


Feature Story
How the Jamaica transgender community is surviving COVID-19
24 September 2020
24 September 2020 24 September 2020Rose Clark (not her real name) is a 21-year-old transgender woman living in Kingston, Jamaica. Through sex work she’d been able to afford the basics—food, clothes and a small apartment.
Another transgender woman, Carla John (not her real name), worked in a hotel bar on Jamaica’s north coast. It allowed her to live independently of an unsupportive family since she was 19 years old.
COVID-19 upturned their lives. A night-time curfew made it impossible for Ms Clark to work. She was evicted in May. Ms John’s employer shut down operations in April and sent staff home. Since then she’s been living with hostile relatives.
These two are not alone. The Equality Group—a coalition of civil society organizations serving lesbian, gay, bisexual and transgender (LGBT) people in Jamaica—conducted an online survey to gauge the impact of COVID-19 on the LGBT community. It found that a quarter of respondents had lost their job, while three in 10 were unable to pay for food, rent or utilities.
“There’s been a sharp increase in homelessness,” reported Renae Green, Associate Director of Policy and Advocacy at Transwave. “The community has experienced major loss of income and people are unable to pay for housing, food and other basic amenities.”
The transgender community as a whole has several layers of vulnerability—low access to education and employment, small or non-existent family safety nets and high vulnerability to gender-based violence. These are the underlying causes for a 2018 study finding that half (51%) of transgender women in Jamaica were living with HIV.
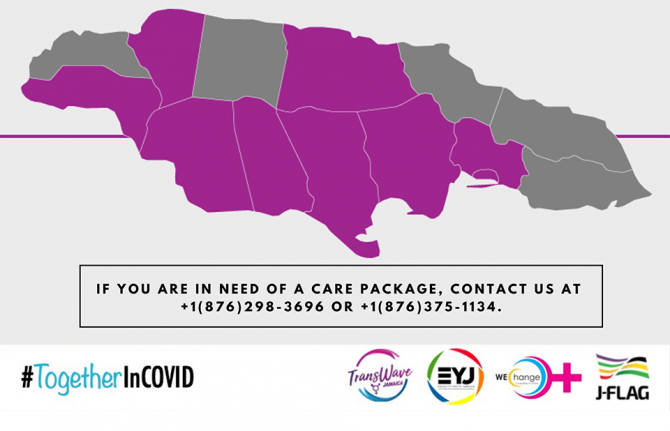
Transwave has collaborated with WE-Change, JFLAG and Equality Youth to run a COVID-19 hotline. It also provided care packages, including non-perishable food items and toiletries, to people in need. Already more than 100 transgender people have benefitted.
Critically, a Trans Emergency Fund was established to raise money to cover or subsidize applicants’ rent for short periods. Both individuals and organizations have made donations. And Transwave manages a virtual support group, providing much needed emotional solidarity during this trying time.
If anything, COVID-19 has intensified Transwave’s ongoing efforts to shine a light on the hidden issues facing one of Jamaica’s most marginalized groups.
“We are not included in decision-making processes,” Ms Green said plainly. “Decision-makers barely talk about us. We keep having to say “remember trans people”.”
UNAIDS Jamaica provided financial support that was used to ensure that Transwave had personal protective equipment and to supplement care package supplies. The office has also made certain that transgender issues are included in the coordinated HIV civil society response to COVID-19.
This fresh pandemic response has unfolded alongside Transwave’s 2020 strategic planning work, which has been supported by UNAIDS and the United Nations Population Fund.
“There is an urgent advocacy agenda for transgender people that includes all the social determinants to health and human rights,” said Manoela Manova, the UNAIDS Country Director for Jamaica.
“COVID-19 has laid bare just how vulnerable people are when they do not have equitable access to opportunities, justice and health care,” added UNAIDS Jamaica’s Community Mobilization Adviser, Ruben Pages. “That’s why it’s so important and inspiring that Transwave has continued its core work through all this.”
Our work
Region/country




Feature Story
“Physical distance, not social distance”: supporting Jamaican women living with HIV during COVID-19
21 September 2020
21 September 2020 21 September 2020The socioeconomic impact of COVID-19 is clear. People have lost incomes. Children are out of school. Food and housing insecurity are on the rise. And there has been an increase in domestic violence.
But for many women living with HIV in Jamaica, there are added layers of stress. According to the Jamaica Community of Positive Women (JCW+), many of their clients reported having received only one month’s supply of HIV treatment, although they were hoping for the recommended three months. New screening protocols at certain clinics have made some people feel exposed to unfamiliar health-care staff and unexpected disclosure of their HIV status. A few women report not having been able to access contraception on time.
According to the Coordinator of JCW+, Olive Edwards, the pressure of dealing with both pandemics has had a huge mental health impact on women living with HIV.
“Uncertainty is taking a toll,” she said. “It has disrupted life and people are worried. Some are struggling to cope with these feelings of constant uncertainty.
JCW+’s main objective for 2020 was to provide community support for women living with HIV in order to improve treatment adherence and reach viral suppression. When COVID-19 hit in March, they were presented with an added challenge. How would they address women’s new needs?
UNAIDS Jamaica’s COVID-19 emergency response contributed hygiene supplies to care packages. JCW+ used these as an entry point for connecting with clients. Women were provided with soap, household disinfectant and bleach and were shown during peer-share sessions how to use those products, along with masks made by a community mobilizer.
From there, the organization linked women to the Positive Health and Dignity Movement and treatment adherence projects. JCW+ participants prepared personal development plans with a focus on treatment adherence, education, job training and certification goals, where necessary. They keep in contact with the care teams in order to ensure access to optimal health and social support services. They have conversations to keep hope alive and send text reminders to reinforce key health and well-being messages.
“Community needs to be engaged at this time. Managing COVID-19 is about physical distance, not social distance. We felt women needed to meet and talk,” Ms Edwards said. They’ve limited support group sessions to eight people at a time.
According to the UNAIDS Country Director for Jamaica, Manoela Manova, the AIDS response must now strike a delicate balance.
“We must address standing health-care and human rights priorities as well as the immediate physical needs triggered by the COVID-19 response,” Ms Manova said.
Going forward, Ms Edwards says JCW+’s advocacy priorities are ensuring that the HIV response is not neglected because of COVID-19 and ensuring the most marginalized people are caught by state social safety nets.
Ms Edwards asked that UNAIDS continue to “feel the pulse of what is taking place” and support community outreach strategies that are relevant to Jamaican culture.
Our work
Region/country





Feature Story
COVID-19 brings Jamaican people living with HIV closer together
18 September 2020
18 September 2020 18 September 2020COVID-19 has brought new challenges for many people living with HIV in Jamaica:
“I am concerned about going to the clinic too often, but I can only get one month’s supply of antiretrovirals at a time.”
“The place I normally go to meet with my community facilitator is no longer available. Now how do I access care?”
“I haven’t been taking my medicines the way I should. Am I going to catch COVID-19?”
For Dane Lewis, Programme Manager of the Jamaica Network of Seropositives (JN+), addressing the community’s anxieties has cleared a path to more connection and support.
“JN+ started doing a survey almost immediately. We reached about 70% of our membership. This was an opportunity to reconnect to our base, to see what the needs were. It helped us to re-establish contact and brought our community closer together,” he said. “Ultimately we think this pandemic will help us bring and keep more people in care.”
There are an estimated 32 000 people living with HIV on the Caribbean island. In 2019, just 44% of them were on antiretroviral therapy, while roughly one third (35%) were virally suppressed. While most people access treatment through the public health-care sector, community organizations like JN+ play a key role in supporting people to start antiretroviral therapy and stay the course.
They’ve also been a critical partner during COVID-19. Despite having a multimonth dispensing policy, the Jamaica Government has authorized just monthly dispensing in order to avoid stock-outs.
“Community organizations like JN+ have allayed fears and followed-up so that people continue their treatment,” said UNAIDS Jamaica Country Director, Manoela Manova. “That’s why it’s important that civil society is at the decision-making table and that community workers are classified as essential workers during COVID-19.”
For the organization’s retention navigators, not much has changed. They continue to reach out to clients via the telephone to check in on whether they are taking their medicines as they should. There has been more of a shift for community facilitators, who were traditionally connected to treatment sites. Face-to-face support has largely given way to telephone calls and video chats. Twice a month, online sessions are used to address wide-ranging community concerns. JN+ team members are on hand to do things like drop off care packages or connect clients affected by community lockdowns to new treatment sites. The organization has also helped people register to receive financial support from the state.
“There has been a lot of anxiety about being able to access basic food and sanitation items. People lost jobs because of the pandemic, so anxieties turned into real needs for many. We had to stop doing in-person activities, such as our support groups, and refocus our energies on coordinating the peers to provide care packages. The support and network we offer have been important,” Mr Lewis explained.
The JN+ COVID-19 experience underlines the key role that community organizations play in helping clients to access resources.
UNAIDS Jamaica has been working to support the response at the practical and tactical levels. It provided hygiene products to be widely distributed and also facilitated weekly collaboration between civil society organizations responding to the needs of people living with HIV during COVID-19.
“Community organizations save lives,” said Ruben Pages, UNAIDS Jamaica’s Community Mobilization Adviser. “The JN+ experience shows why it is important to support community organizations that are able to reach marginalized people with unique support that those in need are not able to find anywhere else.”
Our work
Region/country




Feature Story
Pacific Unite concert promotes solidarity during the COVID-19 pandemic
16 September 2020
16 September 2020 16 September 2020Broderick Mervyn and his colleagues huddled around a computer, curiosity giving way to pride, as they tuned in to the Pacific region’s first-ever virtual concert.
“I’m from Rotuma Island, a lesser known island of Fiji, and when I saw a Rotuman group perform, there was a sense of pride, admiration and patriotism of not only our country but our culture,” said Mr Mervyn, Coordinator and Founder of Ignite4Change, an organization that advocates for political participation by vulnerable groups.
Mr Mervyn’s sentiments were shared by fellow Pacific islanders and diaspora. At a time of isolation, when many are missing their family due to closed borders or feeling alone, listening to songs of hope performed by dozens of notable musicians and emerging, homegrown artists brought reassurance. The concert, Pacific Unite: Saving Lives Together, was organized by the United Nations in collaboration with community partners intent on bringing communities together in the time of COVID-19 in order to foster solidarity, pay tribute to essential workers and encourage everyone to play their part in preventing the spread of the epidemic.
The concert featured supportive messages from leaders and influencers, including Prince Charles, Fijian Prime Minister Frank Bainimarama and New Zealand’s Prime Minister, Jacinda Ardern, and showcased the region’s vibrant cultures.
“It was educational just as it was entertaining—we got to see and hear from other Pacific islands,” said Foto Ledua, a station manager of Buzz FM in Vanuatu. “As a whole, it is such a great promotion for the Pacific and showed how diverse our cultures are, how rich our music is and how incredibly talented our people are.”
Ms Ledua spoke about the changes brought by COVID-19, including the economic crisis from decreased tourism and the losses that artists face without live concerts to perform at. She said that, “At a time like this, when people can’t travel out of their countries, or even their cities, having a concert brought into your living room is really uplifting.” The concert was broadcasted on television and radio in 13 Pacific countries, Australia and New Zealand and has reached nearly 75 000 views on the United Nations YouTube and Facebook platforms.
Ms Ledua observed that among those watching the event with her, the concert sparked conversations about the impact of COVID-19, as well as climate change, economic recession and other issues facing the people of the Pacific. Reflecting on the response to COVID-19, she said, “In our diversity, we are the same—we may be from different islands, different countries, but we all face the same problems here in the Pacific. We've been through difficult periods in our history, and we survived. We can get through this if we all work together.”
The Speaker of Parliament of Fiji and UNAIDS Regional Goodwill Ambassador for Asia and the Pacific, Ratu Epeli Nailatikau, expressed a similar view on the need to come together to combat the spread of COVID-19. “There are those with no safety net to fall back on … until we beat COVID-19, and hopefully nurse our economies back to normal, we need to act together to slow the spread of the virus and look after each other,” he said.
As the first virtual concert in the region, Pacific Unite brought the people of the Pacific together, reaffirming their shared culture and resilience, and also highlighted the critical role that UNAIDS can play in coordinating the COVID-19 response. Across countries, UNAIDS country directors have led or supported efforts in ensuring that United Nations staff and their dependents have access to the latest COVID-19 information, treatment, care and support. UNAIDS staff have the specialized experience of responding to health crises and building the capacity of communities to prevent the spread of epidemics. The Pacific is no different, where Renata Ram, the UNAIDS Country Director for Fiji and the Pacific and Chair of the United Nations Communications Group for the Pacific, led the charge to mobilize United Nations agencies and community partners and to guide the planning and execution of the concert.
“I accepted the United Nations Resident Coordinator’s proposal to organize the concert, recognizing that it must be for the Pacific, by the Pacific. The soul of the concert were the stories told by communities on how they are coping in a COVID-19 world. These stories and the concert itself speak to the driving force of UNAIDS—the power of communities,” said Ms Ram.
An isolated region, the Pacific is not always afforded the opportunity to be heard on the global stage. Ms Ram spoke about the impact of the virtual concert, stating, “We have unlocked a new communication tool through which voices from the Pacific can be heard. Too often our voices are drowned out due to our small numbers, too often we have been left behind.”
The Pacific Unite virtual concert reveals new possibilities for connection and action and exemplifies how the United Nations can mobilize with artists, community partners and governments to innovatively face the challenges at present and in the future.
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa




Feature Story
Somalia: building a stronger primary health care system
15 September 2020
15 September 2020 15 September 2020This story was first published by WHO
In the first year of the Stronger Collaboration, Better Health: The Global Action Plan for Healthy Lives and Well-being for All (GAP), 12 signatory agencies have engaged with several countries to help them achieve their major health priorities. The initial focus has been on strengthening primary health care and sustainable financing for health. Somalia is one of the countries where progress under the GAP is most advanced and where its added value has been most clearly demonstrated.
The Somalia country Director and Representative of the World Food Programme, Dr Cesar Arroyo underlined the vital importance of the GAP – through cementing collaboration among the 12 agencies: “The GAP initiative marks a crucial step towards solving health-related challenges in Somalia and offers us an opportunity to strengthen our partnerships across the humanitarian community thereby enhancing operational efficiency, particularly within the COVID-19 context and beyond”.
Three decades of civil war and instability have weakened Somalia’s health system and contributed to it having some of the lowest health indicators in the world. The situation varies from region to region but between 26-70% of Somalia’s 15 million people live in poverty and an estimated 2.6 million people have been internally displaced.
But the Government is committed to using current opportunities to strengthen health and social development. These include implementation of Somali National Development Plan for 2019–2024 and the Somali Universal Health Coverage (UHC) Roadmap, launched in September 2019.
Both plans identify primary health care as the main approach to improving health outcomes in the country. Primary health care provides whole-person care for most health needs throughout the lifespan, ensuring that everyone can receive comprehensive care ─ ranging from health promotion and prevention to treatment, rehabilitation and palliative care ─ as close as possible to where they live.
Working together, the Government of Somalia, GAP agencies and multilateral and bilateral partners have identified 5 priorities for enhanced collaboration to accelerate progress towards UHC.
Says Monique Vledder, Head of Secretariat for the Global Financing Facility for Women, Children and Adolescents: “The launch of the Global Action Plan has helped accelerate momentum across global health agencies to align their support to country partners. In Somalia, the GFF has brought the spirit of the GAP from the global to the country level, convening partners across the federal and local governments, Somaliland, UN agencies, donors and civil society to establish the Health Sector Coordination Committee. Country stakeholders and GAP agencies are now building consensus around a priority package of essential services and critical health system reforms”.
Establishment of a health coordination mechanism
Efforts are underway to set up a coordination mechanism for all health partners to strengthen primary health care and fill gaps in services at the district level, building consensus around a priority package of essential services and critical health system reforms and mapping the availability of services and health workers.
Improving access to a package of high-quality essential health services
The country’s health services package is being updated with support from GAP agencies and other partners, with a focus on prevention and community-based components, communicable and noncommunicable diseases, and mental health.
Strengthening emergency preparedness and response through UHC
Somalia is prone to emergencies from natural disasters and disease outbreaks and is now responding to COVID-19. GAP agencies are exploring opportunities to support the finalization and implementation of components of a National Action Plan for Health Security, which includes strengthening of laboratory and early warning systems and ensuring that a package of essential health services and key commodities are effectively delivered in humanitarian settings.
Strengthening the role and capacity of the Ministry of Health
This is essential to address fragmented health service delivery and funding arrangements; improve institutional capacity for policy-making, regulation, coordination, planning, management and contracting; and use of data in decision-making.
Harnessing the private sector for UHC
Private health services and the pharmaceutical sector are largely unregulated in Somalia but could contribute to improving access and achieving UHC. GAP agencies are exploring opportunities to support the development and operationalization of a strategy for the private health sector, to assess its current role in service delivery and implementation of regulatory frameworks and contracting mechanisms.
“GAP provides us an opportunity to accelerate progress in achieving universal health coverage in Somalia through coordinated action and alignment with development partners and UN agencies. More than ever, we now need to push this agenda as we support the health systems of Somalia recover stronger and better from the COVID-19 pandemic“, said WHO Country Representative in Somalia, Dr Mamunur Malik.
“Our collective engagement in improving access to care for women, children, and other vulnerable groups will be decisive in improving health and well being in the country. Through an integrated, coordinated and collaborative approach such as the GAP, we can also build the required capacity of national and local health authorities to deliver not only cost-effective health interventions using a primary healthcare approach, but also monitor and track porgress of the health-related indicators of sustainable development goal in the country", he added.
Although there are many health and social challenges in Somalia, the GAP is leveraging emerging opportunities to strengthen primary health care to support the country in achieving UHC and other health-related SDGs.
To move these efforts forward, GAP agencies are collaborating with the Government to develop an operational plan. They aim to align this with the new funding that a number of agencies are providing for the response to COVID-19, to support the scale-up of primary health care, including implementation of the package of essential health services.
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025






Feature Story
Shelter for key populations in Kyrgyzstan
15 September 2020
15 September 2020 15 September 2020Ishenim Nuru, which means “Ray of faith” in Kyrgyz, is a community organization that has been operating in the Chui region of Kyrgyzstan for many years. It started as a group of people living with HIV, their relatives and volunteers and then established itself as a nongovernmental organization that continues to work to fulfil its mission of improving the quality of life of people living with HIV.
Today, Ishenim Nuru provides the only shelter in the area for people in key populations. “With the COVID-19 epidemic, the situation has worsened for many people, but it has become extremely difficult for people released from prison who are living with HIV, people with tuberculosis and representatives of key populations—many of whom were left without a roof over their head and without help. Therefore, we decided to open a shelter,” said Elmira Asanovna Dzhorbaeva, the head of Ishenim Nuru.
The shelter is a place where people can come and receive basic services, where they can sleep, eat and wash clothes, explained Ms Asanovna. “In our shelter, people living with HIV and their family members can get, in addition to basic services, referral to medical institutions. We work closely with city and regional AIDS centres, send clients for viral load tests, provide adherence counselling, engage lawyers, restore documents, provide psychological assistance, and even help with employment,” she added.
Currently, the shelter can accommodate only 10 people at a time, but according to Yuri Malyshev, the shelter’s social worker, when the situation becomes bad sometimes up to 30 people live in the shelter. “We put in additional beds, try to find a way out. People with different destinies live here, some have no documents, some cannot apply for a pension, some have recently been released from prison, and everyone should have a chance. Our main condition is for a person to have a desire to change and adherence to antiretroviral therapy.”
To date, the shelter’s activities are supported by a United Nations Development Programme project, with financial support from UNAIDS. According to Ms Asanovna, the organization is actively discussing the sustainability of the shelter in the face of reduced donor funding amid COVID-19. “We are looking for sponsors, writing projects, we are planning to build our own greenhouse, build a carpentry shop and our own bakery, so that clients have work. Of course, we dream that one day the shelter will have its own property, since we are renting a small house. I really hope that all our dreams will come true.”
Meerim Sarybaeva, UNAIDS Country Manager for Kyrgyzstan, said, “People who need critical support should get it. In the absence of shelters run by the state, this deficiency is being filled by nongovernmental organizations that are mobilizing resources and providing the needed assistance to people during the coronavirus pandemic.”
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025




Feature Story
Cash donations for people who use drugs during COVID-19 in Bangladesh
09 September 2020
09 September 2020 09 September 2020“I cannot provide my family with sufficient food as my earnings have gone down. I feel depressed seeing my family going through economic pain and hunger,” says Kamal Hossain (not his real name), a person who uses drugs who lives in Dhaka, Bangladesh.
The COVID-19 pandemic is affecting the lives and livelihoods of people everywhere. The impact is especially being felt by people who are socioeconomically disadvantaged or marginalized. In Bangladesh, for people who use drugs and who are already struggling with disenfranchisement from the wider community, the hardships they face in making a living and accessing social protection schemes have been exacerbated.
Some of Mr Hossain’s peers worked before the pandemic, but they lost their jobs during the lockdown. Recreation facilities and drop-in-centres where previously they received health and psychosocial support were either closed or only partially operational, and clinical services were disrupted.
To support people who use drugs during the lockdown, UNAIDS made a donation to the Network of People Who Use Drugs (NPUD). With the donation, NPUD provided meals and clothing during the Eid ul-Fitr festival to people who inject drugs and who are living on the street. Food was distributed by members of the local community. For some, this was the only support they had received during the COVID-19 pandemic.
“I received only one meal during the lockdown. I did not receive any government support as I do not have a national identity card. I also received a mask and soap from a civil society organization,” said Rafiq Uddin (not his real name), who is homeless and uses drugs in Dhaka.
Community-based organizations are struggling to support the livelihoods of people from the populations most at risk, including people who use drugs.
“Since NPUD is an organization of people who use drugs, we cannot stay away from this crisis. In this time of difficulty, some leaders of NPUD have come forward to help and UNAIDS’ support has made the first step to make a difference,” said Shahed Ibne Obaed, the President of NPUD.
After receiving the donation from UNAIDS, NPUD reached out to other partners, including CARE Bangladesh, Save the Children (Bangladesh), local humanitarian agencies and volunteer organizations, to provide more comprehensive food support.
“I received some cash from a volunteer organization in my locality. Some of my relatives and well-wishers helped me with food. I also tried to do some income-generating work to support my family, but it was not available on a regular basis,” said Mr Hossain, who is a member of Ashakta Punarbashan Sangstha (APOSH), a community-based organization in Dhaka.
NPUD mobilized enough resources from various sources to continue to support people who inject drugs and people living with HIV in the older parts of Dhaka and beyond. Around 1600 people who use drugs have benefited from the initiative. Coordination between NPUD and other community-based organizations helped to identify beneficiaries. Outreach workers from drop-in centres, APOSH, Prochesta, Old Dhaka Plus, Alor Pothe and others helped to distribute food and clothes. Members of community-based organizations offered their homes as places to prepare and pack food.
NPUD procured personal protective equipment for outreach workers and masks and soap for beneficiaries and set up an online group to share updates and pictures and give information about their activities. The whole initiative was fully voluntary.
“A major concern is the shortage of human and financial resources to support all vulnerable people who use drugs. Wider donor involvement is necessary to generate more funds to support them, especially those who are living on the street, and to ensure sustainability of this initiative,” said Saima Khan, UNAIDS Country Manager in Bangladesh.
Region/country




Feature Story
Guyana’s HIV food bank comes to the rescue during COVID-19
04 September 2020
04 September 2020 04 September 2020For many Guyanese families, COVID-19 has meant far more than mask-use and movement restrictions.
“The disruptive effect on economic activity means that for some there simply is not enough food,” said Michel de Groulard, UNAIDS Country Director, a.i., for Guyana and Suriname.
But for people living with HIV in Guyana, there’s been no need for a hastily improvised nutrition support solution. For almost 14 years the National AIDS Programme secretariat has invested in the development of a food bank specifically for people living with HIV, including those coinfected with tuberculosis.
The programme started with support from the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and continues to receive Global Fund contributions. From the start there were consistent, major donations from the National Milling Company of Guyana. Since 2017, the Government of Guyana and the Food for the Poor charitable organization have been the primary donors. Importantly, throughout the years the food bank has attracted significant inputs from the private sector. In 2019, there were more than 20 corporate contributors.
Referrals come from the clinical teams attending to people living with HIV. Food support is granted for an initial six-month period, after which the situation is reassessed. In the interim there is a collaborative effort with the Ministry of Social Protection and the Recruitment and Manpower Agency around job placement and other types of social support.
Rhonda Moore worked as an HIV doctor for six years and in three regions before assuming leadership of the National AIDS Programme. She’s seen the difference nutrition assistance makes for people and families on the brink. When people are worried about whether they will eat, they don’t take their treatment properly.
“Food insecurity creates a vicious cycle,” she said. “For people living with HIV it is important to have a healthy, balanced diet along with treatment to control the disease. But when someone doesn’t have food it affects them both mentally and physically. Adherence becomes an issue and the mental health impact also undermines the immune system.”
In the context of COVID-19, the food bank has expanded its reach to HIV-negative members of key populations. The National AIDS Programme is collaborating with community organizations to pair dissemination with the provision of information on COVID-19 and HIV as well as HIV prevention and testing services.
So far, more than 2700 food and personal hygiene packages have been distributed. Rather than have people journey to the food bank, the supplies are now being distributed through the treatment sites in their districts. An open invitation was issued to diagnosed people who hadn’t started or continued antiretroviral therapy to go to their nearest treatment centres for HIV medicines and food—two essentials for surviving COVID-19.
In 2019, Guyana became the first Caribbean country to introduce national nutrition and HIV guidelines. The strategy supports health-care providers, policymakers, social workers and other HIV response stakeholders in responding to the nutrition care and support needs of people living with HIV in diverse conditions. In an epidemic response often dominated by concerns around treatment, Guyana has been proactive about addressing the food insecurity challenge some people living with HIV face either consistently or—as is the case with COVID-19—in exceptional circumstances.
“HIV treatment will fail if people don’t have food—healthy food. The fact that Guyana has been able to respond immediately to alleviate food security challenges and thus protect the well-being of people living with HIV right from the outset of the humanitarian crisis demonstrates the value of making psychosocial support investments integral to our regular treatment programme,” Mr de Groulard said. “It makes countries and communities more resilient, more agile and better prepared to respond to crises.”
Region/country


Feature Story
“Do not guess, get tested” - Free testing for HIV, syphilis, and hepatitis B and C in Yerevan
27 August 2020
27 August 2020 27 August 2020In Yerevan, the capital of Armenia, all polyclinics are now providing free, anonymous, and fast testing for HIV, Syphilis, Hepatitis B and C as part of the “Do not guess, get tested” campaign launched by the Ministry of Health and the Yerevan Municipality on World Hepatitis Day.
“It is an important signal to the population that we keep providing all necessary HIV services to people and that the COVID-19 pandemic has not stopped our prevention and testing work,” said Alexander Bazarchyan, Director of the National Institute of Health.
In preparation for this initiative, the Ministry of Health together with the National Institute of Health and the Municipality of Yerevan, conducted training sessions for medical staff in 20 polyclinics in Yerevan. More than 300 health workers—family doctors, infectious disease specialists, general practitioners, laboratory specialists, etc—received theoretical and practical information on “Management skills of Tuberculosis, Hepatitis B and C” and “HIV testing and counselling services in primary healthcare facilities”.
The activities continued during the COVID-19 epidemic through an educational website developed with support from UNAIDS. The site is a platform where specialists can post accredited online courses so that health professionals can continue their education for free.
In addition, rapid tests for HIV, Syphilis, Hepatitis B and C were purchased within the framework of the UNAIDS Regional Cooperation Programme (RCP) for Technical Assistance on HIV and other Infectious Diseases funded by the Government of the Russian Federation. The RCP aims to strengthen health systems, ensure better epidemiological surveillance of HIV, and promote the scale up of HIV prevention programmes among key populations at higher risk in Armenia, Belarus, Kyrgyzstan, Tajikistan, and Uzbekistan.
“We welcome such timely support as this initiative can facilitate access to testing for people through primary healthcare services and make another step towards achieving Armenia’s commitments to increase access to early diagnosis and treatment,” said Roza Babayan, UNAIDS Representative in Armenia.
Region/country
Related




Feature Story
Sex work during COVID-19 in Tanzania
25 August 2020
25 August 2020 25 August 2020“After COVID-19 kicked in, it has been too difficult to get customers,” says Teddy Francis John, a sex worker from Zanzibar. Since the outbreak of COVID-19, she has faced increased difficulties to earn an income to provide for herself and her two children.
“Everything has become tough and I had to start a small business of selling alcohol—local brew,” she says. The business also helps her meet new clients, as they come to her for drinks and are less vigilant about social distancing guidelines.
Ms John used to live and work in Zanzibar town, but to better earn an income and avoid paying rent, she decided to move to a more rural area. Here, she says, she can more easily find new customers for her local brew.
Rehema Peter is facing a similar situation, just on the other side of the ocean on Tanzania Mainland. She lives in the crowded suburb of Temeke in Dar es Salaam and works as a sex worker and volunteers as a peer counsellor for people living with HIV and for people who use drugs.
Her clients were regulars who used to come to her house, or she would visit those she could trust in their homes. But when COVID-19 broke out, they stopped coming.
“Coronavirus made life very hard. Payment at work used to be little and when COVID-19 came it reinforced the situation. On the side of my partners [clients], they stopped visiting and calling me. The very few who used to visit me often, I called them, but they said they have no money because of COVID-19, as some stopped going to their jobs,” says Ms Peter.
At her job as a peer counsellor she was offered fewer shifts, meaning a lower income. Because she is a former drug user, she has received some support through the Tanzania Network for People who Use Drugs (TaNPUD), which has been supported by UNAIDS to distribute food and hygiene items to people who currently use drugs and people in recovery.
“I just try to be calm and find other means [of income]. I’m searching for additional organizations that can help or support me anyhow. I also try to prepare soap and oil from the knowledge that TaNPUD gave me and I sell it,” says Ms Peter.
Continued services
Both Ms Peter and Ms John are living with HIV and are on HIV treatment. Due to the advocacy and assistance of UNAIDS and other partners of the Tanzanian government, disruptions to HIV services have been minimal in the country. This is felt by both women.
“During this time, it has become difficult to get services in government health facilities; unless you go to a private hospital where you must have cash. However, there is no problem at all in getting HIV-related services, including my treatment,” says Ms John.
Ms Peter say she can now get three months multi-month dispensing of antiretroviral treatment—even up to six months—since the healthcare staff do not want congestion in the clinics. This has helped both women in adhering to their treatment.
Increased stigma
Both Ms Peter and Ms John have experienced an in increase in the stigma and social exclusion they also face as sex workers and as women living with HIV during the COVID-19 outbreak.
“As some people know that I am living with HIV, they tease me. They say ‘prepare yourself for death. People like you never heal. You must prepare for your final journey’” recounts Ms Peter. She has faced discrimination in the community, but her family stands by her.
Ms John also faced increased gossip and mocking of her because of her work.
“People in my surrounding communities started mocking me and others. They gossiped as to how I would earn a living as there are not going to be customers because of the COVID-19 outbreak.” Says Francis John
Despite the COVID-19 outbreak being declared over in Tanzania and despite their continued efforts to find other means of livelihood, earning an income is still hard for the two women, due to continued social distancing regulations.
“[It] has been very difficult to provide this service and this harmed us economically. I know COVID-19 has affected the whole world but it has affected sex workers more because of the nature of our services; it involves proximity,” says Ms John.













