Press Release
Six Caribbean territories and states eliminate mother-to-child transmission of HIV and syphilis
01 December 2017 01 December 2017The World Health Organization has validated Anguilla, Antigua and Barbuda, Bermuda, Cayman Islands, Montserrat, and Saint Kitts and Nevis as achieving dual elimination
Saint Kitts and Nevis/ Geneva, December 1, 2017 - Anguilla, Antigua and Barbuda, Bermuda, Cayman Islands, Montserrat and Saint Kitts and Nevis were today certified by the World Health Organization (WHO) as having eliminated mother-to-child transmission of HIV and syphilis.
“This elimination is the result of our strong political commitment to public health and of making the health of mothers, children and families a regional priority,” said Timothy Harris, Prime Minister of St. Kitts and Nevis. Over the last six years the Caribbean has succeeded in reducing new HIV infections in children by more than half. “This is an amazing achievement given the high rates of HIV in the past, and we intend to improve on this success story even more in the future.”
Carissa F. Etienne, Director of the Pan American Health Organization (PAHO) and Regional Director for the Americas of WHO, said “This elimination is a remarkable achievement that puts the Americas at the forefront of the global effort to ensure that no child is born with HIV or congenital syphilis”. “With political commitment, stronger health systems, and timely prevention, diagnosis and treatment, we can achieve great changes,” she added.
“UNAIDS congratulates the six states and territories on this important achievement,” said Michel Sidibé, Executive Director of UNAIDS. “All countries should follow their example and ensure that every child has an HIV-free start to his or her life.”
In 2015, Cuba, another Caribbean island, became the first country in the world to receive validation from WHO for having achieved elimination of mother-to-child transmission of HIV and syphilis. Subsequently, Thailand and Belarus were also validated as having achieved dual elimination, while Armenia received validation of its elimination of mother-to-child transmission of HIV and the Republic of Moldova was validated for the elimination of congenital syphilis.
Since the launch in 2010 of the Regional Initiative for the Elimination of Mother-to-Child Transmission of HIV and Congenital Syphilis in Latin America and the Caribbean—coordinated by PAHO and the United Nations Children’s Fund (UNICEF), with support from other regional partners—new HIV infections have been reduced in the Caribbean by more than half among children, from 1800 in 2010 to fewer than a thousand in 2016. Reported cases of congenital syphilis, meanwhile, remain below the goal of having no more than 50 cases per 100,000 live births, although they have not declined since 2010, and it is likely there is underreporting of cases.
“The elimination of mother-to-child transmission of HIV and syphilis is not just a dream; it’s an achievable goal,” said Maria Cristina Perceval, UNICEF Regional Director for Latin America and the Caribbean. “Today we can say we are closer to ensuring an AIDS-free generation”.
In the Caribbean as of 2016, 74% of pregnant women living with HIV, 64% more than in 2010, had access to antiretroviral therapy to protect their health and significantly reduce the possibility of transmitting the virus to their children during pregnancy, delivery or breastfeeding. The increased access to treatment contributed to a 52% reduction in the rate of mother-to-child transmission of HIV between 2010 and 2016, which is now at 9%, still higher than the target of 2%.
Other changes in the health sector that have contributed to this progress include intensive participation by both the public and private health sectors, led by the ministries of health, in the implementation of comprehensive maternal and child health services, with an emphasis on universal coverage and quality antenatal and prenatal care. They also include expanded testing to ensure early detection and immediate treatment for both HIV and syphilis, laboratory networks of guaranteed quality in accordance with international standards and the implementation of essential measures to guarantee the human rights of women living with HIV.
“The validation for the elimination of mother-to-child transmission of HIV and syphilis sends a strong message that the Caribbean is making remarkable inroads to achieving the goal of an AIDS-free generation and the achievement directly aligns with achieving our vision and objectives,” said Dereck Springer, Director of the Pan Caribbean Partnership against HIV and AIDS. “The spread of the disease from mothers to children is being halted, but elimination status must be maintained and other Caribbean countries must strengthen their services with the goal of receiving validation from WHO,” he added.
The elimination of mother-to-child transmission of HIV and syphilis is an important milestone for ending AIDS and sexually transmitted infections as public health threats by 2030, commitments endorsed by the United Nations General Assembly and by the World Health Assembly. Other PAHO Member States in the Caribbean are participating in the formal validation process, and it is expected that more will be recognized for their achievements in 2018.
Spotlight on HIV prevention
This week, PAHO and UNAIDS launched their first joint report on HIV prevention in the Americas, entitled HIV Prevention in the Spotlight: A Health Sector Analysis in Latin America and the Caribbean. The report shows that the number of new HIV infections among adults remained stable in Latin America and the Caribbean between 2010 and 2016, at about 120,000 new HIV infections annually. The report urges countries to step up the implementation of a comprehensive package of interventions to prevent new HIV infections for key populations, so as to end the AIDS epidemic as a public health threat by 2030.
Among the report’s specific recommendations is expanded access to HIV self-testing and diagnosis of other sexually transmitted infections, the provision of pre- and post-exposure prophylaxis as recommended by WHO, treatment for all people living with HIV, and eliminating discrimination.
HIV and syphilis in the Caribbean in 2016*
- 310 000 [280 000–350 000] people living with HIV.
- 64% [51–74%] of people living with HIV know their status.
- 81% [64– >85%] of people diagnosed with HIV on antiretroviral therapy.
- 67% [53–77%] of people on antiretroviral therapy have a suppressed viral load.
- 18 000 [15 000–22 000] new HIV infections.
- 9400 [7300–12 000] AIDS-related deaths.
- 1.25 million live births in 2014 in 31 Caribbean countries.
- 10 000 [8700–12 000] children up to 14 years of age living with HIV, 29% less than in 2010.
- <1000 [<1000–1000] new HIV infections among children up to 14 years old in 2016, more than 52% less than in 2010.
- 11 000 [9000–13 000] new HIV infections prevented among children up to 14 years old from 2010 to 2016.
- 97% of women attend at least one antenatal check-up, and 94% of deliveries took place in hospitals in 2016.
- 78% of pregnant women were tested for HIV in 2016, 35% more than in 2010.
- 74% [65–84%] of pregnant women living with HIV are on antiretroviral therapy, a 64% increase since 2010.
- 9% rate of mother-to-child transmission of HIV, 52% less than in 2010.
- 96% coverage of testing for syphilis among pregnant women who had at least one prenatal visit, stable since 2010.
- 80% of pregnant women diagnosed with syphilis received adequate treatment, stable since 2010.
- 1 case of congenital syphilis every 10 000 live births in 2016 according to data from 21 countries, stable since 2010.
* Source: Global Monitoring of AIDS 2017, UNAIDS and data directly reported by countries to PAHO.
WHO validation process
The validation process begins with a request from a country to PAHO for the validation of the elimination of mother-to-child transmission of HIV and syphilis. Then, an independent Regional Validation Committee is formed to carry forward the process, using the global validation standards recommended by WHO.
In the case of these Caribbean states and territories, the members of the regional committee were experts from 10 countries of the Americas, who reviewed the reports of each state and carried out virtual and in situ evaluations in four key areas: health programmes and services, data and information systems, laboratory quality and human rights, gender equality and community participation.
On the recommendation of the regional committee, the Global Validation Advisory Committee conducted a second review and recommended to the Director-General of WHO the validation of Anguilla, Antigua and Barbuda, Bermuda, Cayman Islands, Montserrat and Saint Kitts and Nevis for the achievement of the elimination of mother-to-child transmission of HIV and syphilis as a public health threat.
###
The Pan American Health Organization (PAHO) works with the countries of the Americas to improve the health and quality of life of their peoples. Founded in 1902, it is the oldest international public health organization in the world. It acts as the regional office for the Americas of the WHO and is the specialized health agency of the inter-American system.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Note to editors:
The indicators required by PAHO / WHO for validation in the Americas include:
Impact indicators—must be reached for at least two consecutive years:
- 30 cases or fewer of new perinatal HIV infections per 100,000 live births; and
- 50 cases or fewer of congenital syphilis per 100,000 live births; and
- 2% or below rate of mother-to-child transmission of HIV.
Process indicators—must be achieved for at least two consecutive years:
- 95% or more of all pregnant women should receive at least one antenatal care visit.
- 95% or more of pregnant women living with HIV tested for the virus.
- 95% or more of pregnant women attending prenatal care screened for syphilis.
- 95% or more of pregnant women diagnosed with HIV or syphilis receive adequate treatment.
The term validation is used to attest that a country has successfully achieved the indicators (regional and global targets established for validation) to eliminate mother-to-child transmission of HIV and syphilis at a specific point in time and demonstrate a health system strong enough to maintain the gains.
Region/country






Update
Naomi Watts visits Nyumbani Children’s Home to learn about paediatric HIV treatment
12 July 2017
12 July 2017 12 July 2017Naomi Watts, UNAIDS Goodwill Ambassador, visited Nyumbani Children’s Home in Kenya on 11 July to learn about Kenya’s prevention of mother-to-child transmission of HIV programme and the work done in the home to care for children living with HIV.
In the space of just a few years, as the result of a strong partnership between political leadership, programme implementers and the community, new HIV infections among children aged 0–14 years in Kenya have fallen from 12 000 in 2013 to 6600 in 2015. In June, under the leadership of the First Lady, Margaret Kenyatta, Kenya launched a new framework to accelerate the country’s efforts towards elimination of mother-to-child transmission of HIV and syphilis. The framework calls for the elimination of stigma and discrimination and the creation of an environment that empowers women living with HIV.
Nyumbani Children’s Home opened in 1992 and is currently home to 124 children living with HIV. The home provides nutritional, medical, psychosocial and spiritual care to the children and to the surrounding community, providing a place of safety in Nairobi for abandoned children living with HIV. In addition, the organization has a community- based programme that supports more than 3100 children living with HIV who reside in the informal settlements of Nairobi and 1000 orphans in Nyumbani villages.
Mss Watts and her two sons visited several facilities in the home, including its state-of-art laboratory equipped to undertake early infant diagnosis and viral load testing. Ms Watts congratulated Nyumbani Children’s Home for the impact it makes on a daily basis in the lives of so many remarkable and empowered children. She committed to continue to create awareness of the need to ensure that children living with HIV remain AIDS-free.
Quotes
"Today I have witnessed incredible successes. The Nyumbani children are a living example of the impact of antiretroviral treatment on the health and well-being of children living with HIV.”
"We must counter stigma and discrimination, in particular against children living with HIV. They deserve our love and compassion to remain AIDS free.”
“I observe on a daily basis the power of antiretroviral treatment. Our children are happy, healthy and in school. Together we can make sure that children living with HIV reach their full potential.”
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025


Update
Armenia receives award for elimination of mother-to-child transmission of HIV
06 July 2017
06 July 2017 06 July 2017Armenia has been recognized by the United Nations for its elimination of mother-to-child transmission of HIV programme. The 2017 United Nations Public Service Awards saw Armenia win first prize in the Innovation and Excellence in Delivering Health Services category.
The award was made at the 2017 United Nations Public Service Forum, held in The Hague, Netherlands, on 22 and 23 June to debate how innovative policies can be fostered to implement the 2030 Agenda for Sustainable Development even when resources are scarce, objectives are highly ambitious and interests are disparate.
In 2016, Armenia was one of only four countries to be validated by the World Health Organization for eliminating mother-to-child transmission of HIV.
Quotes
“Maternal and child health protection, including healthy infants born to HIV-positive mothers, are among the major priorities for the health-care system of Armenia. Armenia’s success on elimination of mother-to-child transmission of HIV brings it one step closer to achieving the Sustainable Development Goal of ensuring healthy lives and promoting well-being for all at all ages.”
“This award is a clear signal that Armenia can be among the first countries in eastern Europe and central Asia to achieve an AIDS-free generation and to end the AIDS epidemic.”
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025
















Update
Stay Free proving a challenge in many countries
24 May 2017
24 May 2017 24 May 2017UNAIDS and the United States President’s Emergency Plan for AIDS Relief have convened a ministerial meeting to review progress in implementing the Start Free, Stay Free, AIDS Free framework on 24 May. The meeting, sponsored by Lesotho, Malawi, Swaziland, and the World Health Organization was held on the sidelines of the 70th World Health Assembly.
The First Lady of Namibia and UNAIDS Special Ambassador for Young Women and Adolescent girls, Monica Geingos, was a special guest at the meeting. She gave an inspiring keynote speech that set the tone of the meeting, in which she emphasized the need to change the way we speak to young people and train the people who are educating them on sex and HIV, including teachers and grandparents.
“We’ve done so much great work on the Start Free, but there’s something wrong on the Stay Free,” said the First Lady. “Young people have changed the way they talk and we need to speak their language so we can reach them in a way they can relate to.”
Florence Anam, from the International Community of Women Living with HIV, shared her own personal experience and talked about health systems that are ill-equipped to deal with teenagers and teenage pregnancy. She said, “We need to invest in networks of women living with HIV and build our capacity to contribute to and engage with actions that impact on our lives.” She also talked about the need to involve men and create initiatives for greater male engagement to promote shared responsibility.
The common theme of the meeting was the agreement that excellent work has been done to stop new HIV infections among children, but that adolescents have been left behind and a new approach is needed to reach and engage them in staying free from HIV.
“We will never be able to control and end this epidemic if we don’t think ahead,” said Michel Sidibé, Executive Director of UNAIDS. “This means not just thinking about starting free and giving babies a chance to be born free, but also making sure that they stay free.”
“We are nothing without the scientific evidence, but it cannot be translated into programmes without communities and political leadership,” said Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy.
Ministers of health and representatives of Cameroon, the Democratic Republic of the Congo, Kenya, Lesotho, Malawi, Mali, Namibia, Nigeria, Swaziland, Togo and Zimbabwe joined the Executive Director of UNAIDS and the United States Global AIDS Coordinator to look at some of the challenges they are facing in scaling up HIV prevention and treatment, as well as to share some of the success stories from their respective countries.
They were asked to describe what was the one most important action they were initiating under the Start Free, Stay Free, AIDS Free agenda. Below are some of the highlights of their responses.
Quotes
“One of the interesting approaches we took in the Democratic Republic of the Congo was a programme where the distribution of antiretroviral medicine was done by people living with HIV. This helped decrease stigma, give easier and faster access to treatment and increase adherence. It also freed up health facilities and gave health workers an opportunity to concentrate on new patients and cases needing specialist medical attention.”
“There is an urgency to act responsibly towards ensuring babies are born free of HIV and protecting those babies into adolescence. It's not a matter of programming, but taking the responsibility to make the right choices.”
“Today we have implemented up to 99% of antiretroviral medicine coverage among pregnant women living with HIV but as a minister I’m not happy with 99%. The best measure is the number of children born without HIV. We want the entire country to be HIV-free.”
“Start Free is the order of the day. We have mobilized leaders, empowered young people and focused on reaching pregnant women. Stay Free is the challenge. We have to change the way we speak to young people and make sure that our HIV prevention programmes are led by young people.”
“In Zimbabwe, we have looked at two things: prevention and treatment. If you want to do treatment, do treatment, it’s very good. But if you don’t turn the tap off on new infections, then you have a problem. This is why for Zimbabwe its prevention, prevention, prevention.”
“We have raised political awareness, scaled up HIV testing, but we have a problem of stock-outs and loss to follow-up for which we would like to find solutions.”
“We need to work together and to be accountable, we need all partners, including non-governmental partners, to work hand in hand. We can't do it without our partners—it’s the only way we can accelerate our response.”
“We have mobilized both financial and human resources. Our programmes are being driven by community health workers. They are our solution to our engagement with communities.”
“We have made a certain amount of progress and our objective is to continue along this path. It is important that we don’t let our guard down. We also want to recognize the accomplishments made by our partners, particularly UNAIDS. Alone we go fast, but together we go far.”
“We have a three-month antiretroviral medicine policy because we found that people were not adhering to their medicines because they were taking so much time off work to go time and again to the health centres. And now we are considering going up to a six-month regime. We are looking into how this will work for us.”
“We are expanding our universal health coverage and one of the key interventions is preventing mother-to-child transmission. As part of this we have procured supplies of rapid test kits and first-line drugs for HIV treatment. HIV is also now part of the school curriculum.”
“We need to simplify integrated services for prevention of mother-to-child transmission of HIV and tuberculosis, we need to pay attention to the needs of children—there are too many late diagnosis, and we urgently need age-appropriate formulas to be made available.”

Feature Story
Preventing mother-to-child transmission of HIV in coffee producing areas of Guatemala
08 December 2016
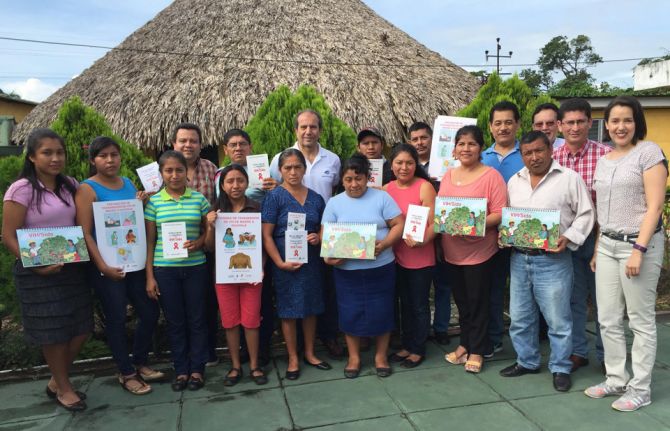
08 December 2016 08 December 2016Preventing mother-to-child transmission of HIV remains one of the major challenges of the AIDS response in Guatemala. In 2015, testing coverage for HIV among pregnant women was 42%. Now, the International Labour Organization (ILO) has teamed up with the Coffee Foundation for Rural Development (Funcafé), the national coffee association, the national AIDS programme and other United Nations agencies, such as UNAIDS and the United Nations Children’s Fund, to promote access to HIV testing, treatment and prevention programmes among women who take up work on plantations during the coffee cutting season.
Seasonal workers employed on coffee plantations often have limited information about HIV and other health issues and restricted access to HIV care and support services. There is also the additional challenge of high levels of mobility and migration among plantation workers. The new programme leverages the network of 16 community health centres established by Funcafé in coffee producing areas of the country’s highlands to provide information related to the prevention of mother-to-child transmission of HIV and to promote the uptake of HIV testing and treatment services for pregnant women.
The project aims to diagnose pregnant women living with HIV and refer them to the official health system for further tests to confirm their status and to start antiretroviral treatment. ILO and its partners provide technical support to train community health workers on providing prevention of mother-to-child transmission of HIV services, bringing HIV treatment and prevention services closer to the people who need them and increasing testing and treatment coverage among pregnant women.
“This is an innovative initiative aimed at strengthening women’s access to prevention of mother-to-child transmission of HIV services by linking the community health system and the national health system and by promoting a multisectoral partnership between the private sector, the Ministry of Health and international partners, with the active participation of communities,” says Ricardo Garcia, UNAIDS Country Director in Guatemala.
Among other aspects, the initiative seeks to train community midwives on HIV prevention and prevention of mother-to-child transmission of HIV on coffee plantations. Midwives play an important role in rural areas as an entry point for pregnant women into the health system. The joint project also aims to raise awareness about HIV prevention and gender equality among male coffee workers and men living in rural areas.
“Workplace settings are an opportunity to provide access to information about HIV prevention tools as well as to promote health, not only among our employees and their families, but in the communities in which we operate, benefiting the entire population,” explains Mynor Maldonado, the Executive Director of Funcafé.
The initiative is part of a wider programme that ILO and UNAIDS have been implementing since 2013. ILO and its partners are exploring similar initiatives with other agribusiness sectors.
Region/country
Related




Update
Ministerial dialogue on Start Free Stay Free AIDS Free
05 December 2016
05 December 2016 05 December 2016On 5 December, health ministers from nine African countries joined UNAIDS, the United States President’s Emergency Plan for AIDS Relief (PEPFAR) and other development partners in Geneva, Switzerland, to demonstrate their leadership in ending AIDS among adolescents and preventing new HIV infections among children by 2020.
The nine ministers attending were:
- Isaac Adewole, Minister of Health, Nigeria.
- Abdourahmane Diallo, Minister of Health, Guinea.
- Bernard Haufiku, Minister of Health and Social Services, Namibia.
- Peter Kumpalume, Minister of Health, Malawi.
- Mantoetsi Liteboho Mohatonyane, Vice-Minister of Health, Lesotho.
- Sarah A. Opendi, Minister of State for Health, General Duties, Uganda.
- Salomon Nguema Owono, Minister of Health and Social Welfare, Equatorial Guinea.
- Mouzinho Saíde, Vice-Minister of Health, Mozambique.
- Sibongile Simelane, Minister of Health, Swaziland.
Representatives of the Governments of Cameroon, Kenya and Zimbabwe also participated.
The meeting, co-convened by Michel Sidibé, UNAIDS Executive Director, and Deborah Birx, United States Global Aids Coordinator and Special Representative for Global Health Diplomacy, aimed to identify the opportunities in, and possible barriers to, implementing the new Start Free, Stay Free, AIDS Free framework. The framework builds on the legacy of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive—which contributed to a 60% reduction in new HIV infections among children in the 21 high-burden Global Plan countries between 2009 and 2015—to accelerate the end of the AIDS epidemic among children, adolescents and young women.
The meeting participants included Jean-Marie Ehouzou, African Union Ambassador to the United Nations in Geneva, and Mark Dybul, Executive Director of the Global Fund to Fight AIDS, Tuberculosis and Malaria. The participants also included key technical partners, including representatives of the United Nations Children’s Fund, the World Health Organization and the Elizabeth Glaser Pediatric AIDS Foundation, as well as representatives of civil society organizations, including Angeline Chiwetani, from the Widows Fountain of Life, Zimbabwe, and faith-based organizations.
The need to assess gaps and challenges at the country level, so that domestic and international resources can be identified to overcome the challenges, was stressed. The ministers were encouraged to demonstrate their continued commitment as champions of Start Free, Stay Free, AIDS Free, mobilize resources and scale up effective responses.
Start Free Stay Free AIDS Free focuses on accelerating progress towards ending new HIV infections among children, finding and treating children, adolescents and mothers living with HIV and preventing the cycle of new HIV infections among adolescents and young women. Building momentum to implement the framework will be critical to empowering high-profile advocates, developing linkages between the global framework, national strategies and community agendas and ending AIDS as a public health threat by 2030.
Resources
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Documents
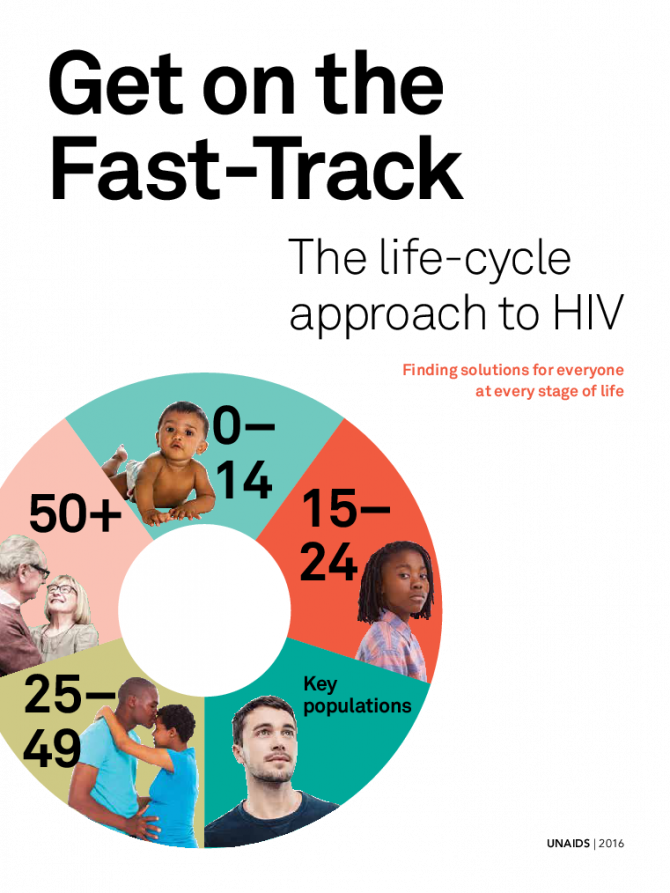
Get on the Fast-Track — The life-cycle approach to HIV
21 November 2016
In this report, UNAIDS is announcing that 18.2 million people now have access to HIV treatment. The Fast-Track response is working. Increasing treatment coverage is reducing AIDS-related deaths among adults and children. But the life-cycle approach has to include more than just treatment. Tuberculosis (TB) remains among the commonest causes of illness and death among people living with HIV of all ages, causing about one third of AIDS-related deaths in 2015. These deaths could and should have been prevented. Download slide deck


Feature Story
Preventing mother-to-child transmission of HIV
24 October 2016
24 October 2016 24 October 2016Over the past five years, there has been a rapid scale-up of services to prevent mother-to-child transmission of HIV. This has reduced the annual number of new infections among children by 50% worldwide since 2010. Globally, an estimated 77% of pregnant or breastfeeding women living with HIV were receiving antiretroviral medicines to prevent transmission of HIV to their children in 2015, up from 50% in 2010.
Antiretroviral medicines have averted 1.6 million new infections among children since 2000. There has also been a dramatic reduction in AIDS-related paediatric deaths. In the 21 priority countries that were the focus of the Global Plan towards the elimination of new HIV infections among children and keeping their mothers alive (Global Plan), AIDS-related mortality among children under 15 years of age dropped by 53% between 2009 and 2015. In countries such as Botswana, Burundi, Namibia, South Africa and Swaziland, even greater reductions, above 65%, were achieved.
However, this welcome news is tempered by some complex remaining challenges. In 2015, there were 1.8 million children under 15 years of age living with HIV worldwide. An additional 150 000 children acquired HIV globally in 2015 (2800 a week), and 110 000 children died of AIDS-related causes (300 a day). In some high-burden countries, such as Angola, Chad and Nigeria, less than half the pregnant or breastfeeding women living with HIV are receiving antiretroviral medicines.
Programmes to help women avoid HIV infection remain underdeveloped and fragile, leading to 900 000 new HIV infections among women over the age of 15 years in 2015. They joined the 17.8 million women already living with HIV, and when they decide to have children they will need services to prevent transmission to their children and maintain their own health. Programmes to help women living with HIV avoid unintended pregnancies also remain inadequate: a recent study in Kenya found that despite improvements in coverage of family planning, women living with HIV were more likely to have experienced an unintended pregnancy than other women.
The World Health Organization (WHO) now recommends treating everyone living with HIV, but it is also essential to maintain good adherence to antiretroviral medicines in order to ensure their efficacy. Good adherence suppresses viral load to undetectable levels, greatly reducing onward transmission to the baby while restoring the mother’s immune system for better health. However, many women gradually stop taking the medicines after the baby is born, increasing the risk of transmission during breastfeeding and placing their own health in jeopardy. In Malawi, a study showed that a third of 7500 pregnant or breastfeeding women did not adhere to antiretroviral therapy adequately, compromising the benefits of treatment and increasing their risk of developing drug resistance.
Access to diagnosis and treatment among children has improved, but much remains to be done. Among the 21 Global Plan priority countries, only half the children exposed to HIV received virological testing within two months of birth, as recommended by WHO. Since mortality among untreated infants is highest in the first three months of life, prompt diagnosis and linkage to treatment are crucial. Yet only half the children under 15 living with HIV in those countries were accessing treatment, compared to 80% of pregnant women living with the infection. This signals service delivery failure for children.
In order to address the unfinished agenda of the Global Plan, UNAIDS and the United States President’s Emergency Plan for AIDS Relief have launched a follow-up initiative known as Start Free, Stay Free, AIDS Free. With the goal of ending paediatric AIDS, this framework embraces the aspiration that every child should be born and remain HIV-free (start free), every adolescent and young woman should be able to protect themselves from HIV (stay free) and every child and adolescent living with HIV should have access to quality HIV treatment, care and support (AIDS-free).
Start Free, Stay Free, AIDS Free includes the targets endorsed in the 2016 United Nations Political Declaration on Ending AIDS of 95% of pregnant and breastfeeding women accessing antiretroviral medicines, reducing new HIV infections among children to 40 000 and 1.8 million children living with HIV accessing HIV treatment by 2018. It also aims to reduce new HIV infections among adolescents to under 100 000 and for 1.5 million adolescents to be on HIV treatment by 2020.
Start Free, Stay Free, AIDS Free promotes concerted and coordinated country-led action designed to close the remaining HIV prevention and treatment gap for children, adolescent women and expectant mothers. Its success will depend on tailor-made acceleration and implementation plans to respond to the country context, building on successful strategies to strengthen systems where necessary and identifying critical opportunities and actions to expand access to life-saving HIV treatment and prevention services. To support implementation, the framework also calls on industry, civil society and international partners to focus on investing in efficient and cost-effective solutions that maximize programme outcomes.
Like the Global Plan, Start Free, Stay Free, AIDS Free places women living with HIV at the centre of the response.
Hands up for #HIVprevention — World AIDS Day campaign













Feature Story
Thailand is the first country in Asia to achieve elimination of HIV transmission and syphilis from mothers to their children
27 October 2016
27 October 2016 27 October 2016Sixteen years ago, Anya Nopalit was thrilled to learn that she was pregnant, but then she received devastating news. “I learned that I had HIV. I was really sad and disappointed. I wondered, why did this happen to me?” said Ms Nopalit, who lives in a fishing village in Chantaburi province in south-east Thailand.
Her doctor encouraged her to have an abortion, but she was determined to keep her baby. “I thought what will be, will be,” said Ms Nopalit.
Luckily, in the very same year that Ms Nopalit learned about her diagnosis, Thailand became one of the first countries in the world in which pregnant women living with HIV had access to free antiretroviral therapy. Untreated, women living with HIV have up to a 45% chance of transmitting the virus to their children during pregnancy, delivery or breastfeeding. However, the risk drops dramatically if HIV treatment is given to both mother and child.
Ms Nopalit followed the treatment regimen advised by her doctor and her son was born HIV-free.
“I was so happy when the doctor told me he was HIV-negative,” said Ms Nopalit.
Thailand’s early commitment to stop babies from being born with HIV has saved many lives and in June 2016 the country received validation from the World Health Organization (WHO) for having eliminated not only the transmission of HIV but also of syphilis from mothers to their children.
According to Thailand’s Ministry of Public Health, the number of children who became infected with HIV in 2015 was 86, a decline of more than 90% over the past 15 years. The rate of mother-to-child transmission of HIV in Thailand declined from 13.6% in 2003 to 1.1% in 2015. The WHO global guideline considers mother-to-child transmission of HIV to be effectively eliminated when the rate of transmission falls below 2%.
At the Tha Mai Hospital in Chantaburi province, where Ms Nopalit accesses her HIV treatment, paediatric HIV cases have become uncommon.
“For the last three years, there were no new cases of mother-to-child transmission,” said Monthip Ajmak, Senior Nurse, Antenatal Care, Tha Mai Hospital.
One of the factors behind Thailand’s remarkable achievement is a well-developed national health system that provides quality services in even the most remote areas. According to Thai health authorities, nearly all pregnant women are routinely screened for HIV and if they are found to be HIV-positive the women start lifelong antiretroviral therapy. More than 95% of pregnant women diagnosed with syphilis also receive treatment.
In Thailand, health-care services for mothers living with HIV are fully integrated into maternal and child health-care programmes in hospitals and are covered by Thailand’s universal health-care coverage.
“Public sector staff receive continuous training, from basic counselling skills to providing a treatment regimen,” said Danai Teewanda, Deputy Director-General, Department of Health, Thailand Ministry of Public Health.
Community leadership has ensured that mothers living with HIV are linked to hospitals and supported throughout their pregnancy. The Best Friends Club at the Thai Mai Hospital has 160 members, who include men and women living with HIV. The club is divided into three groups, with more recent members meeting every month and long-time members meeting twice a month.
“Our club provides counselling services at the antenatal clinic. We coordinate with the hospital staff and provide information to women on how to take care of themselves,” said Malinee Vejchasuk, a counsellor with the Best Friends Club.
Ms Nopalit and her husband wanted to have another child. Four years ago, she gave birth to her second son.
“I am so happy that my two children are healthy and HIV-free. They are lively and play like their friends,” said Ms Nopalit.
When he is not in school, her eldest son now accompanies his parents when they catch crabs, which is their family business, while their youngest son runs around the beach and builds sand castles.
Video: Thailand is first country in Asia to eliminate mother-to-child HIV transmission
Thailand has received validation for having eliminated mother-to-child transmission of HIV and syphilis, becoming the first country in Asia and the Pacific region and also the first with a large HIV epidemic to ensure an AIDS-free generation. Meet Anya Nopalit, a mother living with HIV who has two HIV-negative children.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025

Feature Story
Tireless Indian doctor dedicated to women’s health
28 October 2016
28 October 2016 28 October 2016Gita and her husband arrived at the Sir Jamsetjee Jeejebhoy (Sir J.J.) Hospital more than 15 years ago desperately wanting to have children. Because they were living with HIV, doctors had discouraged them from becoming parents, so they travelled five hours to bustling Mumbai, India, to see Rekha Daver, with the hope of finding a solution. Any solution.
Ms Daver is a doctor who heads the gynaecology department at the state-run hospital. Under her leadership, the hospital has become a referral centre for HIV-positive pregnant women, who are often turned away from other health facilities.
“Back then I could not guarantee that their child would not be HIV-positive, but I enrolled Gita on our antiretroviral therapy programme,” Ms Daver recalled. Subsequently, Gita’s husband was enrolled on the programme. Within a year Gita gave birth to a baby girl at the hospital.
“They never missed an appointment and when their daughter was born HIV-negative you should have seen their happiness,” she said. The couple, with their teenager in tow, still visit Ms Daver, which delights her. “It is not just a question of preventing mother-to-child transmission of HIV, it’s also having two adults living healthy lives.”
Ms Daver knows all about giving life. Since 2000 her team has performed more than 1 000 deliveries of HIV positive women. As of late there is cause to celebrate because in the last two years 100 women on the new three-drug regimen have had children born HIV-free.
Sarita Jadav, the New Delhi United Nations Educational, Scientific and Cultural Organization Focal Point for HIV and School Health Education, praised Ms Daver. “Maternal and child health is one of her passions and she has dedicated more than 37 years to servicing underprivileged women,” she said. Ms Jadav stressed the fact that despite having studied and worked in the United States of America and obtained a green card, Ms Daver chose to return to India and work in state hospitals and to train thousands of medical students.
“Her tireless efforts to bring about change and to save lives have been admired by all,” Ms Jadav added.
Ms Daver talked about the importance of counselling. “When I see women who are HIV-positive and their husbands HIV-negative there are often societal pressures on the couple, not so when the man is HIV-positive and the woman is negative,” she said. “My team and I have been trying to raise awareness about safe sex practices and family planning.” She credits her work at the Human Reproduction Research Centre and at the Indian Council of Medical Research in broadening her scope regarding women’s health.
Supporting women has driven Ms Daver’s career. She always knew she wanted to be a doctor and had set her sights on being a surgeon, but growing up in a small town she realized that helping women was key and that she could make a bigger impact as an obstetrician/gynaecologist.
After attending medical college in India, she spent three years at the Texas Medical Center in Houston, United States. When she decided to move back to India her husband Dr Gustad (medical school sweetheart) and two children moved back with her.
In 1990, she started at the Sir J.J. Hospital and it was then that she started to see more and more women living with HIV.
“I realized there was no cure and that perhaps my best bet was to focus on prevention, especially from mother-to-child.”
After studying programmes in Thailand and Uganda, Ms Daver’s team started providing access to antiretroviral medicine to mothers living with HIV during their pregnancy. Without antiretroviral medicine, between 33% and 45% of infants born to women living with HIV will become infected with HIV. The Sir J.J. Hospital project became a pilot programme and Ms Daver trained other doctors from across India.
With the success of programmes to prevent mother-to-child transmission of HIV, Ms Daver can once again promote breastfeeding. “Before I worried so much because I was saving the child but mortality rates remained high because of a lack of antibodies,” she said. “Now women can safely breastfeed, which makes me so happy,” she said.
Her enthusiasm for her work is infectious, explains her daughter. “I always saw my mother’s devotion to people living with HIV, as well as her passion regarding women’s issues,” said the New York based Roshni Daver. “In fact she inspired me to become a doctor.”
“The key to my mother’s long and successful career is her excellent time management, or perhaps it’s because she wakes up very early,” said her daughter.
Her mother sees it another way, saying, “It gives me a great sense of satisfaction to help all these underprivileged women as well as to train the future generation of doctors.”
Hands up for #HIVprevention — World AIDS Day campaign
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025