Feature Story
There is life after HIV, there is love
08 March 2019
08 March 2019 08 March 2019Mandisa Dukashe was nervous before she took an HIV test in 2002. As a nursing student in South Africa, where more than 4 million people were living with HIV at the time, she knew it was possible that she would test positive for the virus. “I was very stressed,” she says. “I kept postponing the test.”
Ms Dukashe had learned about HIV during her university studies, so the staff at the clinic assumed that she was well informed and didn’t need pretest counselling. “They told me I am a nursing student and should know what it entails.”
The test result was positive. Ms Dukashe joined 510 000 other South Africans who became newly infected with HIV in 2002—20% of all new infections worldwide.
When Ms Dukashe was diagnosed with HIV, South Africa had only recently started to roll out treatment and it was five years before she got access to it. It was harder to come by then, with limited medicine formulations that were only prescribed for people falling ill with an AIDS-related illness.
In 2002, South Africa had more than 4 million people living with HIV but fewer than 15 000 people receiving treatment through public facilities. That year the country also recorded more than 190 000 AIDS-related deaths.
The picture today is much improved.
Ms Dukashe and her family featured on the cover of the 2018 UNAIDS World AIDS Day report, Knowledge is power, as living proof that sustained HIV treatment can suppress a person’s viral load and prevent the transmission of HIV to a partner and children. “This can be done by anyone,” she says.
In 2017, there were more than 4.3 million people on HIV treatment and 110 000 AIDS-related deaths in South Africa. Yet there are still miles to go to end the AIDS epidemic by 2030. South Africa continues to rapidly scale up HIV treatment and is determined to reduce annual AIDS-related deaths to 80 000 or fewer by 2020.
Ms Dukashe says it didn’t take long to reconcile herself to her HIV-positive status. She was determined to embrace her status, look after herself and spread the word. She wanted to warn other young people to avoid HIV infection, take a test and seek support if they tested HIV-positive. “After the counselling, I felt so bold and confident and I was ready within a week to go out and tell the world with an intention of raising awareness, in particular among young women and adolescent girls.”
“At first I didn’t want to reveal my HIV status because I knew that it could be an issue, so I focused on my nursing studies. Eventually I fell in love with a guy and I feared he would reject me, but I had to tell him—I cannot live a lie."
But things were not always easy for her. Ms Dukashe was married when she was diagnosed. “Some people say that HIV can bring you closer, but that wasn’t to be.” They eventually divorced and it took time before Ms Dukashe found love again. “At first, I didn’t want to reveal my HIV status because I knew that it could be an issue, so I focused on my nursing studies. Eventually I fell in love with a guy and I feared he would reject me, but I had to tell him—I cannot live a lie. It took me three months to disclose my status, but to my surprise his response was much better than I hoped. He remains HIV-negative and he is the best husband and father of my children that I could ever ask for. When you have got that kind of support you can live healthily and even forget about HIV.”
Despite the love and support of her husband and family, the weight of living with HIV came flooding back to Ms Dukashe when she and her husband started planning to have children. “When the time came for us to talk about preventing HIV transmission to our children, we needed to think carefully, plan and consult medical experts. That brought it all back for me and I got depressed for a while.”
But help was available, she says. “I got counselling and worked through those feelings and it was all worth it. I now have two wonderful children who were born without HIV. It was my responsibility and also my husband’s responsibility. We got great support and advice.
“Being able to give birth to HIV-negative children was a blessing because I believe if I did not test, my kids could have been born with HIV.”
Ending new HIV infections among children is a high priority for South Africa, with a target of virtual elimination by 2020. Yet despite many years of concentrated effort, 13 000 children acquired HIV from their mothers in 2017. “It pains me that I could not breast-feed my babies,” says Ms Dukashe. “Because I wanted so hard to prevent them from getting HIV I fed them with formula milk, which made me sad.”
Thanks to improved treatment options, women living with HIV are now encouraged to take HIV treatment for their own health and to avoid their children becoming infected during pregnancy, birth or breastfeeding. All breastfeeding women in South Africa living with HIV and on HIV treatment are encouraged to exclusively breastfeed until their baby is at least six months old.
Ms Dukashe is now working as a project manager for point-of-care HIV testing and quality assurance. She is also a motivational speaker, creating demand for HIV testing and treatment, including among women of child-bearing age and their partners.
“Being able to give birth to HIV-negative children was a blessing because I believe if I did not test, my kids could have been born with HIV.”
“I want to encourage everybody in our situation: there is life after HIV, there is love. People should not think twice about going for an HIV test. It was the best decision I ever made, since I learned what to do to keep myself healthy and prevent transmission to my spouse and children. Thinking twice is not going to change the result.”
“As a healthcare professional, it is important for me to show that I am living positively with HIV and managing it successfully. My experience should encourage others to protect themselves and get tested regularly. If you test positive for HIV, start treatment and get counselling and support so you can keep yourself healthy and protect others. HIV is, unfortunately, a reality for millions of people, but treatment works and we are stronger than HIV.”
Finally, Ms Dukashe has a message for young women: “HIV is invisible. Always use a condom and be wary of older men. Age-disparate relationships are a risk. If you rely on an older partner and try to please them, you won’t be able to insist on using a condom,” she said. “I speak from experience, as someone who faced the same pressures.”
Region/country
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala

22 December 2025





Feature Story
International Women’s Day in Ethiopia
12 March 2019
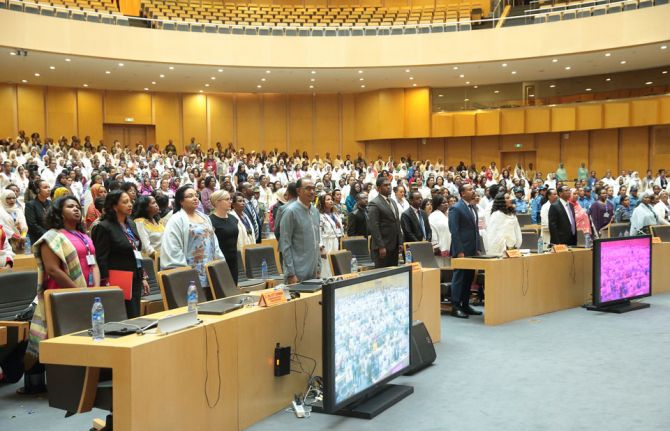
12 March 2019 12 March 2019The UNAIDS Executive Director, Michel Sidibé, celebrated International Women’s Day in Addis Ababa, Ethiopia, at an event organized by the Ministry for Women, Youth and Children Affairs and supported by UNAIDS. The event brought together female leaders and representatives of women’s associations from all over the country. Addressing the meeting, the Prime Minister of Ethiopia, Abiy Ahmed, emphasized that women are the “pillars of the nation.”
Yalem Tsegaye, the Minister of Women, Children and Youth Affairs, outlined the Jegnit initiative. Jegnit means “heroine” and is an innovative movement led by the Government of Ethiopia to empower and bring more women to leadership positions, both at the community and political levels.
During the event Mr Sidibé congratulated the Prime Minister and the Government of Ethiopia for its bold reforms in addressing the gender gap by appointing women to leadership positions in all sectors. He commended the Prime Minister for ensuring gender parity in his Cabinet.
“It is time to empower women and girls, because ending AIDS is as much about righting power imbalances as it is about health. This means prioritizing girls and young women in true partnership with them. It means providing adolescents girls and young women with more options and real choices,” said Mr Sidibé.
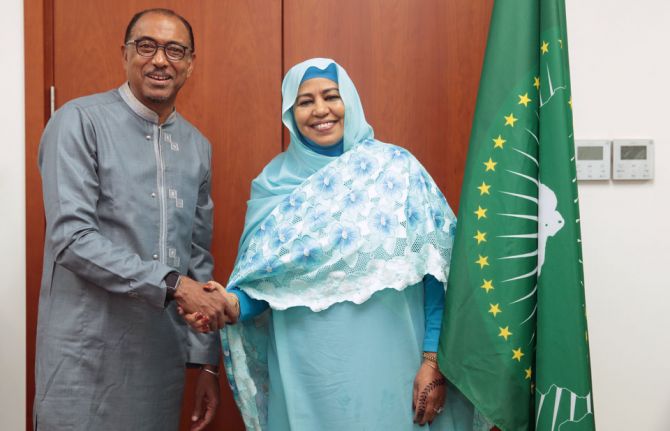
While in Addis Ababa, Mr Sidibé met with Vera Songwe, Executive Secretary of the United Nations Economic Commission for Africa, the first woman to hold the post in 60 years, to discuss ongoing collaboration on sustainable AIDS responses across the African continent.
Mr Sidibé also met with Amira Elfadil of the Department of Social Affairs of the African Union. In 2019, UNAIDS and the African Union are celebrating 20 years of a partnership focused on ending the AIDS epidemic across Africa.
Region/country
Related





Feature Story
Africa — Achieving health coverage without compromising on quality
08 March 2019
08 March 2019 08 March 2019Momentum for Universal Health Coverage (UHC) in Africa is building and many African countries have already integrated UHC into their national health strategies. But with 11 million Africans pushed into extreme poverty each year because of out-of-pocket health expenses, how can Africa achieve UHC which delivers a quality package of care for people living in Africa?
The UHC debate was buzzing in Rwanda’s capital Kigali this week during one of the largest health gatherings in Africa, the Africa Health Agenda International conference 2019. Co-hosted by the Ministry of Health of Rwanda and the African Medical and Research Foundation (Amref Health Africa), 1500 health leaders shared new ideas and home-grown solutions to the continent’s most pressing health challenges.
Participants discussed the need for countries to embrace the concept of UHC and do their utmost to make it work. They stressed that good health allows children to learn and adults to contribute to societies and the economy. They also underscored that it can allow people to emerge from poverty and provides the basis for long-term economic security, essential for the future of the continent.
Host country President, Paul Kagame was awarded the honour of excellence in recognition of his political leadership on UHC. In a tweet he thanked Amref saying, “We owe this progress to partners like you who have joined forces with us in our journey to deliver a dignified and healthy life for all Rwandans.” The Minister of Health of Ethiopia also received an award for Ethiopia’s work in promoting primary health care.
Ensuring that everyone has access to basic health services is a challenge and the key to the success of UHC will be ensuring that the quality of services is good enough to improve the health of the people who access them.
“We need to track the impact of UHC,” said Michel Sidibé, co-moderating a high-level ministerial panel. “Coverage is not enough, we need to be delivering quality, affordable, accessible services to all. The ultimate measure of success for UHC will be whether the poorest, the marginalized and the most vulnerable people are able to benefit.”
During the conference Mr Sidibé participated in a townhall with young people. He spoke to them about their meaningful engagement in the UHC process saying that young people need to ‘claim and own the space.’ He also talked to civil society groups about the remarkable progress towards achieving the UNAIDS 90-90-90 treatment targets across Africa and of the critical need of their continued engagement on HIV within UHC.
The first ever United Nations High-Level Meeting on Universal Health Coverage will take place on 23 September 2019 during the United Nations General Assembly under the theme ‘Universal Health Coverage: Moving Together to Build a Healthier World.’
Region/country

Feature Story
Burkina Faso piloting PrEP
08 April 2019
08 April 2019 08 April 2019For the past four months, Benjamin Sana has been regularly attending the Oasis Clinic in Ouagadougou, Burkina Faso, where he sees a doctor who gives him a full check-up.
The doctor and peer educators also check whether Mr Sana has any questions regarding his pre-exposure prophylaxis (PrEP) regimen. PrEP is taken by people who are HIV-negative but at higher risk of infection, and has proved to be very effective at keeping people free from HIV.
“Two plus one plus one,” answers Mr Sana, referring to when he needs to take the pills—two pills two hours before sex, then one the day after and one again the following day or one a day until his last sexual encounter. After his check-up, the 34-year-old gay man said, “PrEP protects me and I feel reassured.” He still uses condoms and lubricant, but when he doesn’t he said he feels safer.
Mr Sana is one of 100 men taking part in the PrEP pilot project at the Oasis Clinic, run by the Association African Solidarité (AAS). Health clinics in Côte d’Ivoire, Mali and Togo are also taking part in the pilot project, which has been running since 2017.
Camille Rajaonarivelo, a doctor at AAS, said that PrEP is part of a combination prevention approach that also involves trained peers from his community. The project will gauge adherence to treatment and whether participants take PrEP correctly, she explained.
“The final aim of this pilot project is to scale up and roll out PrEP nationally once the authorities give the green light,” she said.
The study aims to evaluate whether the preventive option gains traction and how feasible it would be to roll it out nationally and regionally. Financed by the French National Agency for Research on AIDS and Expertise France in partnership with Coalition PLUS and three European health institutes, the pilot project will provide data and ascertain if the treatment lowers the number of new HIV infections among gay men and other men who have sex with men.
Burkina Faso does not penalize homosexuality, but stigma against it is high. As a result, gay men and other men who have sex with men often hide their sexuality and tend to avoid health services. HIV prevalence in Burkina Faso among gay men and other men who have sex with men stands at 1.9%, more than double the rate among the general population.
The first definitive results of the PrEP pilot project in Ouagadougou should be available in 2020. Mr Sana said that many of his friends had shown interest in taking PrEP. “Because the pilot project has limited participants, a lot of people have been turned away,” he said.
He believes that PrEP will save lives, especially those of young men. “Nowadays, young men take a lot more risks and they don’t protect themselves,” Mr Sana said. Ms Rajaonarivelo agreed and added that this applies to young men and young women. “I am stunned to see new cases of HIV every week,” she said. “We have to beef up HIV prevention and awareness again.”
Special page
Region/country

Feature Story
People living with HIV face major challenges in Zimbabwe
08 March 2019
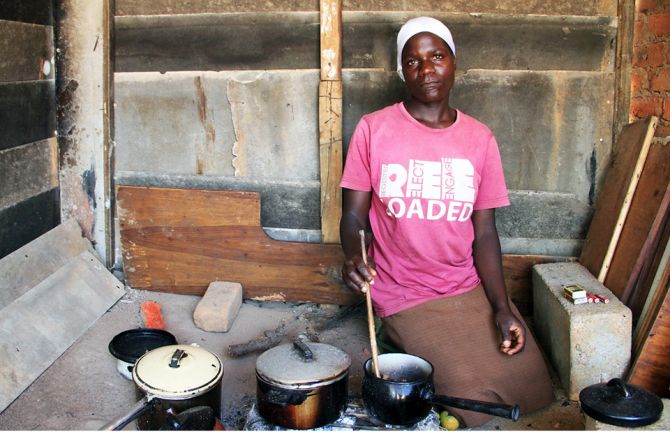
08 March 2019 08 March 2019According to a recent emergency appeal from the United Nations, around 5.3 million people in Zimbabwe are estimated to be in need of urgent humanitarian assistance.
The ongoing economic crisis, compounded by erratic weather conditions in recent years, has led to increased food insecurity and a lack of access to basic essential services, including health care. The appeal is requesting a total of US$ 234 million, including US$ 37.4 million for urgent health needs, to help 2.2 million of the worst affected. The appeal aims to complement Zimbabwe’s ongoing and planned programmes.
Erratic weather conditions, including late onset of rains and below-average rainfall, are affecting farmers and pastoralists across southern Africa, including Zimbabwe. This in a region where agriculturalists are still recovering from a severe El Niño induced drought in 2015/2016. Unpredictable rainfall patterns and a lack of pasture has weakened livestock and outbreaks of crop pests and livestock diseases are prevalent in many districts.
The deteriorating humanitarian situation and the country’s worsening economic circumstances, including currency volatility, are adding to an already difficult situation for Zimbabwe’s 1.3 million people living with HIV.
Household food insecurity and limited access to hygiene, sanitation and water can have a disproportionate impact on people living with HIV. HIV medication should not be taken on an empty stomach. Attacks of severe diarrhoea, cholera or other gastrointestinal infections can accelerate progression to serious AIDS-related illnesses if left untreated. In 2018, Zimbabwe recorded its second biggest cholera outbreak in its recent history. The country is also facing thousands of cases of typhoid fever.
Meanwhile, the lack of access to foreign exchange has significantly reduced stocks of essential medicines, diagnostics and other medical supplies. Some private pharmaceutical suppliers now only accept United States dollars and their prices have dramatically increased. In these circumstances, many people, including people living with conditions such as HIV and tuberculosis, are unable to pay for medicines and basic health services. Where clinics do have availability, many people cannot afford the cost of transport. Lack of adherence to treatment puts patients’ health at risk and may lead to drug resistance.
The fragile situation in Zimbabwe also increases the risk of HIV infection, especially for women and girls, refugees and the internally displaced. During periods of humanitarian emergency, where populations are on the move, girls are particularly vulnerable to family separation, early marriage, teenage pregnancy, gender-based violence and extreme coping mechanisms, including transactional sex.
“UNAIDS is very concerned about the worsening humanitarian situation in Zimbabwe, where people living with HIV are disproportionately affected by food insecurity and shortages of essential medicines,” said UNAIDS Executive Director, Michel Sidibé. “UNAIDS stands ready to work with all national and international partners to ensure that we mitigate the effects of the current situation so that people can access essential services, including HIV treatment and prevention services.”
Learn more
Region/country
Related

Feature Story
Turning words into action for gender equality
07 March 2019
07 March 2019 07 March 2019The second annual Global Health 50/50 report was launched on 7 March in Addis Ababa, Ethiopia. The report reviews progress made over the past 12 months by organizations active in the health sector to implement policies that promote gender equality, non-discrimination and inclusion in the workplace.
This year’s report, Equality works, reviews the gender-related policies and practices of almost 200 organizations. The sample includes organizations from 10 sectors, headquartered in 28 countries across the world that together employ an estimated 4.5 million people.
The report provides a comprehensive guide to how far global organizations active in health are taking steps to promote gender equality across four areas: commitment, evidence-informed policy content, equitable outcomes in power and pay and gender-responsive programming.
The Global Health 50/50 review identifies 14 organizations as very high scorers across these four areas, including UN Women, the United Nations Development Programme and the United Nations Population Fund. UNAIDS is included in a list of a further 17 organizations identified as high scorers.
However, the report stresses that even among good performers, there remains an urgent need for organizations to live up to and put into practice their stated policies on equality, non-discrimination and inclusion.
Ethiopia’s President, Sahle-Work Zewde, was the keynote speaker at the launch and spoke of the need to promote female leadership to implement policies and programmes that foster gender equality.
Ms Sahle-Work is Ethiopia’s first female head of state and currently the only female head of state across Africa. Ethiopia’s Prime Minister, Abiy Ahmed, has ensured gender parity among his cabinet ministers.
Speaking at the launch of the report, Michel Sidibé, UNAIDS Executive Director, said it was fitting that the event was taking place in Ethiopia and spoke of the importance of reaching gender equality as a matter of social justice.
“Women continue to be left behind and are more likely to face harassment and discrimination and slower career progression,” said Mr Sidibé, “It is an outrage that on average women today earn 20% less than men for no reason other than their gender. This must change.”
Mr Sidibé said UNAIDS had made progress on gender parity but acknowledged there was more to be done. He said that UNAIDS had increased the proportion of female country directors from 26% in 2013 to 48% today. He also pointed to the introduction of a single parental leave policy and the expansion of the UNAIDS Leadership Programme to all women in the organization as examples of its commitment to reaching gender equality.
Report

Feature Story
State of Gujarat establishes Transgender Welfare Board
26 February 2019
26 February 2019 26 February 2019In a landmark ruling in April 2014, India’s Supreme Court introduced recognition of a third gender and directed that transgender people must have access to the same rights to social welfare schemes as other minority groups in the country.
Now, the State of Gujarat has established a Transgender Welfare Board to increase access to essential services for transgender people, including to health care, housing, education and employment. The Ministry of Social Justice and Empowerment created the board following consultations with the transgender community and community groups, including the Lakshya Trust and Vikalp. UNAIDS and the United Nations Development Programme provided technical support and guidance throughout the process.
The new board aims to improve cross-departmental coordination to improve the delivery and provision of services for the transgender community. The 16-member board will include 8 civil society representatives, including representatives from the third gender community and will be chaired by the Minister for Social Justice and Empowerment.
"The new welfare board is a great effort to help in day-to-day issues faced by transgender people. We hope that issues of livelihood, employment, social security and the protection of human rights will be addressed by the board," said Aakriti Patel of the Lakshya Trust.
Part of the board’s work will be to work on the development of an agreed legal definition of who can be designated as transgender.
“UNAIDS looks forward to working with the new Transgender Welfare Board in Gujarat. I applaud the ministry and all partners for the work they have done in helping to create the board, which will greatly improve the lives of the transgender community,” said UNAIDS Country Director for India, Bilali Camara.
UNAIDS will continue to provide support to the board with the development of a policy road map and the roll-out of social protection programmes for transgender people. UNAIDS is also working with the private sector in Gujarat to provide skills training for around 3000 transgender people.
In India, HIV prevalence among transgender people is 3.1%, compared to the national HIV prevalence among all adults of just 0.2%.
Region/country




Feature Story
Young people change the narrative on HIV in South Africa
26 February 2019
26 February 2019 26 February 2019Colour my HIV is an HIV prevention and empowerment campaign led by and focused on young people in South Africa. It was launched on World AIDS Day 2018 in Johannesburg, South Africa.
The aim of the campaign is to create an information platform to debunk myths and misconceptions about HIV in order to reduce HIV-related stigma and discrimination, increase knowledge of HIV by presenting new findings by experts and researchers, promote human rights, advocate for political commitment and accountability by policy-makers and other partners and highlight issues around HIV prevention among young people.
UNAIDS sat down with Sibulele Sibaca, the founder of the campaign, to ask her a few questions.
Question: Describe Colour my HIV in five words
Vibrant. Youthful. Life-changing. Futuristic.
Hopeful in all that we do. We hope that by 2030 we will end AIDS. With Colour my HIV we’re hopeful that young people themselves will change the course of HIV.
Question: What do you want to achieve with Colour my HIV?
Firstly, I want get to a point in South Africa where being HIV-positive is like having any other chronic disease—diabetes, high blood pressure—in that it’s a manageable illness.
Secondly, to change the narrative where people think that when you contract HIV it is a death sentence. It’s no longer that at all. South Africa has one of the most well-implemented HIV treatment programmes in the world. I remember when a very close person in my life contracted HIV, the doctor said, “You should be so glad you got HIV in South Africa. This is the country to be in when you have HIV. In other countries people are still crying for HIV treatment and you have it here; all you have to do is adhere to it.”
Thirdly, the stigma around testing for HIV is that if I test positive I am going to die, so people must know that they will not die when they are HIV-positive. It’s one of the reasons I have called the campaign Colour my HIV. We must own it. We must celebrate how far we’ve come with HIV as a country. Let’s not discriminate or stigmatize, instead we must go out and get tested for HIV.
Question: Why the focus on young people?
Primarily, we were thinking of adolescent girls and young women between the ages of 15 and 24 years, because they are the most at risk of HIV infection in South Africa. In this age group, nine girls contract HIV every hour in South Africa. My question is, how and why? Where are they? What are the circumstances that lead to the moment they contract HIV? Are they hungry? This group can be influenced. The messages planted in their heads are critical, as they are still growing. So, Colour my HIV looks to be that voice of reason, to teach and educate them about why they should get tested, to prevent themselves from contracting HIV.
However, it is difficult to focus on girls in isolation. We can’t solely speak to girls, we have to engage boys as well. Men and boys hardly visit the clinic, test or take medication. They have to be included in the narrative, which is why Colour my HIV focuses on young people in general.
Question: Where do you see Colour my HIV in five years?
In the short term, we are looking to start touring South Africa from April until the next World AIDS Day, going into communities and really just spreading HIV awareness. As HIV is not only an issue on World AIDS Day, we are looking to engage communities on how they can embrace HIV and live in colour.
We actually need to end AIDS by 2030. We have 11 years to go. So, the question is what are we doing now? Hopefully this year we are going to take Colour my HIV countrywide. In the next three years, I want to see it journey from the Cape to Cairo. When they talk about ending AIDS by 2030, I want Colour my HIV to be part of the narrative.
Region/country

Feature Story
Young people to campaign against stigma and discrimination in Egypt
27 February 2019
27 February 2019 27 February 2019Ahead of Zero Discrimination Day, young people came together in Cairo, Egypt, to learn how to respond to HIV-related stigma and discrimination and to hear about how the HIV epidemic affects Egypt and the role that young people can play in the AIDS response.
“The burden of the epidemic is higher on young people. In Egypt, it is for young people to lead the HIV response,” said Walid Kamal, Egypt’s National AIDS Programme Manager.
During a discussion on stigma and discrimination, people living with HIV shared some of their testimonies and experiences, helping to give the participants a deeper understanding of how stigma and discrimination affects people living with HIV.
“It is our responsibility to help people living with HIV feel part of the community,” said one of the participating young people.
“It is not only about AIDS, it is about social justice, equality, the empowerment of women and promoting healthy gender norms,” said Ahmed Khamis, the UNAIDS Country Manager for Egypt.
The participants also learned how to plan, design and implement online awareness and advocacy campaigns on social media.
At the end of the meeting, organized by UNAIDS and the National AIDS Programme and held on 21 February, the young people agreed to lead social media campaigns to highlight the harm caused by stigma and discrimination. Starting on 1 March, Zero Discrimination Day, and running for three weeks, the campaigns will be supported by the UNAIDS country office in Egypt and are endorsed by Egypt’s Ministry of Health and Population.
Region/country
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025




Feature Story
How discriminatory Caribbean laws are being challenged in the courts
01 March 2019
01 March 2019 01 March 2019On the night of 6 February 2009 in Georgetown, Guyana, seven transgender women were rounded up by the police and detained for the weekend. The following Monday, in the Georgetown Magistrates Court, they learned that they had been charged with cross-dressing. They pleaded guilty, were convicted and were each ordered to pay a fine. But not before being admonished by the Magistrate that they were “confused about their sexuality.”
With support from the Faculty of Law University of the West Indies Rights Advocacy Project, U-RAP, the group challenged the nineteenth century Guyanese law that bars men from dressing like women, and women from dressing like men “for an improper purpose”. On 13 November 2018, Guyana’s final court of appeal, the Caribbean Court of Justice (CCJ), ruled unanimously that the law violates the Constitution of Guyana and is therefore void.
“No one should have his or her dignity trampled on, or human rights denied, merely on account of a difference,” CCJ President, Adrian Saunders, said.
For U-RAP Co-Coordinator and law lecturer Tracy Robinson, this was a step towards addressing the unequal power and unequal life chances of many Caribbean people.
"Laws do not apply evenly to everyone: those with the least resources and those marginalized are at greatest risk. Trans women are not the only ones who face lives which are cut short by state action and state inaction. There are many other instances in which we leave out and exclude those who are integral and part of our societies,” Ms Robinson said.
HIV is one manifestation of the way vulnerable communities are left behind. In the region, HIV prevalence among key populations is much higher than among adults generally. For example, among transgender women in Guyana—one of the few Caribbean countries with data on this population—the HIV prevalence is 8.4%, compared with 1.7% among all adults. Relevant Caribbean data indicate that HIV prevalence among gay men and other men who have sex with men ranges between 1.3% and 32.8%. The combination of discriminatory laws, stigma and discrimination and the relative lack of friendly services for members of key populations drives people underground, blocking them from HIV prevention and treatment services.
But in some countries, partners are acting to challenge the constitutionality of discriminatory laws held over from the colonial era. Through a case also supported by U-RAP, Caleb Orozco challenged the law in Belize that made “carnal intercourse against the order of nature,” which includes anal sex, a crime punishable by up to 10 years imprisonment. On 10 August 2016, Belize became just the second independent Commonwealth Caribbean country to decriminalize sex between men, and the first to do so through its courts.
And in Trinidad and Tobago the High Court ruled in favour of Jason Jones on 12 April 2018, finding that sexual activity between consenting adults should not be criminalized. This ruling was cited in the landmark Indian Supreme Court decision in 2018 decriminalizing gay sex.
UNAIDS is contributing to community engagement and communication around these issues, including supporting public forums in Belize and Trinidad and Tobago and the sensitization of journalists reporting on the transgender community in Guyana.
For the litigants, these victories are one step forward in a long journey towards equity.
“It forces communication between families and their lesbian, gay, bisexual and transgender relatives. It encourages people who are lesbian, gay, bisexual or transgender to come out the closet. It forces institutions to think about their administrative practices and the discrimination they justified based on that law. It forces homophobic people to acknowledge that the constitution covers everyone,” Mr Orozco said.
Litigant and co-founder of Guyana Trans United, Gulliver Quincy McEwan, said “It was very important for us to be heard and get justice.”