Feature Story
How one Jamaican organization is empowering adolescent girls living with HIV
10 November 2016
10 November 2016 10 November 2016Rushell Gray unflinchingly shares the story of her journey to the edge and back. She was infected with HIV after being abused at the age of nine, but her eight-year-old daughter is HIV-free. “It has been difficult. As a young girl in the community everybody turned a blind eye and blamed me,” she said. “Nobody said this man needs to go to jail. At one point I gave up because the stress was too high,” she recounts.
A petite young woman, Ms Gray is confident and articulate. She credits the Jamaican nongovernmental organization Eve for Life and its transformative programme for her turnaround. Through a combination of counselling, personal development and life-skills education, she has become one of the powerhouse peer educators of Mentor Moms.
The Mentor Moms programme deploys young, empowered women who are affected by HIV and young mothers to help others along the journey. They answer questions and offer reassurance, accompany adolescent girls to their clinic visits and they reinforce guidance on taking medicines, avoiding breastfeeding and keeping clinic appointments.
Ms Gray clarifies that the issues her mentees face are not just about HIV. “They do not have resources, they are not safe in their houses, they are afraid a partner or their family might throw them out. They might have two children or more,” she said. A 2012 survey by the Jamaica National HIV/STI Programme found that one in every five adolescent girls in Jamaica aged 15–19 years reported having experienced sexual violence.
Eve for Life Executive Director and co-founder Patricia Watson noted that many girls are being left behind. “A recent study showed that among girls in state care, 30% have sexually transmitted infections, 41% attempted suicide and 35% have been forced to have sex. Also, children infected with HIV at birth are growing older and becoming sexually active, some without having been informed about their status,” she said.
For the organization, responding to HIV among adolescent girls is about far more than promoting sex messages. It is fundamentally about social protection and addressing the structural and social issues that increase girls’ vulnerability.
For the past two years, Eve for Life has spearheaded the Nuh Guh Deh! (Don’t Go There) national campaign to end sex with girls.
“The overarching goal is to contribute to reducing sexual abuse of girls in Jamaica,” Ms Watson said.
The campaign seeks to mobilize Jamaicans to report acts of sexual violence while increasing awareness about the long-term effects of abuse and the links to HIV. Survivor stories highlight the serious issues they face. The approach maximizes participation and ownership from adolescent girls and young women who have survived sexual abuse.
The Nuh Guh Deh song by the Jamaica dub poetry group No-Maddz aims to reduce social acceptance of predatory relationships between older men and girls.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country
Related


Feature Story
#WhatWomenWant for the HIV response: a new space for new conversations
10 November 2016
10 November 2016 10 November 2016#WhatWomenWant is a virtual space that amplifies the voices of young women, allowing them to share expertise and life experiences, explore solutions and build strengthened networks across gender-related issues, sectors and movements.
Inspired by the impact of the virtual activism surrounding the 2016 Commission on the Status of Women, the Athena Network and its partners, including UNAIDS, used the momentum to build a platform where women could mobilize around the United Nations General Assembly High-Level Meeting on Ending AIDS. From May to July 2016, a social media campaign reached 13 million Twitter accounts and organized five Twitter conversations that engaged 120 000 people. The aim was to hear what women want and to identify specific actions needed to change the lives of women and girls.
The initiative continues to engage an expanding network of primarily women-led organizations working to advance gender equality, with a special focus on areas where health and rights meet.
#WhatWomenWant aims to:
- Focus attention on the urgent need to address women’s rights and gender-related disparities within and beyond the HIV response.
- Act as a catalyst for joined-up action where gender equality, human rights, sexual and reproductive health issues, gender-based violence and the HIV response intersect.
- Put women in charge of defining their own agendas.
- Harness the experience of women to create advocacy tools to advance their own solutions wherever they are.
- Identify opportunities for women to engage stakeholders and to be meaningfully involved in the decision-making processes that most affect their lives.
#WhatWomenWant continues to strengthen links across movements to end child marriage, stop sexual violence, ensure safe and legal abortion rights and advance comprehensive sexuality education.
“At a time when funding for women's rights has been on the decline, the #WhatWomenWant online campaign provides a space for young feminists to contribute to and influence global policy discussions on the HIV response,” says Catherine Nyamburra, a young activist from Kenya. “It provides a space to amplify young feminist voices through various channels of participation and for feminist thought leadership in the response to HIV.”
Video
United States Global AIDS Ambassador, Deborah Birx, explains why young women are more vulnerable to becoming infected with HIV. 1000 young women are being infected every day = 7000 a week globally.
Hands up for #HIVprevention — World AIDS Day campaign
Campaigns



Feature Story
Comprehensive sexuality education in Zambia
09 November 2016
09 November 2016 09 November 2016It is estimated that worldwide only three in 10 adolescent girls and young women between the ages of 15 and 24 years have comprehensive and correct knowledge about HIV.
With inadequate knowledge, young people are ill-equipped to make healthy and safe decisions about their sexual health. However, knowledge, while a crucial foundation, is not in itself sufficient to change behaviour and reduce the risk of HIV infection. Knowledge needs to be combined with the right skills and attitudes, which can be taught and developed through high-quality comprehensive sexuality education (CSE).
CSE not only plays an important role in preventing negative sexual and reproductive health outcomes, but also offers a platform to discuss gender issues and human rights and to promote respectful, non-violent relationships. However, gender-responsive and life-skills-based HIV and sexuality education is only covered in the national curriculum by 15% of the 78 countries analysed in the Global education monitoring report, recently launched by the United Nations Educational, Scientific and Cultural Organization.
When CSE programmes focus on gender and power relations, they are much more likely to show positive effects in reducing sexually transmitted infections and unintended pregnancies than programmes ignoring gender and power.
Such a gender-responsive CSE programme have been implemented in Zambia, which is a signatory to the 2013 Ministerial Commitment on comprehensive sexuality education and sexual and reproductive health services for adolescents and young people in eastern and southern Africa.
The curriculum in Zambia focuses on puberty, HIV prevention, gender equality, sexual and reproductive health, relationships and human rights. The overall goal is for adolescents and young people in Zambia to enjoy better sexual and reproductive health and have better health outcomes overall.
Zambia currently has the largest population of young people in its history, with 52.5% aged below 18 years. During their school years, teachers and sexual health specialists have an ideal opportunity to reach students with correct and appropriate health education information. The onset of adolescence brings not only physical change but also vulnerabilities to human rights abuses, particularly in the areas of sexuality, marriage and childbearing.
Harriet Lilanda, aged 13, a student at Twalumba Primary School in Lusaka, Zambia, thinks that the new sexuality education curriculum is important for young people. “Talking openly about sexuality was not an easy thing, as boys would think I am a loose girl. Parents at home were also closed up on us; now I think the knowledge which we are receiving in class will help me,” she said.
Both teachers and students in Zambia welcomed the introduction of CSE in schools and appreciate its contribution to the attitudes of young people.
“I saw the need to get more involved in teaching comprehensive sexuality education because of the way our society hides information on sexuality,” says Agather Shindende, a teacher at Kabulonga Primary School. “I remember growing up and being told that if you sit next to a boy at school you would conceive. I don’t want the current generation to go through what we went through.”
Schools have the potential to contribute to healthy individual behaviour as well as improved social norms around equality and non-violence, but this cannot be realized if, at the same time, they are places of gender inequality and violence. Access to a safe learning environment must be combined with education about gender equality, non-violent behaviour and sexual and reproductive health for everybody.
“Among the topics that I have learnt, gender stands out as the most interesting one,” says Harriet Lilanda. “I like gender because it teaches us to be equal. Boys and girls can do the same things—mathematics, science, home economics and technical drawing. I have learnt that we must respect each other and that household chores have to be done by girls and boys.”
Gender practices, norms and values influence sexuality, reproduction and relationships: unequal gender relations make it difficult for women and girls to make choices about sex, as well as increasing their vulnerability to violence, early marriage and adverse sexual and reproductive health outcomes.
Ms Shindende appreciates the benefits of CSE and feels that results are slowly being noticed. “The attitude and behaviour among learners regarding gender norms is slowly changing for the better, especially among boys,” she says. “Previously, boys never wanted to take subjects like home economics because they considered it as a subject for girls only, but today, out of 45 learners, 20 are boys and they willingly chose home economics as one of their optional subjects. Therefore, you can see that teaching comprehensive sexuality education from an early age can open up the minds of our young people. We also have many girls taking art and design courses, including technical drawing, which were exclusively for boys.”
When young women and adolescent girls have access to comprehensive age-appropriate sexuality education before becoming sexually active, they are more likely to make informed decisions about their sexuality and approach relationships with more self-confidence. CSE is also known to increase young girls’ condom use, increase voluntary HIV testing among young women and reduce adolescent pregnancy, especially when linked with non-school-based youth-friendly health services provided in a stigma-free environment.
Watch UNESCO video — Being a Young Person: Comprehensive Sexuality Education
Hands up for #HIVprevention — World AIDS Day campaign


Feature Story
Maximizing the potential of a new HIV prevention method: PrEP
01 November 2016
01 November 2016 01 November 2016Pre-exposure prophylaxis (PrEP)—most often a combination of tenofovir and emtricitabine taken orally as a daily tablet—is extremely effective at preventing HIV infection when taken regularly.
The choice of PrEP is recommended for people who are HIV-negative but at high risk of becoming infected. The people who can benefit most from PrEP—including gay men and other men who have sex with men, transgender people, sex workers, serodiscordant couples before the partner living with HIV becomes virally suppressed and young women and girls in the areas of sub-Saharan Africa most affected by HIV—are located where there are high rates of untreated HIV and inconsistent condom use.
People starting on PrEP must be HIV-negative and undergo repeat HIV testing every three months. The side-effects of taking PrEP are usually mild and short-lived. The risk of developing resistance to PrEP medicines is extremely low, as long as the person is confirmed to be HIV-negative when starting PrEP.
In the past two years, PrEP roll-out has moved quickly. It is estimated that in October 2016 around 100 000 people were using PrEP in more than 30 countries, with the majority of users in the United States of America. The UNAIDS target is for there to be 3 million people on PrEP worldwide by 2020.
There are now active national PrEP programmes in Australia, France, Kenya, Norway, South Africa and the United States. Botswana is pursuing regulatory approval and creating an implementation plan, while Thailand and Zimbabwe are among other countries producing guidelines for PrEP roll-out. In addition, more than 20 projects around the world are exploring the use of PrEP.
However, even where there is an existing national programme, PrEP uptake is unequal and the people who would benefit most do not always gain access. Many activists in the AIDS response continue to criticize this inequality. “PrEP is powerful, it has to reach the disempowered,” said Nöel Gordon of the Human Rights Campaign.
PrEP adds to the package of proven prevention options already available. PrEP should be used in conjunction with other prevention methods, such as male and female condoms, voluntary medical male circumcision and antiretroviral therapy for all people living with HIV. When antiretroviral therapy is effective in a person living with HIV, the virus becomes undetectable in the person’s blood and the risk of transmitting the virus to a partner approaches zero. No single HIV prevention method is 100% protective and PrEP does not prevent other sexually transmitted infections or prevent unintended pregnancy. Condoms remain the most widely available and affordable HIV prevention tool and as such should always be promoted along with PrEP.
The benefits of choosing PrEP can be psychological as well as physical and the use of PrEP may counter the anxiety and isolation felt by some people who feel they lack the ability to control their risk of exposure to HIV. PrEP can give people more autonomy about their sexual decision-making, which may also include risk reduction. PrEP may promote improved communication and intimacy with a partner, reduced fear of intimate partner violence, raised self-esteem and greater engagement with all aspects of sexual health.
Offering PrEP can encourage more people at the highest risk of HIV to attend HIV clinics, undergo HIV testing and access either PrEP or treatment depending on the test result. Either way, the outcome is good for the individual and good for HIV prevention.
PrEP gives us one more tool that we can use to better tailor the prevention package to each person’s individual needs, which can change over time. PrEP is not for everyone and is not for ever. Routine PrEP follow-up involves regular review of broader sexual health, including the diagnosis and treatment of sexually transmitted infections and discussion of appropriate combination HIV prevention strategies and contraception, as appropriate.
Hands up for #HIVprevention — World AIDS Day campaign





Feature Story
Ensuring HIV prevention and treatment services in Haiti are back on track after Hurricane Matthew
02 November 2016
02 November 2016 02 November 2016Haiti is regularly in the path of Atlantic Ocean storms, but Matthew was the most destructive hurricane in five decades and the country’s worst natural disaster since the devastating 2010 earthquake. According to the United Nations Office for the Coordination of Humanitarian Affairs, the hurricane killed 546 people, injured 438 and left thousands homeless. More than 141 000 displaced people are now living in temporary shelters.
Jasmin Désir, a community leader of the Union to Fight against Stigma and Discrimination, said the situation on the ground remains desperate for people with very few resources. It is even worse for many people living with HIV. He said their main concern now is being able to take antiretroviral medicines “when there is no food in sight.” Currently, 806 000 people need urgent food assistance.
Renel Julien, a community organizer living with HIV, mobilizes people living with HIV to get food and water. He thinks the emotional strain of dealing with the hurricane’s aftermath has taken a toll on many in the community.
Haiti’s entire health-care system was affected by the hurricane. Medical personnel and community health workers were unable to conduct home visits in some places. Most clinics were seriously damaged and some clinics and hospitals lost all their equipment, including generators, solar panels and computers. Antiretroviral medicines and other supplies were lost during the hurricane.
In the five most affected departments (Grand’Anse, South, South-East, Nippes and North-West), there were 13 994 people living with HIV and 37 functioning HIV treatment centres before Matthew.
According to UNAIDS Haiti, the hurricane has already affected HIV prevention, support, treatment and care services. Urgent programmes are needed to ensure that the current retention rate of people on treatment (between 60% and 80%) does not decline.
“One solution could be a community distribution system,” said Yafflo Ouattara, UNAIDS Country Director for Haiti. “In the short term, this might be the best option to reach people living with HIV who do not have access to their usual services.”
The UNAIDS country office in Haiti is currently supporting the national AIDS programme to gather information on the most affected departments and to explore alternatives for HIV treatment and care. Priorities include mapping treatment centres and reviewing the supply chain for antiretroviral medicines and other supplies.
Community leaders say marginalized groups, including gay men and other men who have sex with men, transgender people and sex workers, are even more vulnerable in these circumstances. Based on a preliminary assessment conducted by nongovernmental organizations in the areas most affected by the hurricane, stigma and discrimination has become a barrier to some people in need of assistance.
“Haiti was only just beginning the development phase to rebuild infrastructure following the 2010 earthquake that destroyed much of the country,” said Edner Boucicaut, Chair of Haiti’s Country Coordinating Mechanism for the Global Fund to Fight AIDS, Tuberculosis and Malaria and Country Director for Housing Works. “Having one disaster after another makes things more complicated than the typical emergency situation.”
César Núñez, Director of the UNAIDS Latin America and Caribbean Regional Support Team, said partners are working to ensure that the achievements made so far in the response to HIV are not diminished. “We are committed to ensuring that the excellent progress Haiti has made with respect to prevention and treatment is not reversed.”
Region/country
Related

Feature Story
PrEP in South Africa
04 November 2016
04 November 2016 04 November 2016There is strong demand for pre-exposure prophylaxis (PrEP) from many people at high risk of HIV infection, but in many areas it is not yet available. Where PrEP is not available through well-structured programmes, people may seek to obtain it through unofficial channels. Self-prescribing PrEP in this way would result in inadequate follow-up with no linkage to health service support and an increased risk of using substandard products, drug resistance and reduced impact.
South Africa has taken on these challenges and was the first country in Africa to approve the use of antiretroviral medicines for prevention. The country has accessed a generic supply of PrEP, thereby reducing the price of the medicines, and its delivery is integrated with other services.
The South African PrEP model is based on both rights and needs, and is initially intended for sex workers, who have the highest HIV prevalence in South Africa and face high levels of stigma and discrimination. User-friendly services have been designed in partnership with sex workers; however, the decision to use PrEP remains an individual choice, free from coercion.
Adding PrEP to combination prevention services is affordable, despite the costs associated with its roll-out, since those costs are expected to be offset by the savings made from avoiding new HIV infections and the associated benefits of increased contact with sexual health services by people at high risk of HIV infection.
“People ask me “How can you afford to implement new interventions?” and I always reply, “How can we afford not to?” Once you answer this question, you will find the way to work it out,” says Aaron Motsoaledi, South Africa’s Minister of Health.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country




Feature Story
Countries in Asia start to roll out PrEP
02 November 2016
02 November 2016 02 November 2016The Thai Red Cross Anonymous Clinic (TRCAC) sits back from a busy street in Bangkok, Thailand. It’s a familiar place for Jonas Bagas, who visits the leafy compound regularly because he is taking pre-exposure prophylaxis (PrEP) as part of a project being piloted by the clinic.
PrEP is the use of antiretroviral medicine in the form of a daily pill to prevent people from acquiring HIV. It is demonstrated to be highly effective in preventing the transmission of HIV among people at high risk of becoming infected.
“One reason I started was because I had a sexual partner who was HIV-positive,” explains Mr Bagas, who is from the Philippines but living in Bangkok for his job with APCASO.
TRCAC started its PrEP project at the end of 2014. Users are charged US$ 1 a day for their supply of pills, along with the recommended counselling and health evaluations. PrEP is only for people who are HIV-negative, so users undergo an initial HIV test and a check for other sexually transmitted infections as well as tests to measure how the liver and kidneys are functioning. After the first month, users repeat the evaluation and then return for testing every three months.
The most common side-effects of PrEP are nausea, headache and weight loss in the first month, but no serious toxicity has been observed during trials. “I find a huge urge to sleep right after taking PrEP, but since I take it at night, that’s not a huge minus,” said Mr Bagas.
While adherence and regular HIV testing present challenges for scaling up PrEP use, researchers describe it is a breakthrough in HIV prevention. Consistent condom use remains low in Asia. In most major cities less than half of gay men and other men who have sex with men are using condoms consistently, which is too low to have an impact on stopping the AIDS epidemic. UNAIDS and the World Health Organization recommend PrEP as an additional prevention choice for people at substantial risk of HIV exposure and who are ready to have regular HIV testing.
“We have been waiting quite a long time to get an HIV prevention method that you can use in privacy and without anxiety. PrEP is the answer to that,” said Nittaya Phanuphak, Head of the Prevention Department at the Thai Red Cross AIDS Research Centre.
PrEP does not prevent other sexually transmitted infections and is not a contraceptive, so health experts say it is best integrated with other sexual and reproductive health services, including the supply of condoms.
Surveys of potential users in Asia find that there is still a low awareness of PrEP as a prevention method. “I hope that PrEP becomes available in the Philippines soon,” said Mr Bagas.
In fact, the nongovernmental organization LoveYourself is starting a pilot project for PrEP, including regular check-ups, risk reduction and adherence counselling, in two of its clinics in Manila, Philippines, in November. “We will embed PrEP education in the HIV testing process. So all those who are going through HIV testing in our clinics, which is about 60 to 100 people a day, will be given PrEP information,” says Chris Lagman, the Director of Learning and Development at LoveYourself.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country


Feature Story
Preventing mother-to-child transmission of HIV
24 October 2016
24 October 2016 24 October 2016Over the past five years, there has been a rapid scale-up of services to prevent mother-to-child transmission of HIV. This has reduced the annual number of new infections among children by 50% worldwide since 2010. Globally, an estimated 77% of pregnant or breastfeeding women living with HIV were receiving antiretroviral medicines to prevent transmission of HIV to their children in 2015, up from 50% in 2010.
Antiretroviral medicines have averted 1.6 million new infections among children since 2000. There has also been a dramatic reduction in AIDS-related paediatric deaths. In the 21 priority countries that were the focus of the Global Plan towards the elimination of new HIV infections among children and keeping their mothers alive (Global Plan), AIDS-related mortality among children under 15 years of age dropped by 53% between 2009 and 2015. In countries such as Botswana, Burundi, Namibia, South Africa and Swaziland, even greater reductions, above 65%, were achieved.
However, this welcome news is tempered by some complex remaining challenges. In 2015, there were 1.8 million children under 15 years of age living with HIV worldwide. An additional 150 000 children acquired HIV globally in 2015 (2800 a week), and 110 000 children died of AIDS-related causes (300 a day). In some high-burden countries, such as Angola, Chad and Nigeria, less than half the pregnant or breastfeeding women living with HIV are receiving antiretroviral medicines.
Programmes to help women avoid HIV infection remain underdeveloped and fragile, leading to 900 000 new HIV infections among women over the age of 15 years in 2015. They joined the 17.8 million women already living with HIV, and when they decide to have children they will need services to prevent transmission to their children and maintain their own health. Programmes to help women living with HIV avoid unintended pregnancies also remain inadequate: a recent study in Kenya found that despite improvements in coverage of family planning, women living with HIV were more likely to have experienced an unintended pregnancy than other women.
The World Health Organization (WHO) now recommends treating everyone living with HIV, but it is also essential to maintain good adherence to antiretroviral medicines in order to ensure their efficacy. Good adherence suppresses viral load to undetectable levels, greatly reducing onward transmission to the baby while restoring the mother’s immune system for better health. However, many women gradually stop taking the medicines after the baby is born, increasing the risk of transmission during breastfeeding and placing their own health in jeopardy. In Malawi, a study showed that a third of 7500 pregnant or breastfeeding women did not adhere to antiretroviral therapy adequately, compromising the benefits of treatment and increasing their risk of developing drug resistance.
Access to diagnosis and treatment among children has improved, but much remains to be done. Among the 21 Global Plan priority countries, only half the children exposed to HIV received virological testing within two months of birth, as recommended by WHO. Since mortality among untreated infants is highest in the first three months of life, prompt diagnosis and linkage to treatment are crucial. Yet only half the children under 15 living with HIV in those countries were accessing treatment, compared to 80% of pregnant women living with the infection. This signals service delivery failure for children.
In order to address the unfinished agenda of the Global Plan, UNAIDS and the United States President’s Emergency Plan for AIDS Relief have launched a follow-up initiative known as Start Free, Stay Free, AIDS Free. With the goal of ending paediatric AIDS, this framework embraces the aspiration that every child should be born and remain HIV-free (start free), every adolescent and young woman should be able to protect themselves from HIV (stay free) and every child and adolescent living with HIV should have access to quality HIV treatment, care and support (AIDS-free).
Start Free, Stay Free, AIDS Free includes the targets endorsed in the 2016 United Nations Political Declaration on Ending AIDS of 95% of pregnant and breastfeeding women accessing antiretroviral medicines, reducing new HIV infections among children to 40 000 and 1.8 million children living with HIV accessing HIV treatment by 2018. It also aims to reduce new HIV infections among adolescents to under 100 000 and for 1.5 million adolescents to be on HIV treatment by 2020.
Start Free, Stay Free, AIDS Free promotes concerted and coordinated country-led action designed to close the remaining HIV prevention and treatment gap for children, adolescent women and expectant mothers. Its success will depend on tailor-made acceleration and implementation plans to respond to the country context, building on successful strategies to strengthen systems where necessary and identifying critical opportunities and actions to expand access to life-saving HIV treatment and prevention services. To support implementation, the framework also calls on industry, civil society and international partners to focus on investing in efficient and cost-effective solutions that maximize programme outcomes.
Like the Global Plan, Start Free, Stay Free, AIDS Free places women living with HIV at the centre of the response.
Hands up for #HIVprevention — World AIDS Day campaign
Related


Feature Story
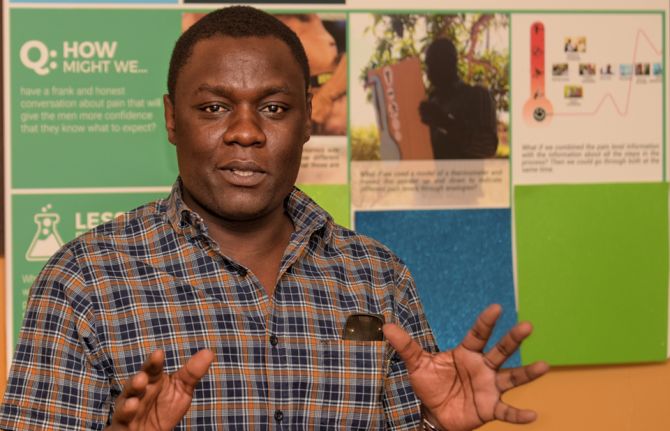
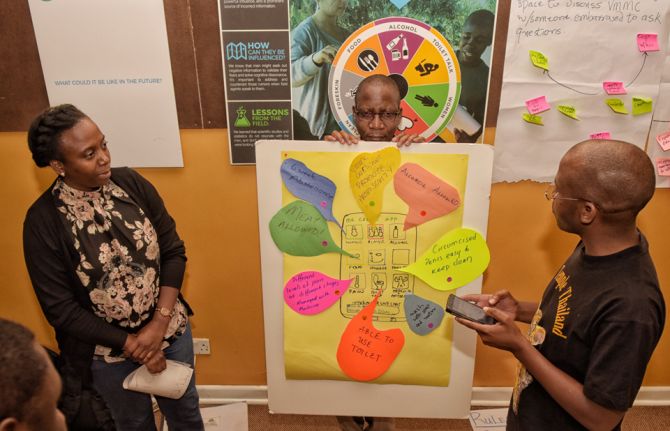
Using market research for long-term sustainability of VMMC in Zimbabwe and Zambia
19 October 2016
19 October 2016 19 October 2016Voluntary medical male circumcision (VMMC) provides at least a 60% protective effect against HIV infection for men, but, while service delivery for VMMC has improved, uptake has stalled. In response, the Bill & Melinda Gates Foundation funded Ipsos Healthcare, a market research company, to investigate how to better understand behavioural and psychographic characteristics of men and boys and the barriers and facilitators within their journey from awareness of the VMMC to uptake.
Much is known about why men undergo VMMC, but those reasons and how men’s beliefs influence decisions to opt for it have not been systematically mapped.
The stages a man goes through when deciding to have VMMC in Zambia and Zimbabwe were documented in order to understand the path to the decision, what affected their decision, the roles of key influencers and how boys and men tend to take different paths to VMMC, depending on their age. Ipsos discovered that, on average, it took men two years and three months to move from awareness of VMMC to having the procedure.
Ipsos surveyed 2000 men between the ages of 15 and 30 in the two countries. The findings showed that men fall into six groups with respect to their attitudes towards VMMC and wanted answers regarding five themes: sex appeal; procedure; pain; social support; and the benefits.
With support from the Bill & Melinda Gates Foundation to translate this research to practice, PSI Zimbabwe and the Society for Family Health, Zambia, used the results of the research to fine-tune and tailor messages to different groups of men. The research also improved the confidence of community workers in delivering previously uncomfortable messages, especially on pain and sex.
PSI Zimbabwe and the Society for Family Health, Zambia, prioritized the different groups by group size, ease of conversion, ability to advocate with peers and risk behaviour. After analysis of the research, they created “personas” of each group and identified areas where programmes and specific messaging could have the most impact.
Community workers mobilizing demand for VMMC report that they are able to quickly identify potential clients from the prioritized groups and target age groups. They are seeing fewer men but achieving a higher conversion rate as a result of the shift from group discussions to one-on-one discussions based on the research.
PSI Zimbabwe and the Society for Family Health, Zambia are now piloting messages and final concepts before scaling up programmes for the long-term sustainability of VMMC implementation.
Hands up for #HIVprevention — World AIDS Day campaign













Feature Story
Thailand is the first country in Asia to achieve elimination of HIV transmission and syphilis from mothers to their children
27 October 2016
27 October 2016 27 October 2016Sixteen years ago, Anya Nopalit was thrilled to learn that she was pregnant, but then she received devastating news. “I learned that I had HIV. I was really sad and disappointed. I wondered, why did this happen to me?” said Ms Nopalit, who lives in a fishing village in Chantaburi province in south-east Thailand.
Her doctor encouraged her to have an abortion, but she was determined to keep her baby. “I thought what will be, will be,” said Ms Nopalit.
Luckily, in the very same year that Ms Nopalit learned about her diagnosis, Thailand became one of the first countries in the world in which pregnant women living with HIV had access to free antiretroviral therapy. Untreated, women living with HIV have up to a 45% chance of transmitting the virus to their children during pregnancy, delivery or breastfeeding. However, the risk drops dramatically if HIV treatment is given to both mother and child.
Ms Nopalit followed the treatment regimen advised by her doctor and her son was born HIV-free.
“I was so happy when the doctor told me he was HIV-negative,” said Ms Nopalit.
Thailand’s early commitment to stop babies from being born with HIV has saved many lives and in June 2016 the country received validation from the World Health Organization (WHO) for having eliminated not only the transmission of HIV but also of syphilis from mothers to their children.
According to Thailand’s Ministry of Public Health, the number of children who became infected with HIV in 2015 was 86, a decline of more than 90% over the past 15 years. The rate of mother-to-child transmission of HIV in Thailand declined from 13.6% in 2003 to 1.1% in 2015. The WHO global guideline considers mother-to-child transmission of HIV to be effectively eliminated when the rate of transmission falls below 2%.
At the Tha Mai Hospital in Chantaburi province, where Ms Nopalit accesses her HIV treatment, paediatric HIV cases have become uncommon.
“For the last three years, there were no new cases of mother-to-child transmission,” said Monthip Ajmak, Senior Nurse, Antenatal Care, Tha Mai Hospital.
One of the factors behind Thailand’s remarkable achievement is a well-developed national health system that provides quality services in even the most remote areas. According to Thai health authorities, nearly all pregnant women are routinely screened for HIV and if they are found to be HIV-positive the women start lifelong antiretroviral therapy. More than 95% of pregnant women diagnosed with syphilis also receive treatment.
In Thailand, health-care services for mothers living with HIV are fully integrated into maternal and child health-care programmes in hospitals and are covered by Thailand’s universal health-care coverage.
“Public sector staff receive continuous training, from basic counselling skills to providing a treatment regimen,” said Danai Teewanda, Deputy Director-General, Department of Health, Thailand Ministry of Public Health.
Community leadership has ensured that mothers living with HIV are linked to hospitals and supported throughout their pregnancy. The Best Friends Club at the Thai Mai Hospital has 160 members, who include men and women living with HIV. The club is divided into three groups, with more recent members meeting every month and long-time members meeting twice a month.
“Our club provides counselling services at the antenatal clinic. We coordinate with the hospital staff and provide information to women on how to take care of themselves,” said Malinee Vejchasuk, a counsellor with the Best Friends Club.
Ms Nopalit and her husband wanted to have another child. Four years ago, she gave birth to her second son.
“I am so happy that my two children are healthy and HIV-free. They are lively and play like their friends,” said Ms Nopalit.
When he is not in school, her eldest son now accompanies his parents when they catch crabs, which is their family business, while their youngest son runs around the beach and builds sand castles.
Video: Thailand is first country in Asia to eliminate mother-to-child HIV transmission
Thailand has received validation for having eliminated mother-to-child transmission of HIV and syphilis, becoming the first country in Asia and the Pacific region and also the first with a large HIV epidemic to ensure an AIDS-free generation. Meet Anya Nopalit, a mother living with HIV who has two HIV-negative children.