
Feature Story
Consultation calls for the global AIDS response to build on emergency adaptations to COVID-19, tackle structural barriers and ensure that country programmes fully recover from COVID-19 disruptions and end AIDS
03 February 2022
03 February 2022 03 February 2022As the Omicron variant surges through communities and health systems already stretched to the breaking point by two years of COVID-19, HIV programme managers and community representatives gathered virtually to review efforts to keep the AIDS response on track and propose ways to better overcome the challenges caused by two clashing pandemics.
“The COVID-19 pandemic has disrupted health services worldwide, at different times and in different ways, and it continues to do so,” UNAIDS Deputy Executive Director, Programme, a.i., Eamonn Murphy said at the opening of the consultation. “But at the same time we’re hearing great successes. Stories and data of impressive resilience and programmatic rebound are increasingly being documented and researched.”
The participants identified the most effective innovations that have allowed HIV services to continue to reach those who need them the most and proposed follow-up research and actions that can help guard against future waves of COVID-19 infections.
“We have learned so much over the past two years of the COVID-19 pandemic. Anticipating the worst, countries and communities rallied effectively to adapt and maintain most HIV services. These global efforts have meant that although there have been gaps and disruptions to services, and some catch-up will be needed, most people living with HIV continued successfully on treatment,” said Meg Doherty, the World Health Organization (WHO) Director of Global HIV, Hepatitis and STI Programmes.
Networks of people living with HIV and key populations at higher risk of HIV infection warned that the often life-saving adaptations made to HIV services have not addressed the stigma, discrimination and structural barriers they face in their day-to-day lives. In addition, COVID-19 has left many even more vulnerable to depression, violence and other harms.
“People are working hard to ensure that treatment is still available and accessible, but people have also lost livelihoods during COVID-19, and they have taken on additional community and family responsibilities,” said Florence Anam, a Programme Manager at the Global Network of People Living with HIV (GNP+). “Strengthening of community systems of health, and the integration of mental health and psychosocial support is more important now than ever. We need to focus on reducing inequities and ensuring that people are economically empowered enough to meet their basic needs as much as possible.”
Country data collected by UNAIDS, WHO, the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and the United States President’s Emergency Plan for AIDS Relief (PEPFAR) show that HIV service disruptions were most severe during the first lockdowns that many countries put in place in early to mid-2020. A combination of movement restrictions and health systems overwhelmed by COVID-19 cases cut off many people living with HIV from the daily medicines they need to stay healthy. HIV testing, the enrolment of people newly diagnosed onto treatment and the provision of HIV prevention tools such as condoms and pre-exposure prophylaxis nearly ground to a halt. Voluntary medical male circumcision, health services for transgender people and other elective medical procedures were suspended altogether in many countries.
Prolonged service interruptions could have led to a wave of AIDS-related illnesses and deaths, undermining decades of efforts to contain the HIV virus. Programmes across the world scrambled to find new ways to reach people living with HIV and the key populations who are at highest risk of HIV infection.
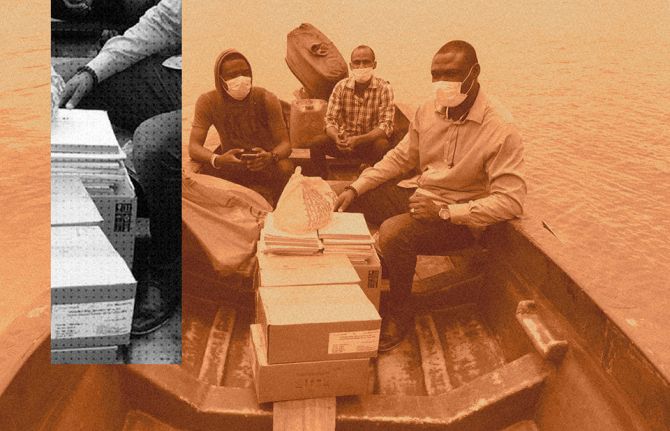
These measures included working with affected communities to deliver antiretroviral medicines door to door and to increase the quantity of medicines provided during each visit in order to reduce the frequency of medical appointments. This multimonth dispensing of antiretroviral medicines has been recommended by WHO since 2016, as it is easier for the patient and reduces the workload of the health system.
Most HIV treatment programmes quickly rebounded after adaptations were put in place.
“The data show that most national HIV treatment programmes in low- and middle-income countries responded with extraordinary resilience to protect 20 years of hard-earned gains through rapid adoption of COVID-19 adaptations,” said Siobhan Crowley, Head of HIV at the Global Fund. “The strong HIV services platform and highly engaged HIV civil society are well poised to serve as an important foundation for integrated services to tackle COVID-19 and other public health threats, but increased investment from all stakeholders is needed to sustain and build on these impressive achievements.”
Irum Zaidi, the Deputy Coordinator at the Office of the United States Global AIDS Coordinator, stressed that the strengthening of health information systems and the adoption of people-centred approaches in the years before COVID-19 was critical to the rapid reaction to the challenges created by the new pandemic.
“Over the past four years, PEPFAR and partner country governments collaborated to implement WHO policies and adaptations for providing people-centred clinical HIV services,” Ms Zaidi said. “These adaptations were rapidly scaled during COVID-19, establishing a flexible service delivery environment to keep individuals on lifelong antiretroviral therapy during COVID-19 surges. Granular real-time data along with PEPFAR’s commitment provided a path forward to support governments and beneficiaries during this unprecedented time.”
Efforts to expand access to a relatively new and promising HIV prevention option—antiretroviral medicines pre-emptively taken by people at higher risk of infection, known as pre-exposure prophylaxis, or PrEP—were also rapidly adjusted to overcome COVID-19 challenges. Those adaptations have included the shifting of clinical consultations to telemedicine and outdoor settings, the use of social media for virtual adherence support and home delivery of PrEP pills. Expansion of self-testing for HIV has helped to maintain the expansion of both PrEP and HIV treatment.
“We need to keep building the resilience that HIV services have shown by prioritizing person-centred differentiated service delivery in response to challenges posed by COVID-19,” said Adeeba Kamarulzaman, the President of the International AIDS Society.
The consultation looked ahead to a future where the COVID-19 response transitions from an acute pandemic phase to a more sustained control programme, similar to the responses to HIV, tuberculosis and other infectious diseases.
The participants agreed that, even within a best-case scenario, it will be important to build on emergency adaptations by establishing a more enabling environment for the populations who currently struggle to access services, and to ensure that HIV programmes can fully recover from COVID-19 shocks and reach the global goal of ending the AIDS pandemic by 2030.
“Perhaps one of the silver linings of the COVID-19 pandemic is how it sparked innovation and inspired their rapid adoption by countries and communities. These will have not only a positive and durable effect on the HIV response but offer models for others to adapt in tackling other health challenges,” said Wafaa El-Sadr, the founder and Director of ICAP.
The consultation, held on 1 and 2 February, was co-organized by UNAIDS, WHO, the Global Fund, PEPFAR, the International AIDS Society and ICAP at Columbia University.
