40 years of the AIDS response




28 October 2021
28 October 2021 28 October 2021The Bangkok Metropolitan Administration (BMA) in Thailand has been awarded the inaugural Circle of Excellence Award at the Fast-Track cities 2021 conference, held recently in Lisbon, Portugal. The Circle of Excellence Award showcases outstanding work in fast-tracking the HIV response and advancing innovative programming to end the AIDS epidemic in cities by 2030.
“To receive the Circle of Excellence Award for Bangkok is a great honour. It demonstrates not only the past achievements but, moreover, the future commitment to accelerate the HIV response and towards ending AIDS in Bangkok. We are proud that innovations have produced remarkable results, particularly same-day antiretroviral therapy and key population-led health services, such as specialized and holistic services for transgender people and the scale-up of pre-exposure prophylaxis (PrEP) programmes. These innovations are not only applied in Bangkok but have become models for the region,” said Parnrudee Manomaipiboon, the Director-General of the Department of Health, BMA, during the award ceremony.
Organized by the International Association of Providers of AIDS Care, in collaboration with UNAIDS, the Fast-Track Cities Institute and other partners, the Fast-Track cities conference highlighted successes achieved across the Fast-Track cities network, addressed cross-cutting challenges faced by local stakeholders and shared best practices in accelerating urban HIV, tuberculosis and hepatitis B and C responses.
“Bangkok has put in place a 14-year strategic plan for ending AIDS from 2017 to 2030, which is under the leadership of the Bangkok Fast-Track Committee,” said Pavinee Rungthonkij, the Deputy Director-General, Health Department, BMA. “During COVID-19, BMA and partners have introduced innovations such as multimonth antiretroviral therapy, an express delivery of antiretroviral therapy service, sexually transmitted infection self-sampling and PrEP,” she added. Among other achievements, Bangkok has expanded its PrEP services to 16 municipal public health centres and eight city hospitals and implemented citywide awareness campaigns. PrEP in the City was the first citywide PrEP campaign focusing on transgender people in Asia.
“Significant progress has been made in the HIV response since Bangkok joined the Paris Declaration to end the AIDS epidemic in cities in 2014. It shows that mutual commitments and a strengthened partnership between stakeholders at all levels are key to an effective HIV response. Bangkok will continue to leverage support, scale up innovations and Fast-Track solutions to achieve the 2025 targets and end AIDS by 2030,” said Patchara Benjarattanaporn, the UNAIDS Country Director for Thailand.


05 July 2021
05 July 2021 05 July 2021ACON, one of Australia’s largest HIV organizations, working to promote HIV prevention strategies among gay men and other men who have sex with men in New South Wales, Australia, has recently launched a new campaign video that enlists some of Asia’s most popular social media influencers.
The campaign aims to raise awareness and promote the uptake of pre-exposure prophylaxis (PrEP), particularly among Mandarin-speaking gay men and other men who have sex with men. The campaign addresses frequently asked questions about PrEP and features Fufu and Josh, also known on social media as FJ234, YouTube personalities with a following of 350 000 subscribers. The pair appear alongside a leading doctor and PrEP advocate, Stephane Wen-Wei Ku, who in the campaign breaks down information on PrEP through relatable and humorous conversations.
“PrEP is a good tool to protect yourself, even if you are not ready to talk about sex with your partner. So, we could all have a great sex life without worrying about HIV,” Josh and Fufu explained.
In Asia and the Pacific, civil society organizations in countries such as Thailand and the Philippines have turned to social media platforms and other innovative solutions to offer new ways to link communities to PrEP and other prevention options. For example, in Thailand, the PrEP in the City campaign, launched by the Institute of HIV Research and Innovation and supported by the UNAIDS Regional Support Team for Asia and the Pacific and other key partners, aimed to increase PrEP uptake among transgender women by challenging negative perceptions. Likewise, in the Philippines, civil society organizations used innovative programmes to deliver antiretroviral therapy to clients, and PrEP and condoms were frontloaded to community champions for distribution.
“Raising awareness of PrEP, which is an extremely effective strategy for preventing HIV transmission, is fundamental to our efforts in eliminating the virus,” said Nicolas Parkhill, the Chief Executive Officer of ACON, reflecting on the critical role of the campaign in scaling up PrEP among Mandarin-speaking gay communities in New South Wales.
PrEP has had an enormous impact on HIV transmission rates in New South Wales and Australia as a whole since it was first made available in 2016 through various state-based trials, and later in 2018 when it was subsidized under the national Pharmaceutical Benefits Scheme. Currently, there are three main ways to access PrEP in Australia. The most common is through the Australian health-care system at a subsidized cost. Other options include purchasing PrEP from a pharmacy using a private prescription from a doctor or purchasing it from a reputable pharmacy and importing it into Australia under the Personal Importation Scheme. These last two options are particularly important for people who are not covered under the Australian health-care system, such as international students.
“PrEP is now the most commonly used HIV prevention strategy for gay men, but if we are to realize its full potential on reducing HIV transmission in New South Wales, we need to break down barriers and ensure that PrEP is easily accessible to all men in every community. By working with Fufu, Josh, Stephane Wen-Wei Ku and Hotline, we hope the video will be able to help raise awareness and show how effective it is, how easy it is to get and its benefits,” Mr Parkhill added.
The campaign video was developed in partnership between ACON and the Taiwan Tongzhi Hotline Association, a sexual health organization. A vital feature of the campaign was that the content was developed with the Mandarin-speaking community, so that the messaging is authentic to Mandarin-speaking men. The video is available in Traditional and Simplified Mandarin, with English subtitles.
“To close the gaps and ensure that no one is left behind, we must foster innovation and scale up access to HIV prevention and treatment services. Strong national commitment to scale up PrEP, adopting national PrEP policies and guidelines, setting ambitious PrEP targets and allocating sufficient resources for PrEP will help countries across the region to get the HIV response back on track. We have the tools to end AIDS. Now we must use them,” said Eamonn Murphy, Director, UNAIDS Regional Support Team for Asia and the Pacific.


19 January 2021
19 January 2021 19 January 2021This year, Guyana will roll out a comprehensive plan for pre-exposure prophylaxis (PrEP). The Guyana Minister of Health, Frank Anthony, announced that the national strategy will be implemented in collaboration with clinics across the country and nongovernmental organizations.
“We want to expand to ensure anyone who is at risk for HIV would have access,” Mr Anthony said. “We believe that with a comprehensive programme for PrEP we can prevent many infections.”
This move marks the culmination of years of advocacy and partial PrEP implementation. The existing PrEP policy is a programme for serodiscordant partners only, so couples in which just one person is living with HIV have been able to access PrEP through the public health-care system to avoid transmission to the HIV-negative partner.
Since 2015, the World Health Organization has recommended that “people at substantial risk of HIV infection” should be offered PrEP. Several countries have prioritized key populations, including gay men and other men who have sex with men, sex workers and transgender people, for PrEP programming. In Guyana, those groups also have higher HIV prevalence: 8% for transgender women, 6% for sex workers and 5% for gay men and other men who have sex with men.
Last year, Guyana’s Society against Sexual Orientation Discrimination (SASOD Guyana) moved from calling for a more inclusive PrEP programme to offering the service itself. The group teamed with the Midway Specialty Care Centre to fill this gap in the country’s HIV prevention response.
“We want combination prevention to take the front burner,” said Joel Simpson, the SASOD Guyana Managing Director. Through this private sector/civil society partnership, for the first time people in Guyana from any population group were able to elect to initiate PrEP. The medicine was sold to clients at cost price and those accessing the service through the nongovernmental organizations paid no consultation fees.
A 2018 SASOD Guyana assessment of gay men and other men who have sex with men and transgender people supported by the International HIV and AIDS Alliance (now called Frontline AIDS) found that, when sensitized, there was a high level of interest in taking PrEP. However, just around 60% of focus group participants were willing to pay to do so.
“We need politicians and technical people to base decisions on science and research. At times we have encountered a moralistic approach to setting public policy,” Mr Simpson reflected. “It’s not about whether you belong to a particular population group. It’s about responding to reality and lowering risk.”
Guyana’s HIV programme results are among the Caribbean’s best. The country surpassed the 2020 testing target, with 94% of people living with HIV diagnosed in 2019. Seventy-three per cent of people who knew their status were on treatment. Of those, 87% were virally suppressed. Over the past 20 years, new HIV infections have been reduced by half in the South American nation.
“HIV treatment has come a long way, and not just for people living with HIV. To close the gaps and ensure that no one is left behind it is critical that best practices for prevention and treatment are implemented fully,” said Michel de Groulard, UNAIDS Country Director, a.i., for Guyana and Suriname. “This is why we are pleased about the direction the Health Ministry is taking this year to ensure that PrEP is made available to all who need it. We have the tools to end AIDS. Now we must use them.”


09 December 2020
09 December 2020 09 December 2020Rena Janamnuaysook steps off the Skytrain in Bangkok’s bustling Sukhumvit shopping district. She looks up, filled with a sense of joy as her eye catches an advert just beyond the platform. The advert is promoting the PrEP in the City campaign to raise awareness and increase the uptake of PrEP among Thai transgender women and shows glimpses of the lives of four transgender women as they juggle their busy work schedules, their role as a mother and their relationship with loved ones, all the while taking control of their health with their daily dose of pre-exposure prophylaxis (PrEP). For Ms Janamnuaysook, a transgender advocate and Program Manager for Transgender Health at the Institute of HIV Research and Innovation (IHRI), this first-ever PrEP campaign for transgender women in Thailand signals promise for the country’s HIV response.
“PrEP campaigns of the past were only targeting other key populations, especially men who have sex with men and gay men. Transgender women were left out from PrEP campaigns or public messages,” says Ms Janamnuaysook.
HIV prevalence among transgender people in Thailand was estimated to be 11% in 2018, with no sign of a decline in the past few years, and the current uptake of PrEP among transgender women is only 7%, making the group a particularly at-risk population. Less than half (42%) of transgender people reported that they are aware of their HIV status, while services catering to their specific needs are limited.
Limited awareness and knowledge about PrEP contribute to the low uptake. The campaign strategy includes reframing the conversation on PrEP use and challenging negative perceptions of PrEP within the transgender population. “For transgender women who know about PrEP already, they still don't want to get it because it has been associated with risky behaviour or negative behaviour. In Thai society, if you use PrEP then you are perceived to have multiple partners, be a sex worker or must have unprotected sex,” says Ms Janamnuaysook.
Ms Note, a client at the Tangerine Clinic, South East Asia’s first transgender-specific sexual health clinic that offers gender-affirming integrated health care and PrEP, among many other health services, speaks of the perception of PrEP, saying, “I had to be cautious so that nobody sees me taking the pills because sometimes people are worried and think that I am sick.” A goal of the campaign is to normalize the use of PrEP and promote continued use, particularly important when evidence suggests that nearly half of transgender women (46%) in Thailand did not return for their one-month visit after starting PrEP.
“The campaign makes taking PrEP seem similar to taking vitamins or supplements for good health. It removes the image that PrEP is suitable for only certain groups, when in fact it can be taken by anybody,” said Ms Note.
Adverts for the campaign are on billboards across Bangkok, illustrative of the collaboration with the Bangkok Metropolitan Administration and the commitment to achieve the city’s Fast-Track Targets. Online, IHRI has enlisted various social media influencers, bloggers and opinion leaders in the transgender community to share information about the campaign.
“I personally feel proud to have participated in this campaign, which makes people see the other sides of us, transgender women, and our potentials,” says Jiratchaya (Mo) Sirimongkolnavin, a model and beauty blogger featured in the campaign, who is a former winner of Miss International Queen, one of the world’s largest transgender beauty pageants. She goes on to explain, “It encourages people to have general conversations about sex and how to protect themselves from HIV infection.”
Promoting positive representations of Thai transgender women is an underlying focus of the campaign. “I think the story in the video will help wider audiences to see the diversity among transgender people that actually exists in today’s society,” said Ms Note. “The fact that transgenders have many occupations and abilities.”
At a launch event for the campaign, Satit Pitutecha, Deputy Minister of Public Health, spoke about the government’s commitment to strengthening the HIV response, stating, “The Ministry of Public Health has committed to working in partnership with communities and civil society to promote access to HIV and other health services for transgender people.”
Ms Janamnuaysook is proud of the buzz that the campaign has catalysed, which has been shared widely in Thailand and in surrounding countries. She hopes that this campaign, with its tailored messaging for transgender women, won’t be the last and believes that it can serve as a model for future campaigns focusing on other key populations.
The PrEP in the City campaign was developed by IHRI and is supported by the United States President’s Emergency Plan for AIDS Relief through the United States Agency for International Development’s LINKAGES Thailand Project, managed by FHI 360 and the United States Centers for Disease Control and Prevention, the Bangkok Metropolitan Administration, the Division of AIDS and STIs of the Ministry of Public Health and the UNAIDS Asia–Pacific Office.

02 November 2020
02 November 2020 02 November 2020Pre-exposure prophylaxis (PrEP), an HIV prevention option whereby someone who is HIV-negative takes antiretroviral medicines prior to possible exposure to HIV, has been shown to be highly efficacious across all populations. The offer of PrEP as part of a combination approach to HIV prevention has been recommended by the World Health Organization for all people at substantial risk of HIV since 2015.
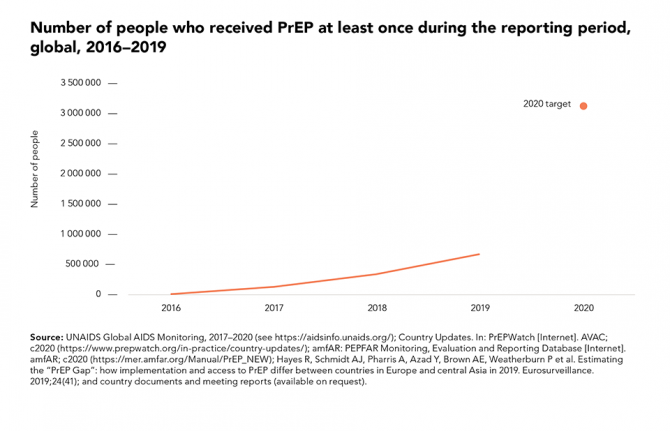
The number of people reported to have received PrEP at least once in the previous year has increased dramatically in recent years, from fewer than 2000 in 2016 to more than 590 000 in 2019. In several cities in North America, Europe and Australia where PrEP is widely available, this relatively new prevention tool has contributed to steep reductions in HIV infections among gay men and other men who have sex with men. Global coverage, however, is still far short of the 2020 target of 3 million people receiving PrEP.


07 October 2020
07 October 2020 07 October 2020The Ashodaya pre-exposure prophylaxis (PrEP) demonstration project for female sex workers in south India has shown how PrEP and HIV prevention programmes can be strengthened and their implementation accelerated beyond pilot projects.
While PrEP has been shown to be highly efficacious, with nearly 100% protection if it is taken as directed, delivering a successful PrEP programme is challenging. HIV prevention efforts among sex workers have traditionally focused on condom use, and while a range of successful programmes have contributed towards the decline in new HIV infections in the Asia–Pacific region, sex workers still experience a disproportionate burden of infection. In 2019, 9% of the estimated 300 000 new HIV infections in the Asia–Pacific region were among sex workers and globally the relative risk of HIV infection is 30 times higher among sex workers than among the general population.
PrEP is a relatively recent addition to the range of HV prevention options available. It involves someone who is HIV-negative taking antiretroviral medicines prior to possible exposure to HIV. Although recommended by the World Health Organization (WHO) for all people at substantial risk of HIV since 2015, PrEP is inaccessible to the majority of key populations, including sex workers, and their partners in the Asia and the Pacific region. There is limited evidence on PrEP use among women, and particularly among female sex workers, in Asia and the Pacific.
The Ashodaya PrEP demonstration project was one of two community-led and community-owned initiatives to provide PrEP to female sex workers supported by the Bill & Melinda Gates Foundation (the other was led by the Durbar Mahila Samanwaya Committee Kolkata). Sex workers in India had been concerned by the fact that, although condom use was high, some sex workers still acquired HIV.
“Our project shows that community-led PrEP delivery can be effectively integrated into the existing HIV prevention and care services for sex workers and result in high retention and adherence. Policymakers need to consult with us, listen to us and trust us as we know what works for us and how to make it work. We have an obligation to make PrEP available as an additional prevention tool in a safe and sustainable way and we are advocating for that,” said Bhagya Lakshmi, Secretary of Ashodaya Samithi.
The PrEP demonstration project, which began in April 2016 and ended in January 2018, reported good results. High levels of continuation on PrEP were reported, with 99% of the 647 participants completing the 16 months of follow-up. For women, it is critical to take PrEP daily to maintain protection. Although adherence was only 70% at month three, this increased to 90% at month six and was 98% in the final month of the project. Self-reported adherence was verified in the blood of a subset of participants at months three and six.
The project not only helped to dispel some common fears about PrEP but showed benefits in bridging the prevention gap. Rather than undermining condom use, it remained stable. Condom use was high for occasional clients, at approximately 98%, but lower for repeat clients (87–96%) and regular partners (63%). There were also no increases in symptomatic sexually transmitted infections and no cases of HIV acquisition during the follow-up period.
Several factors contributed to the success of the Ashodaya PrEP project, including:
“We cannot stop new HIV infections in Asia and the Pacific if we stick to business as usual,” said Eamonn Murphy, Director, UNAIDS Regional Support Team for Asia and the Pacific. “PrEP answers an unmet need and expands the prevention options for people at substantial risk of HIV. We need to scale up PrEP as an additional effective HIV prevention intervention. The principles of the Ashodaya PrEP demonstration project is a model not only for India but for the entire region. The lessons learned from the project are critical to informing the way forward in the prevention agenda.”
From conceptualization to planning, implementation and monitoring, the Ashodaya PrEP project was a community-led process. In 2018, the pilot project ended and analysis of the results was completed with support from UNAIDS India and WHO. Since then, Ashodaya has trained a cadre of community members as advocates for PrEP in partnership with the All India Network of Sex Workers and with support from AVAC. Ashodaya, with support from UNAIDS, WHO, the Durbar Mahila Samanwaya Committee and the All India Network of Sex Workers, is also continuing to advocate for PrEP with the Indian National AIDS Control Organization (NACO). Ashodaya is also exploring opportunities for community social franchising and marketing of PrEP to further support access. NACO has developed a draft national PrEP policy and guidelines. The community is eagerly waiting for the resumption of PrEP services.


30 June 2020
30 June 2020 30 June 2020Mihai Ceban (not his real name) has been locked down at home since 17 March, when a state of emergency was declared in the Republic of Moldova in response to COVID-19. He is an information technology specialist, so working from home has not disrupted his daily routine too much. His was worried, however, by his inability to go out to get his supply of HIV pre-exposure prophylaxis (PrEP). He has been taking PrEP to prevent becoming infected with HIV since September 2019. Although he has a partner, he says taking PrEP makes him feel safer. “You can’t fully trust your partner,” he said.
During the state of emergency, restrictions imposed by the authorities and the fear of becoming infected with COVID-19 limited his social contacts to a maximum of two or three people. However, his partner continued to lead an active social life, which increased his risk of HIV infection.
"The fear of COVID-19 was enhanced by the fear of getting infected with HIV. That's why, when I saw I was running out of my pills, I started worrying. I wondered what I would do if no one was working? How do I protect myself? The response came from the GENDERDOC-M Information Center, which delivered my PrEP at home. And the fact that it was delivered to me during the pandemic means that my right to health was respected. It’s my right to have an active protected sex life during the pandemic. And the delivery of PrEP services at home has brought psychological relief and reduced the anxiety of becoming infected with HIV,” Mr Ceban said.
Mr Ceban is not the only beneficiary of the PrEP deliveries. Alexandru Goja, a health programme consultant at the GENDERDOC-M Information Center, said that during the pandemic more than 90 people received PrEP deliveries at home.
“At the beginning of the pandemic, everyone went into a kind of panic. Some people on PrEP discontinued taking it, but most wanted to continue. For them, we went out, into the parks, in front of their apartments blocks, where we tested them for HIV and delivered their medicine. During quarantine, people from key populations avoided going to medical institutions to pick up their medicines, trying to prevent the risk of becoming infected with COVID-19. The support provided by nongovernmental organizations helps them to exercise their right to health,” said Mr Goja.
Angela Nagît, an infectious disease specialist at the Hospital of Dermatology and Communicable Diseases, agrees with him. During the pandemic, she carried out consultations and prescribed PrEP remotely. It is very important that once enrolled on PrEP, the person should stick to it, she said.
“In the Republic of Moldova, HIV infection continues to be a major public health problem with a great medical, social and economic impact. Around half of the people who are estimated to be living with HIV don’t know their status. Unprotected sexual contact is one of the risk factors for HIV transmission. PrEP is a way to prevent infection, thus ensuring the right to health, especially for those from the key affected groups,” she said.


Ground-breaking new study shows the efficacy of a long-acting injectable to prevent HIV
GENEVA, 19 May 2020—UNAIDS warmly welcomes the announcement that the long-acting injectable cabotegravir is safe and effective in preventing HIV among gay men and other men who have sex with men and transgender women. The HIV Prevention Trials Network (HPTN) 083 study enrolled almost 4600 HIV-negative people from across more than 40 sites in North and South America, Asia and Africa.
“This is a breakthrough that will have a significant impact on the lives of gay men and other men who have sex with men and transgender women when they are at higher risk of HIV infection.” said Shannon Hader, UNAIDS Deputy Executive Director, Programme. “We are particularly pleased that the study met its targets to recruit substantial numbers of younger black men who have sex with men and transgender women, the very people for whom accessing effective HIV prevention still remains a huge challenge.”
In 2018, UNAIDS estimates that there were 1.7 million new HIV infections, 54% of which were among key populations and their partners, including gay men and other men who have sex with men, transgender women, sex workers, people who inject drugs, people in prison, clients of sex workers and sex partners of other key populations.
Pre-exposure prophylaxis (PrEP)—HIV-negative people using antiretroviral medicine to prevent HIV infection—is an important element in the HIV combination prevention toolkit. PrEP allows people to reduce their risk of becoming infected with HIV, particularly during periods of increased risk in their lives. It may also provide reassurance and reduce anxieties when the risks are uncertain.
Once it has passed regulatory approval, and when production of affordable cabotegravir can be scaled up, gay men and other men who have sex with men will have the choice of three highly effective ways to use PrEP to prevent HIV infection: daily pills, pills taken before and after sexual activity (event-driven PrEP) or an injection every two months. Transgender women will be able to choose between injections or daily pills, since the World Health Organization does not recommend event-driven PrEP because of possible drug interactions with some hormones. Injections of cabotegravir every two months are an important option for people who find it hard to take a pill every day, yet remain vulnerable to HIV infection.
The trial was scheduled to continue for at least another year, but the first interim analysis of the data was brought forward a few weeks because of the potential disruption that the COVID-19 pandemic might cause to high-quality clinical trial procedures. The Data and Safety Monitoring Board (DSMB) in the United States of America reviewed the data up to March 2020 and found that there was already clear evidence that cabotegravir was highly effective and not inferior to the currently recommended oral PrEP regimen.
Half of the study group were given oral PrEP and were injected with a placebo; the other half were given a cabotegravir injection and took a placebo pill. The study found a total of 12 HIV infections in the group using the injectable compared to 38 in the group taking the daily pill. The side-effects of both treatments were relatively mild, with only 2.2% of people in the injection group choosing to stop having the injections because of painful reactions. The DSMB therefore recommended that the study be halted and that all participants be notified of the result. The participants will be able to choose which regimen they wish to continue on.
Despite good adherence in the oral group and very few discontinuations in the injection group, the overall incidence of HIV infection in the study was 0.79 per 100 person-years. Planned analyses will explore why those 50 infections occurred among the 4565 trial participants.
An additional study (HPTN 084) is ongoing to establish the efficacy of the long-lasting injectable in non-transgender women. To date, more than 3000 sexually active women in seven African countries have enrolled in the study. Those results are expected in November.
“We are eagerly awaiting the results of the ongoing HPTN 084 study among African women,” said Dr Hader. “We hope that by the end of this year there will be equally good news for women around the world.”
HTPN 083 was conducted by the HPTN and funded by ViiV Healthcare and the United States National Institute of Allergy and Infectious Diseases. Cabotegravir has not yet been approved for the treatment or prevention of HIV as a single agent by regulatory authorities anywhere in the world. ViiV Healthcare plans to use the data from HPTN 083 for future regulatory submissions.
UNAIDS congratulates the research teams and urges continued investment in research and development for HIV vaccines, diagnostics, preventative medicines, treatment and a cure.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Download the printable version (PDF)


GENEVA, 17 March 2020—UNAIDS warmly welcomes the decision made to make pre-exposure prophylaxis (PrEP) available to everyone who needs it in England. Activists and advocates have been campaigning for a number of years to make the life-saving preventative HIV medicine available to people at higher risk of HIV and on 15 March the government announced that PrEP will be made available across the country as part of the government’s efforts to end HIV transmission by 2030.
“This is absolutely the right thing to do,” said Winnie Byanyima, Executive Director of UNAIDS. “PrEP has been evaluated across different age groups among gay men and other men who have sex with men, transgender women, heterosexual men and women and people who inject drugs. In each of these contexts, the data are clear: PrEP prevents HIV and must be made available to all who need it.”
From 2017, PrEP was available in England as part of the Impact trial, which enrolled around 20 000 participants. The government has committed £16 million from 2020 to 2021 for the roll-out of PrEP through the National Health Service, starting in April 2020.
The availability of PrEP through the Impact trial is believed to have contributed to the fall in new HIV infections among gay men and other men who have sex with men across England. New infections among gay men and other men who have sex with men are estimated to have fallen by 71% from their peak in 2012. Efforts are being put in place to improve the availability of PrEP, as part of a comprehensive sexual health service, to other groups that could benefit.
The United Kingdom of Great Britain and Northern Ireland has accelerated its response to HIV and has already achieved the 90–90–90 targets. Of the estimated 103 800 people living with HIV in the United Kingdom in 2018, 93% had been diagnosed with the virus, of whom 97% were accessing treatment, and, of the people on treatment, 97% had undetectable viral loads, meaning they cannot transmit the virus.
UNAIDS commends the United Kingdom’s decision and will continue to support all efforts across the country to end AIDS by 2030.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Download the printable version (PDF)