Tuberculosis TB
Публикации
Documents
UNAIDS Executive Director meets with Brazilian Government and civil society
UNAIDS Executive Director Mr Michel Sidibé held a series of meetings with Government officials and civil society groups in Rio de Janeiro and Brasilia during his official visit to Brazil.
Related
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 июля 2024 года.
UNAIDS Terminology Guidelines
01 июля 2024 года.
 Ahead of World AIDS Day UNAIDS is calling for urgent support to Let Communities Lead in the fight to end AIDS
Ahead of World AIDS Day UNAIDS is calling for urgent support to Let Communities Lead in the fight to end AIDS
30 ноября 2023 года.
Summary — Let Communities Lead — UNAIDS World AIDS Day report 2023
28 ноября 2023 года.
 Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics
Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics

06 июня 2023 года.
 In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence
In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence

03 апреля 2023 года.
 UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
24 мартаа 2023 года.
 LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians
LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians

27 февраля 2023 года.
 One year on: We must sustain the HIV response in Ukraine
One year on: We must sustain the HIV response in Ukraine

23 февраля 2023 года.
Documents
UNAIDS Executive Director, Michel Sidbé visits Brazil
UNAIDS Executive Director Mr Michel Sidibé visited the Rio de Janeiro based Viva Cazuza Society on 26 March, a non-profit organization that provides a home for 20 children and adolescents, aged 2 to 16, who are living with HIV.
Related
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 июля 2024 года.
UNAIDS Terminology Guidelines
01 июля 2024 года.
 Ahead of World AIDS Day UNAIDS is calling for urgent support to Let Communities Lead in the fight to end AIDS
Ahead of World AIDS Day UNAIDS is calling for urgent support to Let Communities Lead in the fight to end AIDS
30 ноября 2023 года.
Summary — Let Communities Lead — UNAIDS World AIDS Day report 2023
28 ноября 2023 года.
 Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics
Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics

06 июня 2023 года.
 In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence
In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence

03 апреля 2023 года.
 UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
24 мартаа 2023 года.
 LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians
LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians

27 февраля 2023 года.
 One year on: We must sustain the HIV response in Ukraine
One year on: We must sustain the HIV response in Ukraine

23 февраля 2023 года.
Documents
UNAIDS Executive Director Michel Sidibé attends 3rd Stop TB Partners Forum, Rio de Janeiro
The Executive Director of UNAIDS, Mr Michel Sidibé is in Brazil this week to attend the 3rd TB Partners Forum. Earlier today in Rio de Janeiro, Mr Sidibé also joined the international launch of the World Health Organization’s annual report on global TB control.
Related
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 июля 2024 года.
 Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics
Brazil hosts the announcement of the Global Council on Inequality, AIDS and Pandemics

06 июня 2023 года.
 In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence
In Northeast Brazil, civil society and local government collaborate to increase HIV treatment adherence

03 апреля 2023 года.
 UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
24 мартаа 2023 года.
 The First Fallen but We Will Overcome
The First Fallen but We Will Overcome

03 ноября 2022 года.
 UNAIDS welcomes Chile’s public apology in landmark case of involuntary sterilization of women living with HIV
UNAIDS welcomes Chile’s public apology in landmark case of involuntary sterilization of women living with HIV

27 мая 2022 года.
 Encouraging income generation and social entrepreneurship by people living with HIV in Brazil
Encouraging income generation and social entrepreneurship by people living with HIV in Brazil

29 мартаа 2022 года.
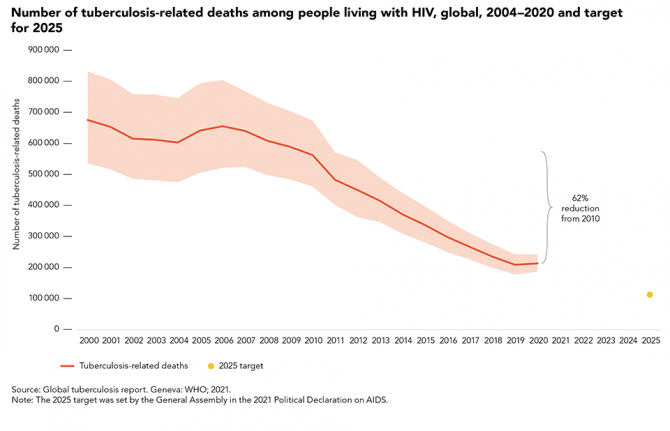
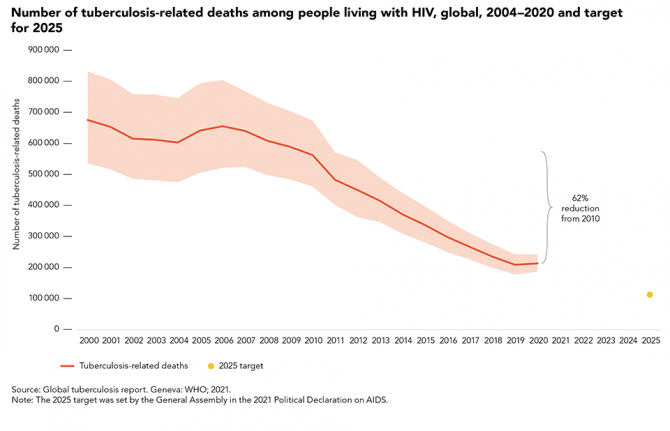
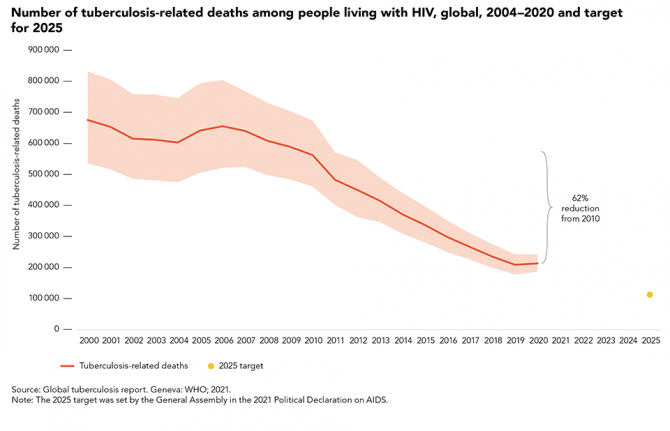
 Impact of COVID-19 hits hard as TB deaths among people living with HIV rise for the first time since 2006
Impact of COVID-19 hits hard as TB deaths among people living with HIV rise for the first time since 2006
23 мартаа 2022 года.
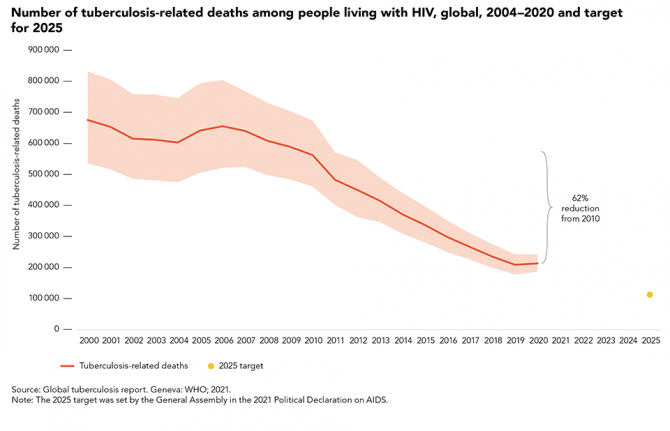 TB disease and deaths declining among people living with HIV, but there have been some reversals due to the COVID-19 pandemic
TB disease and deaths declining among people living with HIV, but there have been some reversals due to the COVID-19 pandemic
23 мартаа 2022 года.
40 years of the AIDS response
08 июня 2021 года.
Documents
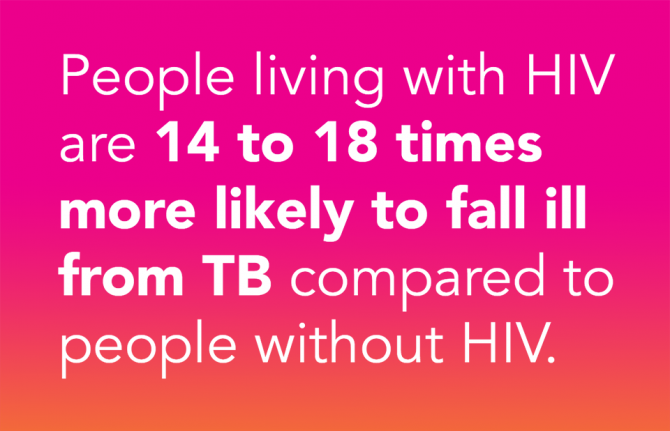
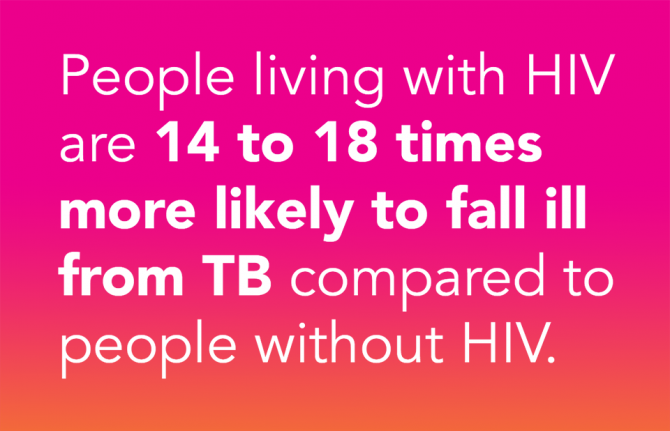
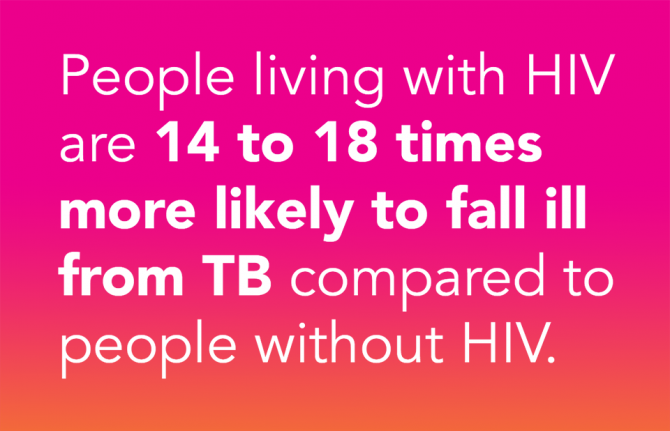
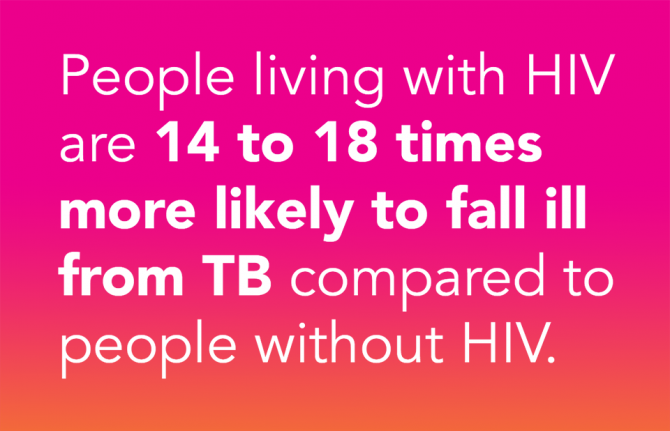
Tuberculosis and HIV: the dual epidemic
Up to half of all deaths in people living with HIV are caused by tuberculosis - Yet TB is both preventable and curable.
Related
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 июля 2024 года.
 UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
UNAIDS Executive Director Message on World TB Day – Yes, we shall and we can end TB among people living with HIV!
24 мартаа 2023 года.
 Impact of COVID-19 hits hard as TB deaths among people living with HIV rise for the first time since 2006
Impact of COVID-19 hits hard as TB deaths among people living with HIV rise for the first time since 2006
23 мартаа 2022 года.
 TB disease and deaths declining among people living with HIV, but there have been some reversals due to the COVID-19 pandemic
TB disease and deaths declining among people living with HIV, but there have been some reversals due to the COVID-19 pandemic
23 мартаа 2022 года.
40 years of the AIDS response
08 июня 2021 года.
 Tuberculosis deaths among people living with HIV are declining globally, but worrying gaps in TB care persist
Tuberculosis deaths among people living with HIV are declining globally, but worrying gaps in TB care persist
24 мартаа 2021 года.
 Huge gaps in TB care for people living with HIV in some countries
Huge gaps in TB care for people living with HIV in some countries
24 мартаа 2021 года.
 Tuberculosis testing gap among people living with HIV is narrowing
Tuberculosis testing gap among people living with HIV is narrowing

15 февраля 2021 года.

Feature Story
WHO report highlights growing numbers of drug-resistant tuberculosis
19 марта 2010
19 марта 2010 19 марта 2010
For the first time, the WHO global report includes an assessment of progress countries are making in the diagnosis and treatment of multidrug-resistant TB.
Up to a quarter of people with tuberculosis in some regions can no longer be treated with standard drug regimens. This is the stark finding of a new World Health Organization report which estimates that 440,000 people had multidrug-resistant TB (MDR-TB) in 2008, a third of whom died.
Multidrug and Extensively Drug-Resistant Tuberculosis (M/XDR-TB): 2010 Global Report on Surveillance and Response presents data from 114 countries. It underlines that almost half of all cases of MDR-TB are estimated to occur in China and India. In Africa an estimated 69,000 cases emerged.
The report also explores the relationship between HIV and MDR-TB and notes that drug resistant TB among people living with HIV has been widely documented in certain settings, such as hospitals. It further states that TB patients co-infected with HIV in three Eastern European countries, Estonia, Latvia, and the Republic of Moldova, were found to be at greater risk of having multidrug-resistant tuberculosis compared to TB patients without HIV infection. Studies in Lithuania, Ukraine and Mozambique show similar results. More research is required to ascertain whether these findings would be replicated worldwide and the report notes that no data have been received from countries with the highest HIV prevalence.
According to UNAIDS, HIV-positive people are especially vulnerable to the impact of TB and MDR-TB. They are at increased risk of contracting the disease and experiencing serious side effects and are more likely to die if infected. HIV and TB are seen as so closely connected that they are often referred to as ‘co-epidemics’. To appropriately respond to both epidemics and avoid more widespread drug resistance, fully integrated TB/HIV services should be priority concern of all TB and HIV programmes.
Preventing people living with HIV dying from tuberculosis is one of the nine priority areas in the UNAIDS Outcome Framework 2009-11.

According to the WHO report only an estimated 7% of all MDR-TB patients are diagnosed. Credit: WHO/D.Orr
For the first time, the WHO global report includes an assessment of progress countries are making in the diagnosis and treatment of multidrug-resistant TB. Six countries are the subject of special focus. Bangladesh is one of the few developing nations carrying out continuous surveillance among TB cases which were previously treated in selected areas. China has reported results from its first ever drug resistance survey; Ethiopia was among the first countries to introduce rapid molecular laboratory tests. Nepal and Romania both have successful treatment programmes for MDR-TB and South Africa has introduced policy changes for improving management and care for those living with the disease.
Although there has been notable success in some countries, world-wide progress in controlling multidrug-resistant TB remains slow. According to the WHO report only an estimated 7% of all MDR-TB patients are diagnosed.
Of major concern is the very high cost of treating this form of the disease. The price of drugs alone is 50 to 200 times higher than treating a drug-susceptible TB patient. However, WHO maintains that treatment of MDR-TB has been shown to be cost-effective.
According to the report, there is an urgent need for drug regimens which are shorter than the current two year span, improvements in laboratory facilities and access to rapid diagnosis and treatment. WHO is undertaking a five-year project aimed at strengthening TB laboratories with rapid tests in some 30 countries. It is also working closely with a number of organisations to increase access to treatment so that more lives can be saved.
Note: Multi-drug resistant TB (MDR-TB) is tuberculosis that is resistant to at least Rifampicin and Isoniazid, the two most powerful anti-tuberculosis drugs. Extensively drug- resistant TB (XDR-TB) is MDR-TB that is also resistant to at least two out of the three classes of second line TB medicines.
WHO report highlights growing numbers of drug-res
Cosponsors:
Partners:
Feature stories:
Call for global action on the threat of drug-resistant tuberculosis (03 April 2009)
Call for fully funded Global Fund to fight AIDS, Tuberculosis and Malaria (31 March 2009)
UNAIDS Executive Director meets with TB Programme Managers, TB civil society (26 March 2009)
Need for scale up in integrated TB and HIV screening to address linked epidemics (24 March 2009)
TB deaths rise in people living with HIV (17 March 2008)
MDR-TB more common in people living with HIV (28 February 2008)
Publications:
Multidrug and Extensively Drug-Resistant Tuberculosis (M/XDR-TB): 2010 Global Report on Surveillance and Response (pdf, 850 Kb)
Related
 United for ending cervical cancer, HIV and inequities for women and girls
United for ending cervical cancer, HIV and inequities for women and girls

17 ноября 2022 года.
 Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners
Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners

16 ноября 2022 года.
 Key considerations to integrate HIV and mental health interventions
Key considerations to integrate HIV and mental health interventions

28 апреля 2022 года.

Feature Story
New data shows progress in addressing TB/HIV
08 декабря 2009
08 декабря 2009 08 декабря 2009
Some 36 million people have been cured of tuberculosis (TB) over the past 15 years through a rigorous approach to treatment endorsed by the World Health Organization (WHO). New data, released by WHO, also indicate that up to 8 million TB deaths have been averted, confirming the Stop TB Strategy as the most cost-effective approach in the fight against TB.
The WHO update also shows continued progress on addressing the lethal combination of TB and HIV. Between 2007 and 2008, 1.4 million TB patients were tested for HIV, an increase of 200, 000. Of those who tested HIV positive, one-third benefited from life-saving HIV anti-retroviral therapy (ART) and two-thirds were enrolled on co-trimoxazole prophylaxis to prevent the risk of fatal bacterial infections. In addition, screening for tuberculosis and access to isoniazid preventive therapy for TB among people living with HIV more than doubled, although the total number is still far short of what it should be.
"Fifteen years of TB investments are bringing visible results in terms of human lives saved. Together, national programmes, WHO, UNAIDS, the Global Fund and other partners have helped save millions of lives from TB," said Dr Mario Raviglione, Director of WHO's Stop TB Department. "But the current pace of progress is far from sufficient to decisively target our goal of TB elimination."
The WHO Stop TB Strategy has five elements: political commitment with increased and sustained financing, case detection through quality-assured bacteriology, standardized treatment with supervision and patient support, an effective drug supply and management system, monitoring and evaluation system and impact measurement.
Data from the latest 12 month period now show that the highest ever number of infectious patients - 2.3 million people - were cured. With 87% of treated patients cured, the 85% global target was exceeded for the first time since it was established in 1991. Furthermore, a total of 53 countries surpassed this treatment milestone.
Fifteen years of TB investments are bringing visible results in terms of human lives saved. Together, national programmes, WHO, UNAIDS, the Global Fund and other partners have helped save millions of lives from TB.
Dr Mario Raviglione, Director of WHO's Stop TB Department
Although more and more patients are being cured, there are millions who are being let down because they are unable to access high-quality care. TB remains second only to AIDS in terms of the number of people it kills. In 2008, 1.8 million people died from TB including half a million deaths in HIV related illness–many of them because they were not enrolled on ART.
A persistent challenge that is largely left unchecked in many parts of the world is multidrug-resistant TB (MDR-TB) and its even more dangerous form, extensively drug-resistant TB (XDR-TB). Of the estimated half a million MDR-TB cases occurring per year, almost 30 000 were officially reported and 6 000 were known to be treated according to WHO international standards in 2008. A major expansion of services is currently in an early and difficult phase but almost 29 000 people are expected to be treated in 2010.
Of the estimated 9.4 million TB cases in 2008 (including 1.4 million TB/HIV cases), 3.6 million cases occurred among women.
"Half a million women died from TB last year. It is a disease that destroys lives, damages families and stifles development," said Dr Mario Raviglione. "Without help to fill the US$ 2 billion funding gap for TB care and control in 2010, the most vulnerable people will continue to miss the benefits so many others have seen."
The new report provides the most accurate information on the global burden of tuberculosis. It also features updates about the work of the Global Laboratory Initiative, the WHO Global Task Force on TB Impact Measurement, and describes the success of a new initiative in 2009 in which global TB data collection went online.
New data shows progress in addressing TB/HIV
Cosponsors:
Partners:
Stop TB Partnership
The Global Fund
Feature stories:
UNAIDS Executive Director meets with TB Programme Managers, TB civil society (26 March 2009)
Publications:
Global tuberculosis control: a short update to the 2009 report
Contact:
For further information, please contact:
Glenn Thomas,
Senior Communications Adviser, Stop TB Department,
WHO +41 79 509 0677,
E-mail: thomasg@who.int
All WHO information can be found at www.who.int
Related
 United for ending cervical cancer, HIV and inequities for women and girls
United for ending cervical cancer, HIV and inequities for women and girls

17 ноября 2022 года.
 Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners
Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners

16 ноября 2022 года.
 Key considerations to integrate HIV and mental health interventions
Key considerations to integrate HIV and mental health interventions

28 апреля 2022 года.

Feature Story
MDR-TB more common in people living with HIV
28 февраля 2008
28 февраля 2008 28 февраля 2008
According to the 4th World Health Organization (WHO) report on anti-tuberculosis drug resistance released on 26 February, multi-drug resistant tuberculosis* (MDR TB) has been shown to be almost twice as common in tuberculosis (TB) patients living with HIV compared to TB patients without HIV.
The report presents the findings of the largest survey of TB drug resistance to date with information collected between 2002 and 2006 from 90,000 TB patients in 81 countries. It demonstrates the highest rates of MDR-TB ever recorded with nearly half a million new cases of MDR-TB worldwide each year––around 5% of the total 9 million new TB cases. It also found that extensively drug-resistant tuberculosis** (XDR-TB), a virtually untreatable form of the respiratory disease, has been recorded in 45 countries.
The true scale of the problem also remains unknown in some pockets of the world. Only six countries in Africa—the region with the highest incidence of TB in the world***––were able to provide drug resistance data for the report, and none of these were able to provide information on drug resistance in people living with HIV. Other countries in the region could not conduct surveys because they lack the equipment and trained personnel needed to identify drug-resistant TB.
‘This report confirms the serious threat that drug resistant TB poses to people living with HIV,’ said Alasdair Reid HIV/TB Adviser, UNAIDS. ‘UNAIDS, together with WHO and our international partners, is working with TB and HIV programmes in countries across the world to ensure they work more closely together to prevent the development and spread of drug-resistant TB among people living with HIV through better diagnosis and treatment of TB in people living with HIV and improved TB infection control in HIV care settings and communities affected by HIV’.
WHO estimates that US$ 4.8 billion is needed for overall tuberculosis control in low- and middle-income countries in 2008, with US$ 1 billion needed to respond to drug resistant tuberculosis. There is currently a gap in financing of US$ 2.5 billion, including a US$ 500 million gap for drug resistant tuberculosis.
NOTE TO EDITORS:
* The bacteria responsible for TB becomes resistant when people who are ill with TB are not provided with or do not complete a full course of medication. Drug-resistant TB, like drug-sensitive TB, can also be transmitted through the air from an infected person to a non-infected person. MDR-TB is a form of TB that does not respond to the standard six month treatment using first line-drugs (i.e. resistant to isoniazid and rifampicin). It can take two years to treat with drugs that are 100 times more expensive than first-line treatment.
** XDR-TB is a form of TB caused by bacteria resistant to virtually all the most effective anti-tuberculosis drugs (i.e. MDR-TB plus resistance to any fluoroquinolones and any one of the second-line anti-tuberculosis injectable drugs: amikacin, kanamycin or capreomycin).
*** In sub-Saharan Africa HIV is dramatically fuelling the spread of TB which is a major cause of death among people living with HIV. MDR-TB and XDR-TB are highly lethal in people living with HIV––studies show case fatality rates of over 90%. Drug-resistant TB is therefore a major threat to the effectiveness of both TB treatment and anti-retroviral treatment programs.
MDR-TB more common in people living with HIV
Cosponsors:
Related links:
Publications:
Anti-tuberculosis drug resistance in the world (pdf, 2.4 Mb)
Related
 United for ending cervical cancer, HIV and inequities for women and girls
United for ending cervical cancer, HIV and inequities for women and girls

17 ноября 2022 года.
 Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners
Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners

16 ноября 2022 года.
 Key considerations to integrate HIV and mental health interventions
Key considerations to integrate HIV and mental health interventions

28 апреля 2022 года.

Feature Story
Joining forces to tackle TB and HIV
24 ноября 2006
24 ноября 2006 24 ноября 2006 Photo credit : WHO
Photo credit : WHOTuberculosis (TB) is one of the biggest killers of people living with HIV and at least one third of the 39.5 million people estimated to be living with HIV around the world are likely to be infected with the TB bacteria. As a result of chronically poor investment in global TB control a new strain of TB is emerging that has become resistant to most of the available anti-tuberculosis drugs. Known as extensively drug resistant TB (XDR TB) this strain has serious implications for people living with HIV as it is almost untreatable in many of the countries where it is occurring leading to very high death rates. WHO and UNAIDS, together with other actors working on TB and HIV issues are stepping up action to stop the spread of TB and this deadly new strain.
TB is an infection which usually affects the lungs and is spread, like the common cold, through the air from an infectious person coughing, sneezing or even speaking. One third of the world’s population is infected with TB but only 5-10% of people who are infected with TB actually develop TB disease during their lifetimes. However, co-infection with HIV makes TB disease much more likely and one in ten people infected with TB who also have HIV will develop TB disease each year.
TB is treatable and can usually be cured in people living with HIV, however some strains of TB bacteria have now acquired resistance to one or more of the antibiotics commonly used to treat them; these are known as drug-resistant strains. Treatment for these infections is much longer and much more expensive. The recent outbreaks of tuberculosis that is resistant to almost all of the available TB drugs are giving serious cause for concern as this extensively drug resistant strain (XDR TB) is virtually untreatable when it occurs in people living with HIV and has a very high death rate.
UNAIDS has been following the developments closely. “We need to rapidly ensure prompt diagnosis and effective treatment of TB for people living with HIV in order to prevent drug resistance from developing and spreading,” said UNAIDS’ HIV/TB advisor, Alasdair Reid.
TB drug resistance arises mainly because of inadequate TB control, poor patient or clinician adherence to standard TB treatment regimens, poor quality drugs or inadequate drug supplies. People living with HIV are particularly vulnerable to developing drug-resistant TB because of their increased susceptibility to infection and progression to active TB.
At the 37th Union World Conference on Lung Health held in Paris in November 2006, the interaction between TB and HIV and the threat of extensively drug resistant TB featured prominently in the agenda. The serious implications of the new strain of XDR TB for people living with HIV were highlighted at a special plenary session held during the conference. Dr Kevin De Cock, Director of WHO HIV/AIDS Department said, “The recent emergence of a cluster of cases in South Africa has demonstrated the high mortality that XDR TB can have when associated with HIV infection. Countries with a high prevalence of HIV have been responding quickly to draw up plans for managing and preventing drug-resistant TB and this is welcomed.”
Because of the serious threat that TB and especially XDR TB poses for people living with HIV, UNAIDS and the WHO HIV and TB departments are joining forces to encourage a coordinated and concerted global effort to control TB in people living with HIV.
WHO’s Global Task Force on XDR TB have recently published a report outlining measures needed to urgently combat extensively drug-resistant XDR TB. It follows the announcement by WHO and its partners that US$ 95 million will be required to implement the recommendations in the report, to address the threat of XDR-TB in 2007 in southern Africa. WHO have also released new guidelines on how to improve the diagnosis of TB in people living with HIV.
Links:
Access WHO new guidelines.
Frequently asked questions about Tuberculosis and HIV.
WHO TB
Stop TB partnership
Presentations from the Union meeting on XDR TB can be viewed through the Kaisernetworks link on the Union website.
International Union Against Tuberculosis and Lung Disease
Related
 United for ending cervical cancer, HIV and inequities for women and girls
United for ending cervical cancer, HIV and inequities for women and girls

17 ноября 2022 года.
 Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners
Delays in global, affordable access to long-acting, injectable HIV medicines would cost lives, say AIDS campaigners

16 ноября 2022 года.
 Key considerations to integrate HIV and mental health interventions
Key considerations to integrate HIV and mental health interventions

28 апреля 2022 года.

Feature Story
New African resolve to combat AIDS, TB and Malaria
08 мая 2006
08 мая 2006 08 мая 2006
From right: Representative of UN Secretary General, Executive Director UNAIDS, Dr Peter Piot; President of Niger Republic, Mamodou Tandja and President Council of Senate Senegal, Mbaye-Jacques Diop on arrival for the opening session of the meeting of Heads of State and Government at the Special Summit of the African Union on HIV/AIDS, Tuberculosis and Malaria in Abuja
Photo: Sunday Aghaeze
African leaders and Heads of State recently met in Abuja, Nigeria at a Special Summit on HIV/AIDS, Tuberculosis and Malaria to address the challenges posed by the three diseases that kill an estimated four million Africans every year.
Organized by the African Union in collaboration with UN Agencies and other development partners, and at the invitation of Nigerian President Olusegun Obasanjo, the Special Summit adopted the Abuja Call for accelerated action towards Universal Access to AIDS, tuberculosis and malaria (ATM) services in Africa, and a resolution to achieve this by 2010. The delegates also adopted an African Common Position to be presented to the High Level Meeting on AIDS in June 2006.
In the Abuja Call, participants urged for intensified leadership at all levels; further commitments regarding human rights; increased mobilization of resources including negotiations for debt cancellation; and collective advocacy with multilateral and bilateral donors.
African leaders renewed their commitment to allocate 15% of their national budgets to health, and to incorporate health financing plans into national development plans.
“For the first time the political commitment exists to work towards Universal Access to HIV prevention, treatment and care, but getting this will require that once more we change gear and further accelerate the response to AIDS. We have no other options that will save entire societies”, said UNAIDS Executive Director Dr Peter Piot.
Nigerian President Olusegun Obasanjo commended African countries for the progress they had so far made in responding to AIDS, tuberculosis and malaria. The Nigerian leader called for the development of structures and systems guaranteeing better and more transparent utilization of funds, as well as for the development of strategies translating national level goals into community targets.

Press Conference after the closing of the Special Summit (left to right) Alpha Oumar Konaré, Chairperson of African Union Commission and former President of Mali; President Sassou-Nguesso of Republic of Congo, Chairman of the African Union; President Olusegun Obasanja of Nigeria, Host of the Special Summit and Alhaji Mamadou Tandja, President of Niger Republic
Photo: Sunday Aghaeze
Also speaking on the occasion, African Union Commission Chairperson, Prof. Alpha Konare, outlined measures Africa should adopt to successfully deliver AIDS, tuberculosis and malaria services. These include local production of essential medicines, greater mobilization of resources, more efficient utilization of resources, and ensuring access to the most vulnerable groups.
Sub-Saharan Africa has just over 10% of the world’s population, but is home to more than 60% of all people living with HIV - 25.8 million. In 2005, an estimated 3.2 million people in the region became newly infected, while 2.4 million adults and children died of AIDS. Among young people aged 15-24 years, an estimated 4.6% of women and 1.7% of men were living with HIV in 2005.
Related links
Read Statement of the UNAIDS Executive Director Dr Peter Piot at the Special Assembly of Heads of State and Government, Abuja, 4 May 2006
Photo gallery
3 April 2006
4 April 2006
Related
 Leave no one behind and that includes people who use drugs
Leave no one behind and that includes people who use drugs

04 мая 2023 года.
 Dangerous inequalities and overcoming them
Dangerous inequalities and overcoming them

18 ноября 2022 года.