Press Release
UNAIDS calls on countries to accelerate efforts and close service gaps to end the AIDS epidemic among children and adolescents
22 July 2019 22 July 2019As global 2018 targets are unmet, Start Free, Stay Free, AIDS Free report shows that efforts need to focus on the countries falling behind
GENEVA/MEXICO CITY, 22 July 2019—A new report released today at the 10th IAS Conference on HIV Science in Mexico City, Mexico, shows that the world is lagging behind in its commitment to end the AIDS epidemic among children and adolescents. The report, Start Free, Stay Free, AIDS Free, shows that the pace of progress in reducing new HIV infections among children and expanding access to treatment for children, adolescents and pregnant women living with HIV has slowed significantly and that global targets set for 2018 have been missed, despite important gains being made in some countries.
Globally, around 160 000 children aged 0–14 years became newly infected with HIV in 2018. This is a major decrease from 240 000 new infections in 2010. However, the bold and important target set for 2018 was fewer than 40 000 new infections.
“The failure to reach the 2018 targets to reduce new HIV infections among children and adolescents and to widen access to life-saving treatment is both disappointing and frustrating,” said Gunilla Carlsson, UNAIDS Executive Director, a.i. “We need to act quickly to turn this situation around and honour the commitment to end the AIDS epidemic for the next generation.”
Around 82% of pregnant women living with HIV now have access to antiretroviral medicines. There has been considerable progress among countries in eastern and southern Africa, with more than 90% of pregnant women accessing antiretroviral medicines in Ethiopia, Kenya, Uganda, United Republic of Tanzania and Zimbabwe and 95% or higher in Botswana, Malawi, Mozambique, Namibia and Zambia. This has resulted in a 41% reduction in new HIV infections among children, with remarkable reductions achieved in Botswana (85%), Rwanda (83%), Malawi (76%), Namibia (71%), Zimbabwe (69%) and Uganda (65%) since 2010. The progress made by these countries shows what can be achieved through strong political leadership, rapid policy adoption and concerted efforts by all stakeholders.
The report throws light on where gaps need to be filled to prevent new HIV infections occurring among children. For example, in eastern Africa, 10 000 of 26 000 new HIV infections among children in 2018 were the result of women not being retained on treatment throughout pregnancy and breastfeeding. In southern Africa, 17 000 of 53 000 new infections among children were the result of the mother becoming infected with HIV during pregnancy or breastfeeding. A total of 16 000 new infections could have been averted in southern Africa by retaining mothers on treatment throughout pregnancy and breastfeeding. In western and central Africa, almost 27 000 of the 44 000 new infections could have been averted if their mothers had accessed antiretroviral medicines.
“These new data show that many countries have made important progress toward reaching the 2020 targets, and yet others are lagging significantly behind,” said Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy. “These stark disparities highlight the critical role of political commitment, rapid policy implementation and data-driven investments in accelerating impact.”
Country-level analysis of how mother-to-child transmission of HIV happens can provide vital information to shape national responses.
“Ending AIDS and achieving universal health coverage means leaving no one behind. Yet, too many children and adolescents with HIV are still missing out on the chance to grow up in full health as they can’t access treatment,” said Ren Minghui, the World Health Organization’s Assistant Director-General for Universal Health Coverage/Communicable and Noncommunicable Diseases. “We need to intensify our efforts to and keep our promise to these children.”
Children living with HIV are also being left behind in HIV treatment scale-up and are not being diagnosed and treated early enough. An estimated 940 000 children aged 0–14 years were accessing treatment in 2018, double the number that were on treatment in 2010 but far short of the target of 1.6 million set for 2018.
Children living with HIV are still less likely to have access to HIV treatment than adults living with HIV, a disparity that is widening in some countries, especially in western and central Africa. As a result, the AIDS epidemic is still claiming the lives of many children aged 0–14 years. Children in this age group comprised 5% of all people living with HIV in 23 focus countries but accounted for 15% of people who died from AIDS-related illnesses in those countries in 2018.
"We know how to prevent children from contracting HIV, and we know how to prevent the onset of AIDS in children if they do become infected. They need to be tested and linked to care and treatment as a matter of urgency, but we are missing these opportunities,” said Henrietta Fore, Executive Director of the United Nations Children’s Fund. “Knowing what to do is not enough. We must come together and act with renewed commitment to children and adolescents living with HIV and give them the best chance to survive and thrive.”
For optimal outcomes, children who become infected with HIV must access treatment as quickly as possible. However, in 2018, only 63% of the 1.1 million infants exposed to HIV in the 23 countries worst affected by the epidemic were tested for HIV by the age of two months.
“In many ways, we as a community have settled for a substandard quality of care for children living with HIV,” said Chip Lyons, President and Chief Executive Officer, Elizabeth Glaser Pediatric AIDS Foundation, “We must not allow children to perpetually receive less than the basic standard of care we demand for adults. Especially when the ultimate consequence of that approach is that children and young people are dying of HIV at disproportionally and unacceptably high rates.”
The report also shows that the target of reducing the annual number of new HIV infections among young women and adolescent girls aged 15–24 years to less than 100 000 by 2020 is unlikely to be reached. Globally, new HIV infections among young women and adolescent girls were reduced by 25% between 2010 and 2018, to 310 000. While new HIV infections among adolescent girls and young women aged 15–24 years have declined by over 40% in Botswana, Burundi, Lesotho and South Africa, missing the global target has meant that 6000 adolescent girls and young women are still becoming infected with HIV every week.
The root factors driving the vulnerability of young women and girls to HIV infection are social, structural and behavioural and must be addressed in order to achieve sustainable prevention outcomes. Gender discrimination, gender-based violence, restricted access to opportunities and a lack of tailored services all compound their vulnerability to HIV. Effective responses prioritize an approach combining access to HIV and sexual and reproductive health services with social, structural and behavioural programmes.
“The disparity in viral load suppression rates among adolescents with HIV compared to adults is unacceptable and behoves the global community to advocate for more robust, potent antiretroviral therapy regimens for adolescents as well as to hasten efforts to prevent new infections in this critically vulnerable population,” said Fatima Tsiouris, Deputy Director of the Clinical and Training Unit and Prevention of Mother-to-Child Transmission Lead at ICAP, Columbia University.
The number of voluntary medical male circumcisions undertaken between 2015 and 2018 stood at over 11 million among all age groups, which means that at least 13 million procedures need to be carried out by 2020 in order to reach the target of voluntarily circumcising 25 million men and boys between 2015 and 2020.
UNAIDS and the United States President’s Emergency Plan for AIDS Relief launched the Start Free, Stay Free, AIDS Free framework in 2016 to build on the achievements of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive, which ended in 2014.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Women living with HIV in China unite to confront discrimination
Women living with HIV in China unite to confront discrimination
14 October 2024
Related
 UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day
UNAIDS calls for rights, equality and empowerment for all women and girls on International Women’s Day

06 March 2025
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Update
Only half of HIV-exposed babies are tested for HIV
25 March 2019
25 March 2019 25 March 2019The earlier that a baby who has been born with HIV is diagnosed and starts treatment, the better the outcome.
To diagnose children younger than 18 months of age with HIV requires virological testing, which detects the virus or its components. Serological testing―which tests for HIV antigen and/or antibody generated as part of the immune response to infection―is used for children older than 18 months and adults. Serological testing cannot be used for infants, since it can’t differentiate between HIV antibody produced by the mother and then passed to her baby during the pregnancy, with the baby remaining uninfected, and HIV antibody produced by an HIV-infected baby.
Virological testing is not consistently available in most low- and middle-income countries, however, and when it is available it is often expensive and time-consuming, involving several clinic visits for mothers and infants, the transport of samples to centralized laboratories and potential delays in the return of results.
Globally, only half of infants who are exposed to HIV during pregnancy are tested before eight weeks of age. Since mortality among untreated infants is highest in the first three months of life, prompt diagnosis and linkage to treatment are crucial.
Related information
Related




Feature Story
Kenya: leadership and innovation for results in eliminating mother-to-child transmission of HIV
26 July 2018
26 July 2018 26 July 2018A meeting at the 2018 International AIDS Conference, being held from 23 to 27 July in Amsterdam, Netherlands, has showcased how Kenya is responding to the challenges and opportunities on the way towards validation of the elimination of mother-to-child transmission of HIV in a high-burden context.
Building on the Start Free Stay Free AIDS Free framework, specific attention is being given in Kenya to ensuring access to treatment for children and adolescents living with HIV, while addressing inequities, particularly among adolescent girls and young women.
The participants heard about the role of high-level champions—including community leaders, parents, religious leaders and other relevant stakeholders—highlighting the need for action at all levels, based on robust programmatic data.
Kenya has made significant progress in preventing new HIV infections among children, which fell from an estimated 13 000 in 2010 to 8000 in 2017. This has been possible through programmes such as the mentor mother initiative, which supports and cares for women living with HIV, the mother–baby pair approach, which synchronizes appointments for the mother and the child at the health facility, and audits of every child exposed to HIV in order to identify barriers in accessing health facilities.
The leadership of Margaret Kenyatta, the First Lady of Kenya, and her Beyond Zero Campaign have been instrumental in raising awareness on the importance of services to promote the health of mothers and children, including HIV prevention.
The participants heard, however, that more needs to be done to ensure that progress is equal across the country. Progress has been threatened by recent challenges, such as a health workers strike, which has affected antenatal care and testing coverage, and reduced community support, which has affected demand creation for HIV services.
The participants decided that there was an urgent need to scale up HIV programmes. This would be complemented by innovations in tracking the targets for paediatric and adolescent HIV and accounting for every mother and child. Furthermore, the resilience of the health system needs to be strengthened.
The meeting, held on 24 July, was jointly organized by the Ministry of Health of Kenya, UNAIDS and the Elizabeth Glaser Pediatric AIDS Foundation.
Quotes
“As I reflect on the great gains Kenya has made, what is worrying in the last few years is the widening gap in terms of increased infections among adolescents, especially among young women. The challenges of some of the efforts made, for women especially, mean that our investments in eliminating mother-to-child transmission of HIV may be wiped out in two decades.”
“Every child has the right to be born free from HIV. And every child living with HIV should receive life-saving treatment to stay AIDS-free. And every young person should be supported to stay free from HIV. We cannot leave any child or mother behind.”
“Adopting innovations, such as point-of-care HIV testing with nearly immediate results, is critical to support us young women living with HIV to access the services we need. Programmers and service providers need to listen to our needs and concerns.”
“Progress shown by the data from Homa Bay, Kenya, to reduce new paediatric infections is a powerful message from the highest prevalence county in one of the highest burden countries. If we can do it in Homa Bay, we can do it anywhere.”
Region/country
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025



Press Release
UNAIDS warns that progress is slowing and time is running out to reach the 2020 HIV targets
24 July 2018 24 July 2018New HIV infections are rising in around 50 countries, AIDS-related deaths are not falling fast enough and flat resources are threatening success. Half of all new HIV infections are among key populations and their partners, who are still not getting the services they need
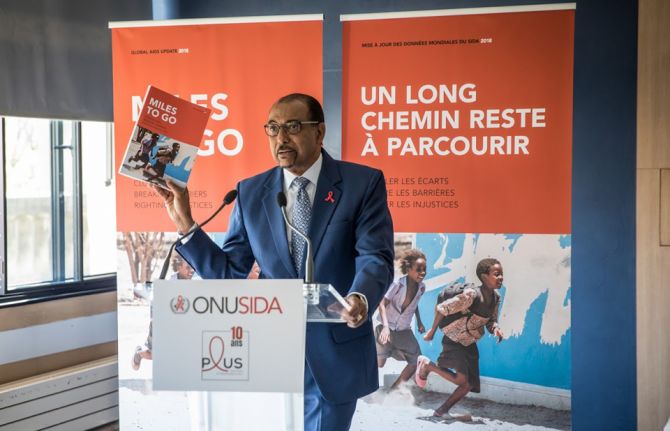
PARIS/GENEVA, 18 July 2018—UNAIDS is issuing countries with a stark wake-up call. In a new report, launched today in Paris, France, at an event co-hosted with Coalition PLUS, UNAIDS warns that the global response to HIV is at a precarious point. At the halfway point to the 2020 targets, the report, Miles to go—closing gaps, breaking barriers, righting injustices, warns that the pace of progress is not matching global ambition. It calls for immediate action to put the world on course to reach critical 2020 targets.
“We are sounding the alarm,” said Michel Sidibé, Executive Director of UNAIDS. “Entire regions are falling behind, the huge gains we made for children are not being sustained, women are still most affected, resources are still not matching political commitments and key populations continue to be ignored. All these elements are halting progress and urgently need to be addressed head-on.”
HIV prevention crisis
Global new HIV infections have declined by just 18% in the past seven years, from 2.2 million in 2010 to 1.8 million in 2017. Although this is nearly half the number of new infections compared to the peak in 1996 (3.4 million), the decline is not quick enough to reach the target of fewer than 500 000 by 2020.
The reduction in new HIV infections has been strongest in the region most affected by HIV, eastern and southern Africa, where new HIV infections have been reduced by 30% since 2010. However, new HIV infections are rising in around 50 countries. In eastern Europe and central Asia the annual number of new HIV infections has doubled, and new HIV infections have increased by more than a quarter in the Middle East and North Africa over the past 20 years.
Treatment scale-up should not be taken for granted
Due to the impact of antiretroviral therapy roll-out, the number of AIDS-related deaths is the lowest this century (940 000), having dropped below 1 million for the first time in 2016. Yet, the current pace of decline is not fast enough to reach the 2020 target of fewer than 500 000 AIDS-related deaths.
In just one year, an additional 2.3 million people were newly accessing treatment. This is the largest annual increase to date, bringing the total number of people on treatment to 21.7 million. Almost 60% of the 36.9 million people living with HIV were on treatment in 2017, an important achievement, but to reach the 30 million target there needs to be an annual increase of 2.8 million people, and there are indications that the rate of scale-up is slowing down.
West and central Africa lagging behind
Just 26% of children and 41% of adults living with HIV had access to treatment in western and central Africa in 2017, compared to 59% of children and 66% of adults in eastern and southern Africa. Since 2010, AIDS-related deaths have fallen by 24% in western and central Africa, compared to a 42% decline in eastern and southern Africa.
Nigeria has more than half (51%) of the HIV burden in the region and there has been little progress in reducing new HIV infections in recent years. New HIV infections declined by only 5% (9000) in seven years (from 179 000 to 170 000) and only one in three people living with HIV is on treatment (33%), although HIV treatment coverage has increased from just 24% two years ago.
Progress for children has slowed
The report shows that the gains made for children are not being sustained. New HIV infections among children have declined by only 8% in the past two years, only half (52%) of all children living with HIV are getting treatment and 110 000 children died of AIDS-related illnesses in 2017. Although 80% of pregnant women living with HIV had access to antiretroviral medicines to prevent transmission of HIV to their child in 2017, an unacceptable 180 000 children acquired HIV during birth or breastfeeding—far away from the target of fewer than 40 000 by the end of 2018.
“One child becoming infected with HIV or one child dying of AIDS is one too many,” said Mr Sidibé. “Ending the AIDS epidemic is not a foregone conclusion and the world needs to heed this wake-up call and kick-start an acceleration plan to reach the targets.”
Key populations account for almost half of all new HIV infections worldwide
The report also shows that key populations are not being considered enough in HIV programming. Key populations and their sexual partners account for 47% of new HIV infections worldwide and 97% of new HIV infections in eastern Europe and central Asia, where one third of new HIV infections are among people who inject drugs.
“The right to health for all is non-negotiable,” said Mr Sidibé. “Sex workers, gay men and other men who have sex with men, prisoners, migrants, refugees and transgender people are more affected by HIV but are still being left out from HIV programmes. More investments are needed in reaching these key populations.”
Half of all sex workers in Eswatini, Lesotho, Malawi, South Africa and Zimbabwe are living with HIV. The risk of acquiring HIV is 13 times higher for female sex workers, 27 times higher among men who have sex with men, 23 times higher among people who inject drugs and 12 times higher for transgender women.
“Communities are echoing UNAIDS’ call,” said Vincent Pelletier, positive leader and Executive Director of Coalition PLUS. “We need universal access to adapted prevention services, and protection from discrimination. We call upon world leaders to match commitments with funding, in both donor and implementing countries.”
Stigma and discrimination persists
Discrimination by health-care workers, law enforcement, teachers, employers, parents, religious leaders and community members is preventing young people, people living with HIV and key populations from accessing HIV prevention, treatment and other sexual and reproductive health services.
Across 19 countries, one in five people living with HIV responding to surveys reported being denied health care and one in five people living with HIV avoided visiting a health facility for fear of stigma or discrimination related to their HIV status. In five of 13 countries with available data, more than 40% of people said they think that children living with HIV should not be able to attend school with children who are HIV-negative.
New agenda needed to stop violence against women
In 2017, around 58% of all new HIV infections among adults more than 15 years old were among women and 6600 young women between the ages of 15 and 24 years became infected with HIV every week. Increased vulnerability to HIV has been linked to violence. More than one in three women worldwide have experienced physical or sexual violence, often at the hands of their intimate partners.
“Inequality, a lack of empowerment and violence against women are human rights violations and are continuing to fuel new HIV infections,” said Mr Sidibé. “We must not let up in our efforts to address and root out harassment, abuse and violence, whether at home, in the community or in the workplace.”
90–90–90 can and must be achieved
There has been progress towards the 90–90–90 targets. Three quarters (75%) of all people living with HIV now know their HIV status; of the people who know their status, 79% were accessing treatment in 2017, and of the people accessing treatment, 81% had supressed viral loads.
Six countries, Botswana, Cambodia, Denmark, Eswatini, Namibia and the Netherlands, have already reached the 90–90–90 targets and seven more countries are on track. The largest gap is in the first 90; in western and central Africa, for example, only 48% of people living with HIV know their status.
A big year for the response to tuberculosis
There have been gains in treating and diagnosing HIV among people with tuberculosis (TB)—around nine out of 10 people with TB who are diagnosed with HIV are on treatment. However, TB is still the biggest killer of people living with HIV and three out of five people starting HIV treatment are not screened, tested or treated for TB. The United Nations High-Level Meeting on Tuberculosis in September 2018 is an opportunity to bolster momentum around reaching the TB/HIV targets.
The cost of inaction
Around US$ 20.6 billion was available for the AIDS response in 2017—a rise of 8% since 2016 and 80% of the 2020 target set by the United Nations General Assembly. However, there were no significant new commitments and as a result the one-year rise in resources is unlikely to continue. Achieving the 2020 targets will only be possible if investments from both donor and domestic sources increase.
Ways forward
From townships in southern Africa to remote villages in the Amazon to mega-cities in Asia, the dozens of innovations contained within the pages of the report show that collaboration between health systems and individual communities can successfully reduce stigma and discrimination and deliver services to the vast majority of the people who need them the most.
These innovative approaches continue to drive the solutions needed to achieve the 2020 targets. When combination HIV prevention—including condoms and voluntary medical male circumcision—is pursued at scale, population-level declines in new HIV infections are achieved. Oral pre-exposure prophylaxis (PrEP) is having an impact, particularly among key populations. Offering HIV testing and counselling to family members and the sexual partners of people diagnosed with HIV has significantly improved testing access.
Eastern and southern Africa has seen significant domestic and international investments coupled with strong political commitment and community engagement and is showing significant progress in achieving the 2020 targets.
“For every challenge there is a solution,” said Mr Sidibé. “It is the responsibility of political leaders, national governments and the international community to make sufficient financial investments and establish the legal and policy environments needed to bring the work of innovators to the global scale. Doing so will create the momentum needed to reach the targets by 2020.”
In 2017, an estimated:
36.9 million [31.1 million–43.9 million] people globally were living with HIV
21.7 million [19.1 million–22.6 million] people were accessing treatment
1.8 million [1.4 million–2.4 million] people became newly infected with HIV
940 000 [670 000–1.3 million] people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
Miles to go—closing gaps, breaking barriers, righting injustices
13 August 2018
The global AIDS response is at a precarious point—partial success in saving lives and stopping new HIV infections is giving way to complacency. At the halfway point to the 2020 targets, the pace of progress is not matching the global ambition. This report is a wake-up call—action now can still put us back on course to reach the 2020 targets.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025


Feature Story
Aisha Muhammadu Buhari to ensure that no child is born with HIV in Nigeria by 2020
26 March 2018
26 March 2018 26 March 2018The wife of the President of Nigeria, Aisha Muhammadu Buhari—the new UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission of HIV and the Promotion of Treatment for Children Living with HIV in Nigeria—has vowed to end mother-to-child transmission of HIV in the country.
“It is with a great sense of responsibility and humility that I accept the honour to serve as a UNAIDS Special Ambassador. I am looking forward to using my voice to help ensure that no child is born with HIV in Nigeria by 2020,” said Ms Buhari, upon commencement of her new role.
Nigeria has one of the highest rates of new HIV infections among children in the world. In 2016, an estimated 37 000 [22 000–56 000] children were newly infected with HIV and 24 000 [14 000–37 000) children died of AIDS-related illnesses. Around 270 000 children [180 000–380 000] children were living with HIV in 2016, and just 32% of pregnant women living with HIV had access to antiretroviral medicines to prevent transmitting the virus to their child.
“I am privileged to announce Aisha Muhammadu Buhari’s acceptance of the appointment as UNAIDS Special Ambassador for Nigeria. The trust and respect that she commands in the country will help us to quicken the pace of stopping new HIV infections among children as well as ensuring treatment for all children living with HIV,” said Michel Sidibé, the Executive Director of UNAIDS.
The appointment of Ms Buhari will reinforce recent efforts to scale up the response to HIV in Nigeria. In December 2016, the President of Nigeria, Muhammadu Buhari, launched a Fast-Track plan that includes using domestic resources to maintain 60 000 people living with HIV on treatment and to ensure that an additional 50 000 people can access treatment each year.
“We are delighted that her excellency has accepted this important role of UNAIDS Special Ambassador. The goal of eliminating mother-to-child transmission of HIV in Nigeria is a laudable one. It must be achieved,” said Pauline Tallen, the Board Chairperson of the National Agency for the Control of AIDS, Nigeria.
Ms Buhari is a passionate advocate for the rights of vulnerable women and girls. During her one-year tenure, she will advocate for increased access to antenatal care services and HIV testing for all pregnant women and their linkage to adequate treatment and care. She will also advocate for an increase in domestic resources for the HIV response at the federal and state levels.
“My three lovely children are all HIV-free because I benefited from prevention of mother-to-child transmission of HIV services. All pregnant women living with HIV in Nigeria deserve children who are born free from the virus, and the new UNAIDS Special Ambassador’s voice can help us make a huge difference. She is now in a strong position to advocate for free prevention of mother-to-child transmission of HIV services in the country,” said Lucy Attah Enyia, a beneficiary of prevention of mother-to-child transmission of HIV services.
A formal ceremony to commemorate Ms Buhari’s acceptance of her appointment will take place during the visit of Mr Sidibé to Abuja, Nigeria, in April 2018.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025
Documents
Start Free Stay Free AIDS Free — 2017 progress report
27 April 2018
This progress report reflects achievements made during the first year of implementation (through December 2016), as countries have taken actions in line with new or existing national strategies. The most recent data on country progress in 2016 are based on country-reported data and country-developed models using Spectrum software that were reported to UNAIDS in 2017.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025