Update
Parental consent undermines the right to health of adolescents
16 March 2020
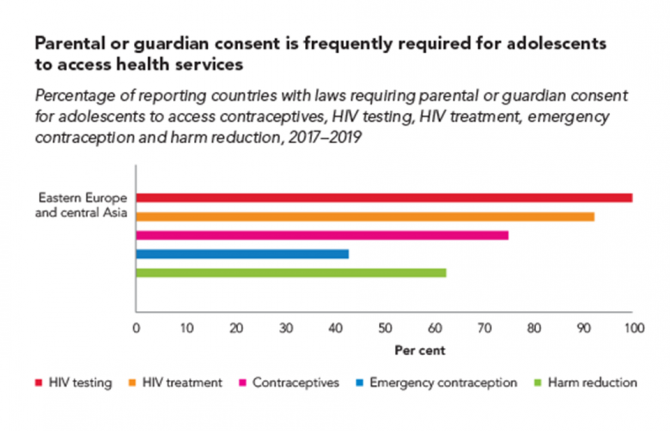
16 March 2020 16 March 2020Many countries have laws or policies that prevent adolescents from accessing essential health services without the consent of a parent or guardian. The original intention may have been to protect minors, but these stipulations often have the opposite effect and increase the risk of HIV and other health problems among adolescents.
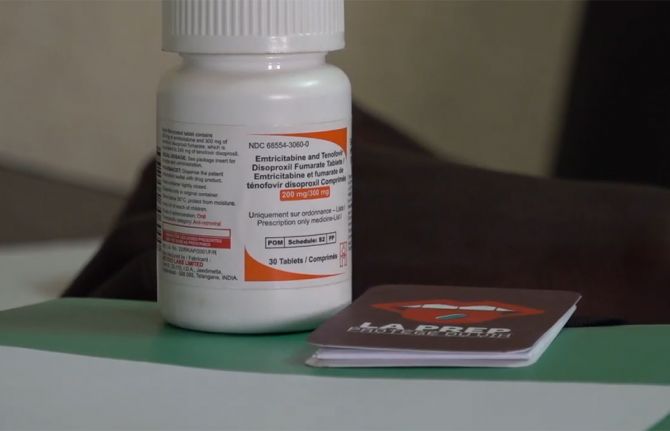
A large proportion of countries across all regions restrict access to HIV testing and treatment for adolescents. In 2019, for instance, adolescents younger than 18 years needed explicit parental consent in 105 of 142 countries in order to take an HIV test. In 86 of 138 reporting countries, they needed such consent to access HIV treatment and care. These kinds of laws and policies also may complicate or hinder adolescent access to pre-exposure prophylaxis (PrEP), a highly effective prevention tool.
Research in sub-Saharan Africa shows that in countries where the age of consent is 15 years or lower, adolescents are 74% more likely to have been tested for HIV in the past 12 months compared with countries where the age of consent is 16 years or higher—with girls especially benefiting from the easier access.
Country-level details on which countries have consent laws can be viewed on the UNAIDS Laws and Policies Analytics web page.
Resources





Feature Story
Turning the tide of the HIV epidemic in Thailand
17 January 2020
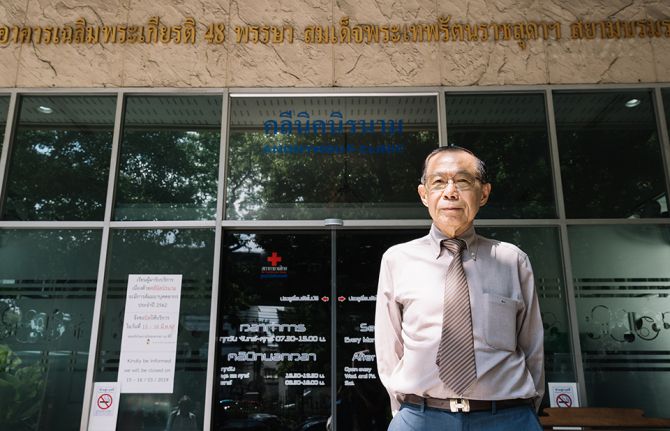
17 January 2020 17 January 2020It is a morning like any other at the Thai Red Cross AIDS Research Centre, a civil society organization operating under the umbrella of the Thai Red Cross Society. In a building in the heart of Bangkok, nurses, doctors, counsellors and peer educators are busy with their daily work, providing HIV services for the 200 people who attend the Thai Red Cross Anonymous Clinic every day for medical check-ups, HIV tests and HIV prevention services, including condoms and pre-exposure prophylaxis (PrEP).
When he was 35 years old, Praphan Phanuphak―the Director of the centre, which he co-founded in 1989―discovered the first case of HIV in Thailand. “It happened by accident. A patient was referred to me to investigate why he had a recurrent fungal skin infection,” he recalled. “In February 1985, this patient was admitted with pneumocystis pneumonia. During that month, another man was referred to the hospital with generalized cryptococcus infection. Both were diagnosed with HIV. Since then, I have devoted my life to treating people living with HIV and developing solutions to expand access to HIV services in the country.”
Mr Praphan remembers that in the early days of HIV the response in Thailand faced several challenges. At the time, Thai law required hospitals to report the names of people diagnosed with HIV to the Ministry of Public Health, which contributed to increasing stigma and discrimination against people living with HIV. In response, the Thai Red Cross established the Thai Red Cross Anonymous Clinic, Asia’s first anonymous clinic, and advocated with the Thai Government to remove the reporting law. The Anonymous Clinic remains the most renowned centre providing voluntary HIV testing in the country.
“Until the beginning of 2000, antiretroviral medicines were not available through public health facilities in Thailand, and many people living with HIV could not afford to buy them,” said Mr Praphan. He said that in 1996 the Thai Red Cross AIDS Research Centre was the first to provide free antiretroviral medicines as part of its clinical trials through the HIV Netherlands–Australia–Thailand Research Collaboration.
“After years of despair, a time of hope finally came. For that, I want to thank Her Royal Highness Princess Soamsawali, who stood by our side by setting up a fund for the prevention of mother-to-child transmission of HIV in 1996, several years before the Thai Government started its successful prevention programme,” said Mr Praphan.
The AIDS response in Thailand has changed dramatically over the years. In 2006, Thailand integrated its HIV services, including antiretroviral therapy, into its universal health coverage scheme. Since 2014 Thailand has provided antiretroviral therapy for all regardless of their CD4 level. Everyone can access treatment for free, and people living with HIV are offered treatment immediately after diagnosis.
However, many people are starting antiretroviral therapy late. “We have the medicines, but many people are not being diagnosed fast enough,” warned Mr Praphan. Despite tremendous progress, the HIV epidemic is not yet over in Thailand. HIV remains concentrated among key populations: almost 50% of new HIV infections in 2018 were among gay men and other men who have sex with men. Low uptake of HIV testing among key populations is related to the acceptability of services and stigma and discrimination, which hinder access to HIV diagnosis, prevention and care.
“From our experience, helping key populations to reach their peers and bring them to HIV drop-in centres, where they can be tested, is the best way to detect and diagnose people living with HIV early enough,” said Mr Praphan, who successfully advocated to amend Thai law to allow certified lay providers from key populations to provide a number of HIV services.
The Thai Red Cross AIDS Research Centre’s approach focuses on undertaking pilot projects to generate evidence to inform national planners and policymakers. That evidence provides a foundation for national acceptance and the roll-out of innovation on a national scale.
Taking the lead in reaching out to key populations, the centre has been offering PrEP to people at substantial risk of HIV since 2014 through projects such as the Princess PrEP Programme. In October 2019, Thailand introduced PrEP under its universal health coverage benefits package as a pilot phase in efforts to scale up PrEP nationwide.
Mr Praphan believes that policymakers and programme implementers should understand that, “We cannot continue to do business as usual. In Asia and the Pacific, several countries are still either sceptical or conservative in terms of promoting the necessary approaches to change the course of the HIV epidemic.” He thinks that the region cannot achieve the 90–90–90 targets by 2020 at the current pace. “We need to think out of the box and look at what other countries are doing that can be taken as a model. This is how we can move faster on our way towards ending AIDS as a public health threat.”
Region/country

Update
Barriers to PrEP must be removed
09 December 2019
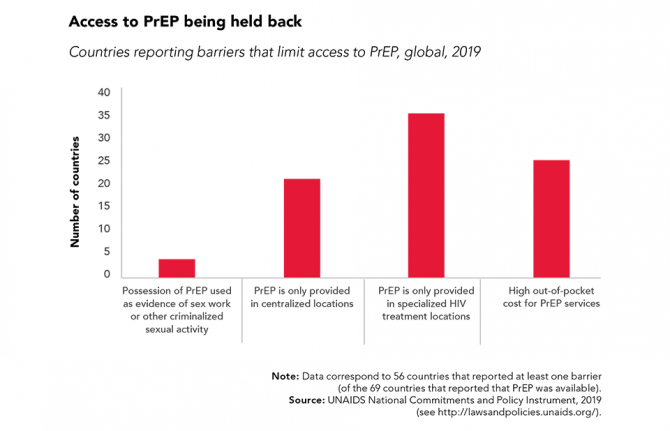
09 December 2019 09 December 2019Oral pre-exposure prophylaxis (PrEP) has shown considerable impact in reducing new HIV infections when provided as an additional HIV prevention choice to gay men and other men who have sex with men, transgender people and sex workers.
PrEP is now being rolled out in sub-Saharan Africa for serodiscordant couples and adolescent girls and young women who are at higher risk of HIV infection. Uptake is high when community-level stigma and misconceptions are addressed, when women and girls are provided with accurate and relevant messaging about PrEP and when PrEP is framed as an empowering prevention method and a positive life choice.
However, further global expansion of PrEP requires countries to address regulatory issues and other barriers that are stopping people who want to use PrEP from doing so.




Feature Story
iwantPrEPnow website founded out of necessity
28 November 2019
28 November 2019 28 November 2019When Greg Owen started hearing about a medicine taken daily that could keep people from contracting HIV, he didn’t believe it. The British man, from London, asked around and his friends told him that pre-exposure prophylaxis (PrEP) was only available in the United States of America or through a clinical trial, the PROUD study, in England.
“I finally managed to get a hold of some via a friend in early August 2015,” he recounted. “The next day, I went for an HIV test and it came back positive.” In shock, he felt like the system had failed him.
“It was too late for me, so out of necessity and anger we decided we had to do something,” Mr Owen said. His friend Alex Craddock was on PrEP. He needed to keep taking the medicine, which he obtained from the United States, so they both set out to help themselves and their friends.
They gathered as much information on PrEP as they could and on 19 October 2015 the website iwantPrEPnow went live.
With a small budget and limited time, but with a lot of publicity, iwantPrEPnow attracted more and more people. Traffic exploded.
“We had no master plan, but clearly there was a need for advice and access to the medicine within the community,” Mr Owen said.
Through a PrEP trial in England, more than 10 000 people have access to PrEP. In Wales, Scotland and Northern Ireland, PrEP is available through National Health Service (NHS) sexual health clinics. Countless others have obtained PrEP by buying it online.
Mr Owen, a club promoter turned full-time activism coordinator, credits 30 years of AIDS activism for improving HIV awareness and bringing new medicines to the forefront.
“PrEP has been a game-changer because it’s like the final piece of the jigsaw puzzle that has been missing,” he said. “We had already stepped up testing regularly, encouraged increased condom use and started people on treatment as soon as possible. All of these are part of our combination prevention response needed to fight the fire.”
Will Nutland, co-founder of Prepster, a group advocating for PrEP to be integrated within NHS England, considers the medicine as one of the most effective and cost-effective HIV prevention tools ever.
“No other HIV prevention technology has had the impact on HIV diagnosis in a place like London,” Mr Nutland said.
Half of new HIV infections in the United Kingdom have been shouldered by gay men and other men who have sex with men. In the past two years, new HIV infections among gay men and other men who have sex with men have decreased more than 30% across the country, according to HIV data by Public Health England. And in London, there has been a 44% drop.
Prepster and iwantPrEPnow launched within a week of each other. The founders didn’t know each other, so when they realized the crossover between them, they met and now collaborate on most projects.
For Mr Owen, PrEP has also changed the narrative. “We now have whole generations talking about sex in a guilt-free way,” he explained. He believes that people feel more liberated after decades of shame, death and disease linked to sex without condoms.
Among HIV advocates, the sector feels reinvigorated. Mr Owen feels proud being part of this supportive, loving and vibrant community. He says their common goal has brought lots of different players together.
“PrEP needs to be made available to all and not just at sexual health clinics,” he said, echoing Mr Nutland.
Their ongoing objective involves further increasing awareness of and access to PrEP for everyone who could benefit, particularly women, transgender people and communities of colour.
“A community means no one is left behind,” Mr Owen said. “No one gets turned out, that’s a real community.”
Video
Region/country
Related
Documents
Power to the people
04 December 2019
A new report by UNAIDS, Power to the people, released ahead of World AIDS Day, shows that where people and communities living with and affected by HIV are engaged in decision-making and HIV service delivery, new infections decline and more people living with HIV gain access to treatment. When people have the power to choose, to know, to thrive, to demand and to work together, lives are saved, injustices are prevented and dignity is restored.




Feature Story
Interview with UNAIDS PrEP expert Rosalind Coleman
16 September 2019
16 September 2019 16 September 2019Pre-exposure prophylaxis (PrEP) is delivered by a pill made of a combination of medicines. It has proved to be highly effective in preventing HIV-negative people from acquiring the virus. It is being rolled out or piloted in many countries across the world, including the United Kingdom. UNAIDS PrEP expert Rosalind Coleman explains.
How does the United Kingdom’s roll-out of PrEP compare with that of other high-income countries?
The United Kingdom’s PrEP programme is the largest in Europe, in terms of the number of people who have started PrEP. But the variety of ways that PrEP is made available in the country illustrates clearly that one PrEP strategy does not fit all countries. It also demonstrates how important advocates are and the key role of collaboration between all parties interested in PrEP.
In Scotland, PrEP is available free in sexual health clinics to residents of Scotland. The national-level purchasers have successfully negotiated an affordable price for them to buy PrEP.
In England, PrEP is not available routinely and advocates, progressive PrEP providers and others who support PrEP provision have had to be resourceful. Generic medicines have been purchased at competitive prices through the establishment of a large research trial that makes PrEP available in sexual health clinics. But the trial has not been able to provide PrEP to all the people who are asking for it, so online purchasing of PrEP from overseas is also a large source of PrEP. For people buying online, access to the clinical support, tests and follow-up that are part and parcel of a quality PrEP service should be provided and promoted.
Can you tell us a little more about the roll-out of PrEP in low- and middle-income countries?
The roll-out of PrEP in low- and middle-income countries is a mixed picture. Great progress has been made in providing PrEP in southern and eastern Africa and in some other regions, such as Thailand and now Viet Nam in Asia, and Brazil in Latin America. In other countries, particularly those with a growing HIV epidemic, PrEP access is extremely difficult. There is a combination of reasons for the low PrEP provision: the cost of the programme and overall low attention to primary HIV prevention certainly play a role, as does stigma and discrimination against providing appropriate services for many of the key populations that could benefit. Insufficient knowledge of PrEP and even misinformation among potential users and PrEP providers also prevent the promotion of PrEP.
Very clear and focused planning for PrEP scale-up, as part of a comprehensive HIV prevention programme, is an essential part of reducing new HIV infections
The use of PrEP is often associated with key populations, such as sex workers or gay men and other men who have sex with men, but can it be useful in other contexts?
For a PrEP programme to be effective, PrEP has to be taken by people with a real likelihood of contracting HIV and who want to take control of reducing that possibility―often members of key populations, but anyone in the situation of having a high prospect of HIV exposure should be able to discuss the use of PrEP and access it. This could include the HIV-negative member of a serodiscordant couple before the person living with HIV reaches viral suppression, or someone with a previous diagnosis of a sexually transmitted infection (STI) where there is a high rate of untreated HIV among their sexual partners.
Remaining on PrEP while in a period of potential high HIV exposure is vital and similarly depends on a personal conviction to take PrEP, good understanding of how to use and stop PrEP and ease of access.
How PrEP is messaged―this should be in a non-stigmatizing and empowering way from public advertising to health-care worker attitude―will make all the difference in effective PrEP uptake and continuation.
There has been some questioning of PrEP as contributing to the increase in STIs such as syphilis and gonorrhoea. Is there any evidence for this?
The link between PrEP use and increase in other STIs beyond HIV is a hot topic! The discussion should not become a reason to reduce PrEP access but instead should identify and encourage improved comprehensive sexual health services for prevention, identification and treatment of all STIs. A supportive and enabling discussion of STI risk and prevention should form part of PrEP provision.
The most recent systematic review confirmed that the STI rate was already high in people asking for PrEP, which is to be expected, and confirms that the people asking for PrEP are having condomless sex. Incidence of STIs is also high for people on PrEP. Whether this high incidence is due to changing sexual behaviour, or due to better detection of STIs because people are undergoing STI testing more regularly as part of a PrEP programme, is not yet resolved.
Either way, the take-home message is that the high rates of STIs that have been found among people using PrEP has identified an unmet need for STI prevention, diagnosis and treatment. In this way, the provision of PrEP is a door to the improvement of broader sexual health care and an opportunity to bring down the incidence of STIs. This is true across all populations using PrEP.
So, is PrEP a game-changer in the response to HIV?
There is currently a lot of attention, funds, brainpower and physical effort going towards PrEP in many settings, including research into future delivery methods (injections or the vaginal ring, for example) that could increase PrEP choice, uptake and continuation. If these efforts are linked to an improvement in all HIV service provision (primary prevention, testing and treatment) and their integration with other health services, such as sexual health and mental health care, then PrEP could have a greater impact beyond prevention of individual HIV infections. However, it is unwise to sit back and think that PrEP will change the game on its own.
PrEP basics by Rosalind Coleman
PrEP success in London
Region/country
Related
Documents
Meeting report, Shaping oral PrEP modelling for high-burden countries in sub-Saharan Africa, 6–8 June 2018
01 January 2019
The UNAIDS/ World Health Organization (WHO) meeting, Shaping oral PrEP modelling for high-burden countries in sub-Saharan Africa, was held in Geneva in June 2018. Meeting participants represented a broad range of oral pre-exposure prophylaxis (PrEP) stakeholders. They considered the model outputs required to advance PrEP programmes, the data and assumptions used in models, and decision-making around “reasonable use” of resources for PrEP. The principles covered in these discussions can apply to other biomedical HIV prevention tools.


Feature Story
Indonesia commits to piloting PrEP
15 July 2019
15 July 2019 15 July 2019Indonesia has decided to pilot pre-exposure prophylaxis (PrEP) in four cities with high levels of HIV prevalence. PrEP is a way for people who do not have HIV but who are at substantial risk of getting it to prevent HIV infection by taking a pill every day. It is hoped that the pilot project will pave the way for a wider roll-out across the country.
The commitment to piloting PrEP came during the 1st Indonesian Symposium on PrEP, which was organized by UNAIDS at the end of June. The two-day event brought together around 150 clinicians, public health officials and representatives of key populations, who shared their experiences of PrEP research and implementation strategies across the Asia-Pacific region. The pilot in Indonesia will be conducted in close collaboration with the Ministry of Health.
PrEP is a highly effective prevention choice for people who are at high risk of HIV infection such as sex workers, people who use drugs and gay men and other men who have sex with men. It is having a big impact in reducing new HIV infections in Australia and its availability is increasing in New Zealand, Thailand and Viet Nam. China, India, Malaysia and Philippines have also initiated pilot projects.
Prevention efforts are vital to strengthening the HIV response in Indonesia and PrEP would be a significant addition to the country’s combination prevention approach. Indonesia had 46000 new HIV infections in 2018 and has one of the fastest growing epidemics in the Asia Pacific region. In 2018 there were 640000 people living with HIV in the country and only 17% had access to treatment.
The discussions at the symposium helped to disperse some of the common misconceptions regarding PrEP, both among communities and services working to reduce new HIV infections. Civil society activists expressed their strong support for PrEP roll-out.
“PrEP will become a necessity for sex workers,” said Rito Hermawan of the Indonesian Sex Workers Network, “As well as using condoms, they can get additional protection by using PrEP. We must educate people about PrEP to stop any misconceptions.”
Other civil society activists echoed their support.
“The more I learn about the benefits of PrEP, the more I wonder why it is not available here,” said Mr. Riunaldi from Intermedika Prana Foundation, “I am hopeful that more people will understand how important PrEP is for our country.”
Participants in the symposium said that many people were already accessing PrEP online, indicating a growing demand in Indonesia.
“It is incumbent on policy makers, health professionals, researchers and civil society organizations to ensure that those at risk of HIV infection have access to the information and resources needed to make informed decisions regarding their health” said Tina Boonto, UNAIDS Country Director for Indonesia.
Region/country




Feature Story
Recognizing the achievements of the Thai Red Cross AIDS Research Centre
02 May 2019
02 May 2019 02 May 2019The Thai Red Cross AIDS Research Centre (TRC-ARC) has been at the forefront of the response to HIV since the early days of the epidemic, when its director, Praphan Phanuphak, diagnosed Thailand’s first case of HIV, in 1985. Since then, it has continued to develop and promote innovative prevention and treatment approaches, including pre-exposure prophylaxis (PrEP), same-day antiretroviral therapy and key population-led health services.
Located in Bangkok, Thailand, the TRC-ARC is an organization that sits under the umbrella of the Thai Red Cross Society. The Thai Red Cross has been a leading organization in the country’s response to HIV through projects implemented with partners and funded through the United States President’s Emergency Plan for AIDS Relief (PEPFAR).
Since the end of 2014, the TRC-ARC has been offering PrEP to people at higher risk of becoming infected with HIV through projects including the Princess PrEP programme, which is strongly supported by Her Royal Highness Princess Soamsawali. The Princess PrEP programme provides free PrEP services through community-led organizations such as the Service Workers in Group (SWING) Foundation, the Rainbow Sky Association of Thailand, Mplus, CAREMAT and SISTERS. The TRC-ARC also offers members of those community groups comprehensive training on health-care provision, sustainable financing, evaluation and quality control.
Since 2017, the TRC-ARC has also been offering same-day antiretroviral therapy to improve retention in care and adherence to treatment. People who test positive for HIV are initially prescribed a two-week supply of medicine and are then referred to other health facilities to continue their treatment.
Another significant achievement has been the creation of the Tangerine Clinic, the first in the country to offer health care and counselling tailored towards transgender people. The clinic is managed by transgender people and staffed by gender-sensitive medical professionals. It provides sexual and reproductive health-care services, psychosocial counselling, hormone counselling and therapy, HIV testing services and referrals for treatment.
During his recent visit to Thailand, the Executive Director of UNAIDS, Michel Sidibé, paid tribute to the work of Mr Praphan and the TRC-ARC at an event organized by UNAIDS and attended by representatives of the Thai Ministry of Public Health, the Thai Ministry of Foreign Affairs, PEPFAR, USAID, United Nations development partners and civil society organizations.
“The Thai Red Cross AIDS Research Centre has played a key role in developing and promoting innovative and effective prevention and treatment approaches to HIV for more than 30 years,” said Mr Sidibé, “Its contribution expands beyond Thailand, being a catalyst for change across the Asia–Pacific region,” he said.
Mr Praphan thanked UNAIDS for recognizing the achievements of the TRC-ARC and said its work would continue until the end of the AIDS epidemic. “I accept this recognition on behalf of all the people working with me at the Thai Red Cross and in the community to ensure that no one is left behind. We have demonstrated how science, integrated into the community level, can bring health care to the most marginalized groups of people.”
Region/country


Press Statement
UNAIDS welcomes additional evidence that effective antiretroviral therapy stops transmission of HIV
03 May 2019 03 May 2019Results from a large-scale European study among serodiscordant gay couples show that adherence to effective treatment prevents transmission of HIV
GENEVA, 3 May 2019—UNAIDS warmly welcomes the PARTNER2 study results that show that HIV transmission does not occur when a person living with HIV is on effective antiretroviral therapy. The study, which enrolled nearly 1000 gay couples in which one partner was living with HIV and the other was not, showed that where the person living with HIV was taking effective antiretroviral therapy and had a suppressed viral load, there was no HIV transmission within the couple.
“This is excellent news. People living with HIV now have confirmation that provided they take treatment regularly and are virally suppressed, they are not infectious,” said Michel Sidibé, Executive Director of UNAIDS. “This gives a strong, positive message that will help to reduce the stigma around HIV and improve the self-esteem and self-confidence of people living with HIV.”
By the end of the eight-year study, 15 people did become infected with HIV. Virus screening showed that none of the new infections were linked to the HIV-positive partners in the study, but came from a sexual partner outside of the couple. The researchers estimate that within the study, which took place across 14 European countries, around 472 HIV transmissions were averted over the eight years.
UNAIDS hopes that the results will encourage more people to get tested early and take effective treatment. In recent years there has been a huge scale-up in the roll-out and uptake of antiretroviral therapy. In 2017, of the 36.9 million people living with HIV, 59% (21.7 million) had access to treatment and 47% were virally suppressed. Concerted efforts are needed to ensure that all people living with HIV have access to and adhere to effective antiretroviral therapy.
A large proportion of HIV transmission still occurs before people know their HIV status. The risk of HIV transmission is highest in the weeks and months immediately after infection, when the viral load is high and the person who has contracted the virus is unlikely to know their status, is not on treatment and is not virally suppressed. This demonstrates the critical importance of continuing HIV prevention efforts, including condom use and pre-exposure prophylaxis—medicine taken by an HIV-negative person to prevent HIV.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
Sophie Barton-Knotttel. +41 22 791 1697 / +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)