Feature Story
Urgent action needed to address HIV in Haut-Mbomou, Central African Republic
15 April 2019
15 April 2019 15 April 2019On the border between South Sudan and the Democratic Republic of the Congo, Haut-Mbomou is the province worst hit by HIV in the Central African Republic, with HIV prevalence at 11.9% compared to a national average of 4%.
Initially spared by the conflict that engulfed the country in 2013 and 2014, since 2018 Haut-Mbomou has seen fighting between rival armed groups, continued insecurity and a large-scale displacement of people. More than 47 000 people have been displaced by insecurity and violence in the province, adding to a population of some 3500 refugees from South Sudan and the Democratic Republic of the Congo.
Alerted by accounts of persistent medicine stock-outs, substandard care for people living with HIV and barriers to access to HIV and health services owing to insecurity, a joint mission of the Central African Republic Ministry of Health, the National AIDS Council, the World Health Organization, the Office of the United Nations High Commissioner for Refugees and UNAIDS visited Haut-Mbomou from 8 to 12 April. Located 1000 km from the capital, Bangui, the province is among the most underserved by health and social services. Half of the health facilities in the province are closed owing to a lack of personnel or rundown facilities.
In the towns of Obo and Zemio, the mission met with local authorities, health-care providers, religious and community leaders, internally displaced people, refugees and people living with HIV. “This joint mission brings together the breadth of national and United Nations expertise to offer practical solutions to the challenges of HIV and health in this critical province,” said Patrick Eba, UNAIDS Country Director for the Central African Republic.
The mission noted the impact of insecurity on the population and on access to health and other services. The main routes of supply are closed and violence outside the urban centres greatly limits access to medicines, food and other essential commodities.
The Obo District Hospital, the main health-care facility in the province, lacks basic laboratory testing equipment, including for blood safety or tuberculosis screening. Access to antiretroviral medicines is greatly limited by regular stock-outs. The absence of CD4 count measurement, viral load testing and other biological tests for people on antiretroviral therapy limits the quality of care for host populations and refugees. The mission was also concerned by the absence of HIV prevention and sensitization efforts, including the unavailability of condoms.
“How can we live in dignity when we face constant stock-outs of antiretroviral therapy and the hospital staff treat us badly? Many people who are on treatment are sick with opportunistic infections, but the hospital cannot give us anything,” lamented a frail, middle-aged woman living with HIV in Obo, who also bravely spoke out against discrimination.
Access to food is increasingly a problem because insecurity limits farming, fishing and hunting and hinders the ability of humanitarian agencies to deliver nutritional support. For vulnerable people living with HIV, including refugees and displaced people, access to food and nutritional support is essential for antiretroviral medicine adherence and effectiveness.
In Zemio, the mission spoke with members of community groups established by Médecins Sans Frontières as part of an innovative programme to facilitate access to antiretroviral medicines. Group leaders collect and dispense antiretroviral medicine to members who live far from hospitals. The group members highlighted that barriers to their access to medicines included roadblocks, insecurity and extortion by armed groups. The mission held a dialogue with communities and leaders of the main armed group in Zemio to emphasize the need for unhindered access to health-care facilities.
The mission showed the complex nature of the challenges facing the HIV response in a context such as that in the Central African Republic, which is characterized by insecurity, population displacement and a collapsed health-care system. Those challenges call for urgent attention and action on the part of the government, the United Nations and others to address emerging and chronic health and HIV challenges. “Addressing these challenges is essential to show that these populations are not forgotten” said Wilfrid Sylvain Nambei, the Minister Coordinateur of the National AIDS Council. “Swift action following this mission will reinforce confidence in the government and its partners and it will advance our efforts to build peace, reconciliation and reconstruction that leaves no one behind.”
Region/country
Related



Feature Story
Côte d’Ivoire signals renewed will to tackle issue of user fees for HIV services
16 April 2019
16 April 2019 16 April 2019The Government of Côte d’Ivoire has signalled its commitment to stop people being charged for accessing HIV testing and treatment services, declaring that it will strictly apply previously announced decisions to prevent people living with or affected by HIV being asked to pay user fees.
A note circulated by the Ministry of Health has reminded all service providers that costs for HIV testing and treatment services should not be charged to people accessing those services. The directive applies for all services for pregnant and breastfeeding women, all HIV testing services, tests for viral load suppression and the prescription of antiretroviral medicines for people living with HIV.
The directive also reminds service providers that children under the age of 15 years should have free access to health services and that young women aged 15–24 years should have free access to primary health care, HIV testing and family planning services.
In several countries, the issue of user fees has been identified as a major barrier to testing people for HIV, to treating people living with HIV and to retaining people in treatment and care.
The renewed commitment of Côte d’Ivoire to confront the issue of user fees followed discussions between the President of Côte d'Ivoire, Alassane Ouattara, and the former President of Botswana, Festus Mogae, who visited the country in March in his capacity as Chairperson of the Champions for an AIDS-Free Generation in Africa.
Following their discussions, the government also announced its intention to increase domestic funding for the AIDS response by US$ 10 million in the next budget.
During his meeting with the President, Mr Mogae congratulated Mr Ouattara and the First Lady, Dominique Ouattara, for their personal commitment to ending the AIDS epidemic as a public health threat by 2030. Ms Ouattara is UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission and the Promotion of Paediatric Treatment of HIV.
At the conclusion of his mission, Mr Mogae underlined the importance of accelerating the response to the epidemic. “We cannot be complacent and allow the huge improvements that we have made so far to be lost. If we stop now, we will lose everything we have already invested and achieved. The entire nation must be mobilized to ensure that no one is left behind,” he said.
There were 500 000 people living with HIV in Côte d’Ivoire in 2017, with around 46% accessing HIV treatment.
Region/country


Feature Story
Cyclone Idai flood survivors ‘just want to go home’
18 April 2019
18 April 2019 18 April 2019Bangula settlement in Nsanje District, in the south of Malawi, is an arduous five kilometre walk from the border with Mozambique.
It is a walk that approximately 2 000 Mozambicans have made since they were displaced a month ago by the floods caused by Cyclone Idai. The settlement is also a temporary home to approximately 3 500 Malawians from surrounding villages who were also displaced.
Being predominately a small holder farming community, their homes, belongings and livelihoods were all washed away by the floods. They are now at Bangula, waiting for the earth to dry so they can go home and begin rebuilding their lives.
The emergency response to assist the 81 000 people in the district affected by the floods is being coordinated by the Government of Malawi, the United Nations, development partners and non-governmental organizations.
Upon arrival at the settlement, heads of households are provided with mats and blankets to sleep on and maize meal to cook.
Women and children are housed in 21 tents to the rear of the settlement, while others sleep under open industrial sheds, on concrete floors under tin rooves.
On a visit to the camp, Michel Sidibé, UNAIDS Executive Director, heard that while some amenities are being provided, there is not enough shelter for everyone and there is no lighting at night, which exacerbates vulnerabilities, especially of women and children.
It is well known that sexual and gender-based violence against women and children is heightened in emergency settings such as the one at Bangula. People also spoke of a lack of adequate nutrition, access to clean water and sanitation as well as their experiences of stigma and discrimination.
The small clinic at the settlement mostly focuses on primary health care and offers antenatal and postnatal services, HIV counselling and testing, refills of HIV treatment and psycho-social support.
While at the settlement Mr Sidibé spoke to a group of people living with HIV who had come to the settlement for shelter. They spoke of how, when the floods came, they tried to keep their HIV treatment safe from the water.
“When the floods came, my house was destroyed. But I managed to reach for my plastic bag where I keep my ARVs, because it is one of my most precious possessions,” said Sophia Naphazi, who resides in Jambo village in the district.
Elizabeth Kutenti, another women living with HIV, spoke of how her pills were safe because she keeps them in the roof. “They are my life,” she said.
The support people at the settlement need to return home is modest. “We need three things: a plastic sheet to cover what is left of our homes; maize seeds to plant and a hoe. Then we can go home,” said Miliam Moses.
“The level of resilience I have seen today is just amazing,” said Mr Sidibé. “The most important message I have heard today is one of hope.”
Mr Sidibé was accompanied by Atupele Austin Muluzi, Minister of Health and Population in Malawi. He thanked the UN agencies and the government departments supporting coordinating in the emergency response.
“We need continued support so that all the people in this settlement get the help they need so they can return home and live in dignity,” he said.
Region/country
Related

Feature Story
Women lead to reduce the impact of HIV and gender-based violence in the Middle East and North Africa
23 April 2019
23 April 2019 23 April 2019According to the World Health Organization, about one third of women worldwide have experienced violence. In some regions, women who have experienced physical or sexual intimate partner violence are 1.5 times more likely to acquire HIV than women who have not experienced such violence. Among marginalized populations, such as sex workers or transgender women, a high prevalence of violence is linked with higher rates of HIV infection.
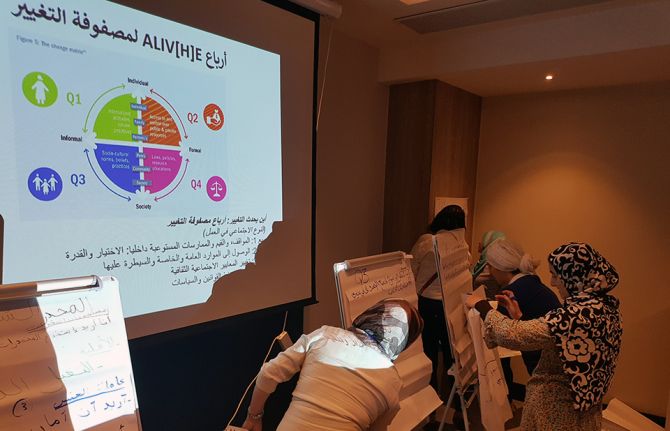
In the Middle East and North Africa (MENA) region, UNAIDS estimates that around 220 000 people are living with HIV. New infections were up by 12% between 2010 and 2017 and AIDS-related deaths increased by 11% over the same period. The stigma and discrimination associated with HIV as well as high levels of gender-based violence are preventing several countries from making progress against the epidemic. Gender-based violence in the region is strongly associated with harmful gender norms and stereotypes.
In 2018, the LEARN MENA project was launched to provide women with a platform to share experiences and explore the linkages between gender-based violence and HIV in the region. Underpinning the project is the Action Linking Initiatives in Violence against Women and HIV Everywhere (ALIV(H)E) framework, a research project that collates evidence on what works to prevent violence and builds women’s awareness to understand and address linkages between violence against women and HIV.
Through community dialogues led by MENA-Rosa, a regional network of women living with or affected by HIV, women are strengthening their own understanding of the root causes of violence and the links with HIV. The dialogues have highlighted the fact that gender inequality is at the centre of violence against women and an increased risk of HIV infection. For example, through the dialogues it was revealed that some women had never been to school. Many had experienced early or forced marriage. Many women acquire HIV from sexual violence, including within their own marriage.
“Violence is everywhere. Over time, and as you get older, you get to see it as normal,” said an Algerian woman participating in one of the dialogues.
The participants described multiple forms of violence across different settings, including in health-care settings, which impede their access to health care, including to HIV prevention and treatment services.
So far, the project has been implemented in seven countries―Algeria, Egypt, Jordan, Lebanon, Morocco, Sudan and Tunisia.
Findings from the project are helping women living with and affected by HIV to advocate for an improved response to the epidemic in the region and for measures to reduce the impact of violence against women. The dialogues have amplified the voices of marginalized women living with and affected by HIV, encouraging decision-makers and partners to build strengthened national community responses. UNAIDS is supporting countries to implement the recommendations and action plans developed from the project.
“MENA-Rosa leaders have learned through this painful process that violence against us should be denounced and not brushed under the carpet,” said Rita Wahab, Regional Coordinator of MENA-Rosa. “Empowerment will help women in all their diversity to know and understand their rights. Our advocates will move forward to expose the links between violence against women and HIV. Gender equality starts at home, grows in society and blossoms in the legal environment.”
LEARN MENA is implemented by UNAIDS, Frontline AIDS and MENA-Rosa, with funding support from USAID. Additional technical support is provided by the Salamander Trust, the lead author of the ALIV(H)E framework.


Feature Story
Scaling up stigma-free services for women in Egypt
11 April 2019
11 April 2019 11 April 2019When the family and neighbours of Salma Karim (not her real name) found out that she was living with HIV they chased her out of her home. With nowhere to go, she was forced to leave her two young children behind. This is not an uncommon story in Egypt. One in five people living with HIV report being forced to leave their homes by their landlords, family or neighbours.
High levels of stigma and discrimination are one of the key factors driving new HIV infections in the country, which doubled between 2010 and 2016. Women and adolescent girls are often the most vulnerable. Societal norms, gender inequality, economic dependence, legal discrimination and harmful practices affect them disproportionately, making them more vulnerable to HIV and facing greater levels of stigma and discrimination in the event of HIV infection.
In 2016, UNAIDS in partnership with the Egyptian Ministry of Health and Population joined efforts towards a gender-transformative response to the HIV epidemic. With funding from the Dutch government, a pilot project called Enhancing Sexual and Reproductive Health of Women Living with and Affected by HIV was launched. Three years later, the pilot has reached double its intended beneficiaries with stigma-free quality sexual and reproductive health services.
“I lost my first child as I didn’t know I had HIV,” explains Nour Tarek (not her real name). It was in one of the pilot project sites in Giza that she received the support to realize her reproductive rights free from discrimination. “I followed up with the doctor in the hospital and I became pregnant again.”
Thanks to the antiretroviral medicine she received while pregnant, her baby Mona (not her real name) was born HIV-negative. “I still have to test again until she is older to make sure she is fine,” explains Ms Tarek.
Having proved its success, the pilot project is now being scaled up to a third of the country’s governorates. The aim is to deliver high-quality sexual and reproductive health and HIV services for 1300 women living with HIV and 3000 women at higher risk of acquiring HIV. Its focus on building the capacity of health-care providers and civil society organizations will be key to avoiding future stigma and discrimination, which is reported to lead one in four people living with HIV in Egypt not to disclose their HIV status when seeking care.
During his visit to Cairo on 9 April, the Executive Director of UNAIDS, Michel Sidibé, and the Ambassador of the Netherlands to Egypt, Laurens Westhoff, discussed the expansion of the project. Implemented through a new three-year Dutch grant, the scaled-up services will complement national efforts to achieve Egypt’s ambitious new National AIDS Strategy 2018–2022 and the Sustainable Development Goals.
Region/country

Feature Story
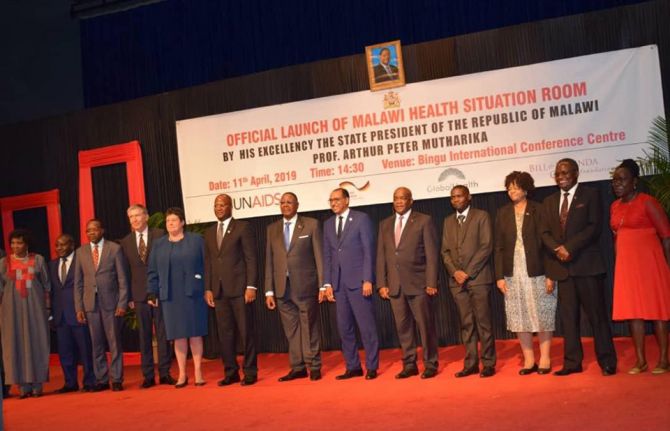
Malawi launches its health situation room
12 April 2019
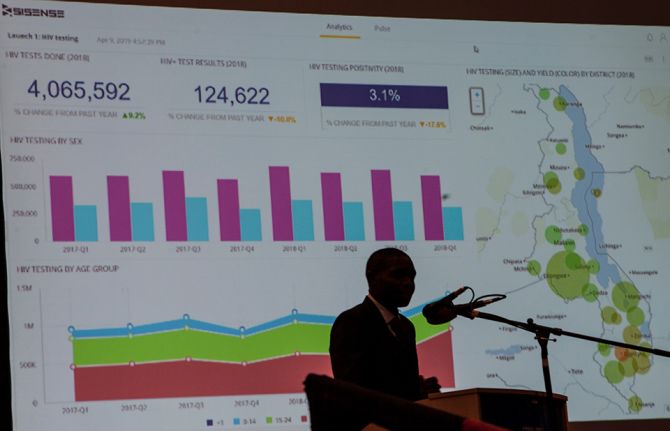
12 April 2019 12 April 2019Malawi has become the latest country to launch a health situation room, a software platform designed to help the government make informed decisions about policies and programmes related to health, including HIV.
The innovative tool bolsters national information systems through real-time visualization of information from multiple data sets. It will enable leaders and programme managers to improve health programmes to achieve the 90–90–90 targets, whereby 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads by 2020.
Malawi is making good progress in its response to HIV. In 2017, 90% of people living with HIV in the country knew their status, 71% of people living with HIV had access to treatment and 61% of people living with HIV had a suppressed viral load. Around 1 million people are living with HIV in Malawi, with new HIV infections in 2017 down by 40% since 2010. However, HIV infections among young women and adolescent girls aged 15–24 years remain high and account for more than one in four new infections per year.
In his speech at the launch of the health situation room in the capital, Lilongwe, the President of Malawi, Arthur Peter Mutharika, said the tool was an important step forward.
“The health situation room is a demonstration of my government’s commitment towards accountability and transparency,” said Mr Mutharika. “My desire is that the health situation room will show us where to focus to improve even further in our quest for a healthier Malawi.”
The Executive Director of UNAIDS, Michel Sidibé, said the launch would strengthen the country’s health sector.
“The health situation room is an important innovation as it shares real-time data to improve the understanding of the country’s HIV epidemic and other health challenges,” said Mr Sidibé at the launch. “It will guide Malawi’s response and help officials to close the gaps, ensuring that no one is left behind as the country gets on track to end the AIDS epidemic by 2030.”
Region/country
Related
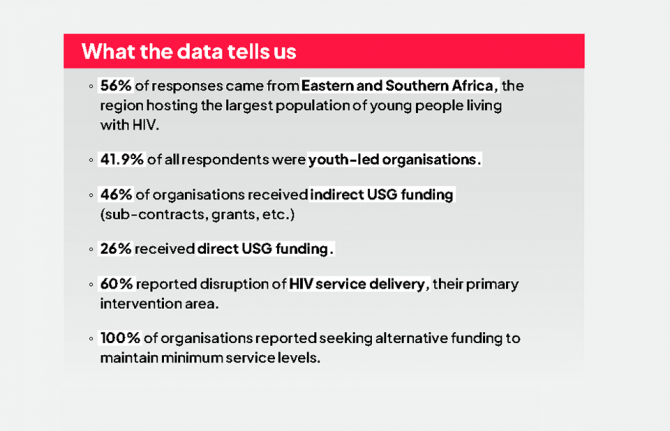
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025
 Impact of US funding cuts on HIV programmes in Malawi
Impact of US funding cuts on HIV programmes in Malawi

15 April 2025


Update
Parental consent is required in the majority of countries worldwide
15 April 2019
15 April 2019 15 April 2019While the intention of age of consent laws for medical services is often to protect children, in practice such laws do the opposite, by discouraging adolescents from accessing the services they need to stay healthy.
Age of consent laws for medical services require people aged younger than 18 years to obtain permission from a parent or guardian before accessing sexual and reproductive health services, HIV testing and treatment, pre-exposure prophylaxis and other health services. They particularly affect adolescent girls, whose sexuality tends to be stigmatized and who bear the physical and social burdens of unwanted pregnancies.
In 2017, 78 of 110 reporting countries stated that they required parental consent for a child under 18 years to access HIV testing, and 61 of 109 reporting countries required parental consent for HIV treatment. In addition, 68 of 108 reporting countries required parental consent to access sexual and reproductive health services.
Related information
Related


Update
Giving young people the knowledge to stay healthy
23 April 2019
23 April 2019 23 April 2019Comprehensive sexuality education plays a central role in preparing adolescents and young people for a safe, productive and fulfilling life, and it is an important component of an HIV prevention package for young people. It provides opportunities to learn and acquire complete, accurate, evidence-informed and age-appropriate knowledge on sexuality and sexual and reproductive health issues.
Comprehensive sexuality education―defined as a curriculum-based process of teaching and learning about the cognitive, emotional, physical and social aspects of sexuality―have been shown to contribute to delayed initiation of sexual intercourse, decreased frequency of sexual intercourse, decreased number of sexual partners, reduced risk taking, increased use of condoms and increased use of contraception among young people.
Despite the importance of comprehensive sexuality education, however, access to it is far from universal.
Related information
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025


Feature Story
Liberia’s catch-up plan takes shape
27 March 2019
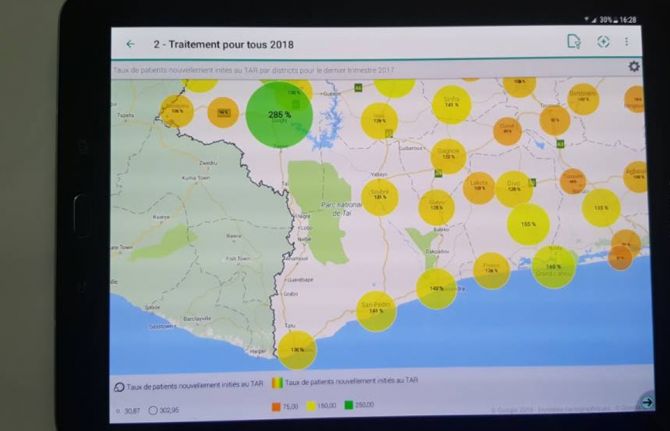
27 March 2019 27 March 2019The HIV epidemic continues to have a profound humanitarian and public health impact in western and central Africa, a region that risks being left behind in the global response to ending the AIDS epidemic. In July 2017, the African Union endorsed a regional catch-up plan for western and central Africa that seeks to rapidly accelerate access to HIV treatment and close the gap between African regions. National catch-up plans have been established in 18 countries in western and central Africa, including in Liberia.
It is estimated that in 2017, 40 000 people were living with HIV in Liberia, including around 3000 children aged 0–14 years. Fewer than one in three adults aged 15–49 years who are living with HIV have access to medicines that would keep them well and stop them passing on the virus to other people. For children, the situation is even more challenging, with just 18% on treatment.
However, there are encouraging signs that Liberia is scaling up its response to the HIV epidemic and adopting best practice programmes and policies to ensure the delivery and take-up of HIV testing, treatment and prevention services. Under the leadership of the Ministry of Health and the National AIDS Commission of Liberia, a Fast-Track plan for 2019–2020 has been developed that identifies high-impact programmes to accelerate the response, the urgent need for adjustments to existing programmes and barriers that must be removed in order to ensure better service delivery. It also recognizes that prevention measures must be reinforced and that stigma and discrimination associated with the virus must be reduced.
The Liberia catch-up plan seeks to triple the country’s test and treat figures, whereby people who test positive for HIV are immediately referred for treatment. The catch-up plan is guided by a location–population approach, with a service delivery bias towards the three counties with the highest unmet need for HIV testing, treatment and care services, urban areas and some other locations. Services are oriented towards adults aged 15–49 years, especially to pregnant women and to groups at higher risk, such as gay men and other men who have sex with men, sex workers, people who inject drugs, prisoners and mine workers. Infants exposed to the virus during pregnancy and breastfeeding are also a priority.
The plan also aims to tackle the low take-up of services by men.
“We are designing interventions that will encourage more men to test and know their status. Of those tested so far, 80% are women,” said the National AIDS Commission of Liberia Chair, Theodosia Kolle. “Stigma remains a major issue in Liberia.”
UNAIDS played a significant role in helping to draft the catch-up plan, mobilizing stakeholder involvement and ensuring that people living with HIV, civil society and members of key populations were included in order to shape its design. Around 70 people took part in a special two-day workshop in March to craft the necessary political and programmatic measures to improve service delivery, enhance community mobilization, increase funding and enable a more efficient use of existing resources and an improved monitoring and evaluation system.
The workshop was also an opportunity to validate the Global AIDS Monitoring (GAM) report for 2019 for Liberia. GAM is the world’s most extensive data collection on HIV epidemiology, programme coverage and finance and publishes the most authoritative and up-to-date information on the HIV epidemic—vital for an effective AIDS response.
“With teamwork we can reach the 2020 Fast-Track Targets as long as we prioritize and implement high-impact programmes,” said Miriam Chipimo, UNAIDS Country Director for Liberia.
The 90–90–90 targets included in the Fast-Track approach are that, by 2020, 90% of all people living with HIV will know their status, 90% of all people living with HIV will have access to antiretroviral therapy and 90% of all people on antiretroviral therapy will have viral suppression.
Region/country


Feature Story
Meet Marlo: the go-to source of information about HIV
29 March 2019
29 March 2019 29 March 2019Discussions about sex and HIV in Indonesia remain highly taboo, while the limited information that exists is often unclear, not easy to digest or contradictory. That’s why many young people are turning towards new technology platforms to seek answers to questions that affect their health and well-being.
In an attempt to improve the quality of information provided to young people, the UNAIDS Country Office in Indonesia has developed Tanya Marlo, or Ask Marlo, a chatbot powered by artificial intelligence and designed to be the go-to source for all things HIV-related.
Marlo is a cute character who provides basic information about HIV through user-friendly content such as infographics, quizzes and FAQs (frequently asked questions). In just a few taps, Ask Marlo users can also book HIV testing appointments at health centres across Jakarta, Indonesia. Young people looking for a more in-depth chat are connected to real counsellors, who are on standby to talk, provide guidance and make referrals to specialized services.
The counsellors receive many questions on how to access HIV services and HIV treatment.
“Many people, particularly young people, in Jakarta still do not know basic information about HIV. I hope that as a counsellor on Marlo, I can change that,” one of the counsellors said.
The Ask Marlo chatbot is integrated into the LINE chat messaging application. Users looking to chat to Marlo can simply add @tanyamarlo on LINE and begin chatting. Indonesia is one of LINE’s top markets, with around 90 million users. Around 80% of its users are young people, many of whom use LINE Today to get news and information and to shop.
Since launching on 1 December 2018, Ask Marlo has increased the number of its users, reaching almost 3000 followers at the end of March. Reviews of Ask Marlo bear witness to how important and necessary the service is for young people.
Upon seeing Ask Marlo for the first time, a psychology graduate from the University of Indonesia said, “It is so youth-friendly! My friends and I use LINE a lot, so this is the perfect platform for Ask Marlo. I am surprised that a chatbot can be used to teach about things as complex as HIV.”
A university student at the Atma Jaya University likes the anonymity provided by the application. “With Ask Marlo, we don’t have to be ashamed to ask anything related to HIV.”
University students, young professionals, communities, civil society activists and the Ministry of Health have endorsed Ask Marlo. Besides students and young professionals, several social media influencers and YouTube personalities have also given their stamp of approval. Their endorsement of Ask Marlo has helped to promote the chatbot to wider audiences. The idea is to eventually expand to offer testing in other major cities across Indonesia.