the 2025 targets | Annex 2: Methods | Slide set | Press release | Microsite
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025




Feature Story
How to build stigma-free key population services
23 June 2023
23 June 2023 23 June 2023At his previous factory job, Tom Wang (not his real name) says coworkers gossiped about his sexuality and made fun of him. When he visited a public health facility for an HIV test, the nurse peppered him with questions like “Why do you need it? Have you been sleeping with many partners?”
Thailand is a country famed for its tolerance. It is among the world’s top locations for gender affirming care. Same-sex sexual activity hasn’t been criminalised since 1956. And the policy tide is turning on other key population issues. A 2021 Drug Law allows for harm reduction as opposed to automatic imprisonment, while a bill is in the pipeline to affirm the rights of sex workers. Yet stigma and discrimination persist. In homes, communities, schools, workplaces and—critically—healthcare settings, discriminatory attitudes can take their toll.
“Microaggressions—intentional or unconscious verbal or behavioural slights toward stigmatised groups—can drive people away from HIV prevention and treatment,” noted UNAIDS Regional Human Rights and Law Adviser, Quinten Lataire. “There are evidence-based approaches for measuring and lowering both overt and subtle stigma and discrimination in healthcare settings.”
It was this need for stigma-free services that led to the establishment of the Rainbow Sky Association of Thailand (RSAT). RSAT offers sexual healthcare for men who have sex with men, migrants, people who use drugs, sex workers and transgender people. It also advocates for the full rights and equity of lesbian, gay, bisexual and transgender (LGBT) communities. Tom Wang is amongst the clients who have benefited from their support.
This work is critical if HIV programmes are to reach and retain key population communities. In Thailand, as in the rest of Asia, these groups carry the heaviest HIV burden. Nationally HIV prevalence is 1% for sex workers, 8% for people who use drugs, 11% for transgender women and 12% for men who have sex with men.
A one stop shop for sexual health services
RSAT’s approach demonstrates how programmes can improve outcomes by implementing strategies to affirm and empower clients. They are jointly supported by PEPFAR, USAID, EpiC, the National Health Security Office (NHSO) and Thailand’s Institute of HIV Research and Innovation (IHRI).
There are no depressing charts or drab walls at their five key population clinics. At the Bangkok site the rainbow motif appears on the floors and walls. There are swarms of cut-out butterflies. Signs are either upbeat and multi-coloured or a soothing blue.
Most of the staff are themselves members of key population groups. All staff receive anti-stigma and discrimination training which even addresses the fine point of body language. Nothing about staff’s interactions should make a client feel judged or uncomfortable. The entire team is retrained annually. There is an internal complaint mechanism that allows clients to confidentially flag issues, as well quality assurance staff to ensure Standard Operating Procedures are followed. Every team member signs a confidentiality agreement.
RSAT’s service package includes on-site testing for HIV and other sexually transmitted infections, Hepatitis C, Tuberculosis and Covid-19. For transgender clients they offer hormone level monitoring. Mental health screenings which evaluate for depression, anxiety and stress have been integrated into the HIV service package. Where required, clients are referred for additional mental healthcare.
“Many of our clients engage in chem sex (recreational drug-use during intercourse). Some clients inject meth so we need to provide more than condoms. They also need clean syringes and needles which are part of our harm reduction package,” said Deputy Director, Kao Kierati Panpet.
Pre- and post-test counselling are critical. All counsellors are certified and accredited by the Ministry of Public Health according to Counsellor Supervisor, Sasiprapha Khamthi. Even before receiving HIV test results, clients know that treatment is available. Following a positive test, the counsellors reassure clients that with treatment they can live a normal life, explained Niphon Raina, Care and Counselling Supervisor.
“We also ask what their concerns are and give basic information about how HIV is and is not transmitted, using a picture book so they are clear on the facts,” Care and Counseling Officer, Bussarin Poonvisitkun added.
RSAT keeps a stock of antiretroviral therapy drugs onsite and can initiate new clients’ treatment on the day of diagnosis by giving them one month’s supply. Although HIV care is provided at the Ratchaphiphat Hospital, RSAT is able to dispense right away in accordance with instructions from a hospital doctor, delivered via telemedicine. Clients living with HIV receive help from the care and support team to navigate their next steps, including attending hospital visits.
RSAT also provides pre-exposure prophylaxis or PrEP services with hospital supervision. Mr. Tom Wang explains how this has protected his health: “I decided to get on PrEP because I am changing partners. To me PrEP is another means of protection in case you are intoxicated or the condom breaks. It’s a way to ensure I stay HIV-free.”
A redress mechanism for rights violations
The organisation advocates for structural changes to eliminate stigma and discrimination. For example, they are currently making recommendations for the Gender Recognition Draft Bill.
“But the reality is that policy and legal changes take a lot of time,” said RSAT Director, Tanachai Chaisalee.
While this longer-term work proceeds, a redress mechanism helps clients address current concerns. RSAT is tapped into the Crisis Response System (CRS) initiated by the Ministry of Public Health in collaboration with the Office of the Attorney General, Ministry of Justice. People with complaints about prejudice or rights violations in any sphere can scan a QR code and report their experience. Reports may also be sent via Facebook, email or LINE, Thailand’s answer to WhatsApp. A multi-disciplinary team conducts investigations and works with the client and other stakeholders to help.
The lion’s share of reports made via RSAT come from transwomen (78%) while gay men have lodged 17% of reports. The most common challenges relate to requirements for gender confirming attire, social exclusion (particularly during job application processes) and HIV status.
RSAT’s Human Rights Manger, Watcharawit Waraphattharanon, shares that they have been able to resolve some cases very quickly. For instance, if a person living with HIV is being forced to take an HIV test as a requirement for work, the Attorney General’s office does an emergency intervention.
“We can close these cases within one week,” he said.
“The work of key population-led, community-based organisations like RSAT is critical to reach those who most need HIV services,” UNAIDS Country Director, Patchara Benjarattanaporn stressed. “The Government’s progress in funding Community-led Health Services and building partnerships between these organisations and the public health system puts us on the path to end AIDS.”
A group of journalists visited the Ozone Foundation as part of the UNAIDS, UNDP, APN Plus and USAID/PEPFAR Southeast Asia Regional Workshop on HIV-related Stigma and Discrimination in Bangkok, Thailand on June 8, 2023. Learn more about this novel training
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Press Release
UNAIDS welcomes announcement by Colombian government that will enable people access to the most appropriate HIV treatment for them
12 June 2023 12 June 2023UNAIDS welcomes the issuance of Resolution 881 of 2023 by the Ministry of Health of Colombia, which initiates the administrative procedure to evaluate the existence of reasons of public interest for issuing a compulsory license for dolutegravir (DTG)-based regimens. According to the ministerial resolution, the impact of this measure could mean a significant reduction of more than 80% of DTG’s price.
Dolutegravir (DTG) is an antiretroviral integrase inhibitor, recommended by the World Health Organization (WHO) as a first-line treatment option for people living with the human immunodeficiency virus (HIV). Regarding viral suppression and disease reduction, treatments incorporating DTG-based regimens have demonstrated greater adherence due to their lower incidence of adverse events while presenting enhanced effectiveness, safety, and reduced likelihood of resistance development.
Compulsory licensing is a provision in the World Trade Organization (WTO) Agreement on Trade Related Aspects of Intellectual Property Rights (“TRIPS Agreement”), that enables governments to supply its citizens with generic versions of patented treatments either through domestic production or imports, ensuring drug prices are affordable. WTO Inter-ministerial 2001 Doha Declaration reaffirmed the rights of member states to make use of all flexibilities in the agreement to protect public health, including compulsory licenses, “and the freedom to determine the grounds upon which such licenses are granted.” More recently, in the 2021 Political Declaration of the United Nations General Assembly High-level Meeting on AIDS, countries have committed to make use of TRIPS flexibilities “specifically geared to promoting access to medicines.”
"This resolution is a step forward to provide equal and sustainable access to best HIV treatment options for all people living with HIV in Colombia, nationals and migrants. This action shows the government’s commitment to close the treatment gap with assured quality affordable essential medicines which are easy to take and very well tolerated.”, says Andrea Boccardi, UNAIDS Director for the Andean Countries (Peru, Ecuador, Bolivia, and Colombia. "The government issued national guidelines in 2021, in line with WHO recommendations, but until now high prices of DTG have remained an obstacle to make it widely accessible to people living with HIV in Colombia."
The Colombian League for the Fight against AIDS and the IFARMA Foundation also celebrated the decision from the Colombian government. Both institutions participated on behalf of civil society in the updating of the Clinical Practice Guidelines (CPG) based on scientific evidence for the care of HIV/AIDS infection in adults, pregnant women and adolescents.
"The decision validates past initiatives of civil society in Colombia to achieve greater coverage of simplified treatments with fewer adverse effects at the lowest possible price, while at the same time it will reinvigorate the efforts of community-based organizations in education and promotion of adherence to ARVs, recognizing that structural barriers are factors that facilitate or hinder adherence to antiretroviral treatments", says Jorge Pacheco, Director of the Colombian League for the Fight against AIDS.
“Through this measure Colombia is taking an important step to guarantee people’s access to the most appropriate medication for them in line with international recommendations and commitments”, says Luisa Cabal, UNAIDS Regional Director for Latin America and the Caribbean. "Timely access to effective HIV treatment can save lives, improve health outcomes, enhance the quality of life, and contribute to the overall well-being of individuals living with HIV. This measure shows commitment to the global effort to combat inequalities in access to health."
UNAIDS commends and supports the Ministry of Health for its proactive approach to pursuing public interest and urges all stakeholders to collaborate in implementing Resolution 881 of 2023.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS Latin America and the CaribbeanDaniel de Castro
tel. +507 6998 3175
decastrod@unaids.org
Region/country






Press Release
Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics
06 June 2023 06 June 2023UNAIDS launching group to generate evidence on the inequalities driving pandemics and advocate for the adoption of multisectoral approaches to strengthen the response to AIDS and other pandemics
BRASILIA/GENEVA, 6 June 2023—Brazil is hosting the announcement of the new Global Council on Inequality, AIDS and Pandemics chaired by The First Lady of Namibia, Monica Geingos, the Director of the University College London Institute for Health Equity, Sir Michael Marmot and the Nobel prize winning economist, Joseph E. Stiglitz. Brazil’s Minister of Health, Nísia Trindade, is a founding member.
“I am delighted to host the announcement of the Global Council on Inequality, AIDS and Pandemics. It is time to convert lessons learned into action by reducing the inequalities driving today’s health crises and strengthening pandemic preparedness for the future,” said Ms Trindade, “Brazil is determined to play its part by making the case for increased collaboration and evidence-based policymaking to build more resilient health systems around the world.”
Social and economic inequalities within countries and between them are exacerbating and prolonging pandemics and amplifying their impact amongst the poorest and the most vulnerable. The same intersecting inequalities that drive HIV, COVID-19, MPox and other diseases are leaving countries and communities at risk of future outbreaks and pandemics. But experience shows that there are actions at the global, regional and national levels that can build pandemic responses that reduce rather than exacerbate inequality.
The work of the Global Council will harness essential evidence for policymakers and elevate political attention to the need for action to end inequalities that fuel AIDS and other pandemics. Crucially, it will encourage and support frontline communities to advocate for the policy shifts necessary to fight current pandemics and better prepare for tomorrow’s outbreaks.
“The AIDS response is one of the best examples of how communities experiencing intersecting inequalities can unite to overcome them and save millions of lives,” said UNAIDS Executive Director, Winnie Byanyima who is a member of the Global Council and is in Brazil for the announcement. “A broad movement of people living with and affected by HIV has brought down the price of medicines and diagnostics, strengthened national health responses, enabled the rise of a strong network of community-led organizations and secured the removal of punitive discriminatory laws in many countries. But evidence-based policies and approaches need to be applied everywhere and for everyone and sadly that’s not the case right now.”
Gender-based inequities endanger the health of women around the world. For example, in countries including Ghana, Côte d’Ivoire, and Liberia HIV prevalence for young women is more than 5 times more than young men of the same age—reflecting, in part, economic and education inequality.
“Gender inequality provides fuel to pandemics like AIDS and COVID-19” said the First Lady of Namibia, Monica Geingos. “It increases the vulnerability of women and girls to deadly viruses by limiting access to knowledge, financial resources, and life-choices and undermines their ability to protect themselves and their families. We have to re-imagine pandemic responses that can reduce inequality rather than exacerbate it.”
“Inequalities in access to health and other essential services are largely the result of deliberate policy choices,” said Joseph Stiglitz. “To fight future pandemics, we must learn the lessons of the HIV response and adopt inequality-busting approaches to make the world a healthier, fairer and safer place for everyone.”
Successes and failures in the HIV response provide valuable lessons on how the world can deal with future pandemics. For example, gay men are more likely to be living with HIV. But laws and policies drive the size of the gap. In Malaysia where gay men are criminalized and arrested gay men are 72 times more likely to be infected than other adults; but in Thailand where same-sex relations are legal and community pandemic response is strong, gay men are only 12 times more likely. Viruses cross population groups. These contribute to why Thailand, with lower inequality, is approaching epidemic control while Malaysia is losing ground in the fight against AIDS.
Meanwhile, the issue of inequality extends beyond HIV to other pandemics. Countries with higher income inequality, for example, have experienced greater COVID-19 mortality. At the height of the COVID-19 pandemic, wealthy countries spent billions of dollars on responses but almost half of developing countries were forced to cut health spending, undermining the capacity to fight global pandemics. Several countries in Africa continue reporting significant numbers of MPox deaths during the pandemic, yet the vaccines being used in high-income countries are not available.
Even within countries that have made good progress against HIV, some communities have struggled to benefit from the staggering pace of medical advances. In Brazil, HIV infections are falling dramatically among the white population as access to treatment is widened and new prevention tools such as PrEP are rolled out but HIV infections among the black population are still on the rise.
“Evidence-based strategies to address the social determinants of health are crucial not only for improved health outcomes for the individual but also for building stronger economies and fairer societies,” said Sir Michael Marmot, from Brasilia. “Health is a good marker of how well a society is doing overall. Health equity tells us about societal inequalities.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS BrazilRenato De Paiva Guimaraes
tel. +55 61 99304 2654
depaivaguimaraesr@unaids.org
UNAIDS Latin America and the Caribbean
Daniel de Castro
tel. +507 6998 3175
decastrod@unaids.org
UNAIDS Geneva
Michael Hollingdale
tel. +41 79 500 2119
hollingdalem@unaids.org
Website
Watch
Watch: Jovem de Expressao matters to young people in Ceilandia, Brazil
Region/country




Feature Story
How working with providers of natural and holistic medicine for complementary self-care techniques is helping Nicaragua increase adherence to HIV medicines and reduce new infections
29 May 2023
29 May 2023 29 May 2023Right after taking his HIV treatment each morning, Antonio Hooker prepares a kit of fresh herbs and fruits he has bought at the local market to cross the Bilwa area, a village on the northern Caribbean coast of Nicaragua, as a health promoter for the Association of People Living with HIV (ASONVIHSIDA). He strengthens HIV prevention knowledge among vulnerable groups in his indigenous Miskitu community. He also teaches community leaders and people living with HIV or other health problems to use the power of natural medicine in conjunction with antiretroviral medicines to improve their immune systems.
Antonio is one of the dozens of volunteers and community promoters who have been certified by the Nicaraguan AIDS Commission, the Ministry of Health and the Institute of Natural Medicine and Complementary Therapies through training in "Self-Care in Sexual Reproductive Health and HIV from the Perspective of Natural Medicine".
Since his diagnosis 17 years ago, Antonio has learned the importance of self-care. He now shares his knowledge and training experiences with family members and others living with HIV in remote communities along the Nicaraguan coast.
"The course opened my mind to the importance of natural medicine and traditional practices, such as massage and meditative activities," says the health promoter. "We know these techniques work because we see improvement in our health while seeing progress in adherence to HIV treatment, as well as strengthening social, community networks and relationships within the families of people living with HIV."
The course "Self-care in Sexual Reproductive Health and HIV from the Perspective of Natural and Holistic Medicine" aims to provide guidelines on self-care for people living with HIV or similar conditions and their families. Through the appropriate use of medicinal plants, reflexology (a system of massage used to relieve tension and treat illness, based on the theory that there are reflex points in the feet, hands and head linked to each part of the body) and complementary therapies, such as the practice of the Chinese martial art and system of callisthenics well known as Tai Chi Chuan, which consists in sequences of slow controlled movements.
"The objective is to build skills and abilities among people living with HIV, volunteers and active community members to develop a comprehensive approach to sexual and reproductive health, sexually transmitted infections (STIs) and HIV," explains Dr Enrique Beteta, Nicaragua's Deputy Minister of Health. "It also allows people to access information and linkage to health services at the local level to take care of their health and the well-being of those around them."
The services harnessing natural medicine are complementary, not alternative, to HIV medicines. Indeed, the programmes have helped increase uptake of and adherence to HIV medicines.
Nicaragua’s comprehensive approach and partnership with communities has helped it to advance progress on treatment and prevention. Since 2010, Nicaragua has experienced a 20% decrease in new HIV infections, while in Latin America, new infections have increased by 5% in the same period. About 11 000 people live with HIV in the country, and 90% have been tested and know their positive diagnosis, above regional (82%) and global (85%) rates.
The course offers 84 hours of theoretical and practical training, a quarter of which is focused on Sexual and Reproductive Health and HIV modules. The certification also focuses on putting people at the centre, not only as beneficiaries but also as key protagonists, participating, exercising and demanding access to their rights for equality and equity.
"The course also aims to identify in people the autonomy to make decisions, as transformative agents, in a framework of respect, solidarity and social justice," explains Marie Engel, Director of the UNAIDS Multi-country Office for Guatemala, Honduras and Nicaragua. "Working to eliminate stigma and discrimination is also an important outcome of this initiative."