Injecting drug use IDU


Feature Story
Launch of advocacy explainers on western Africa model drug law
28 September 2021
28 September 2021 28 September 2021Since the West Africa Commission on Drugs launched a groundbreaking model drug law in 2018, civil society across the region and beyond has been engaging stakeholders on the need to use the model law as a blueprint for national reform.
The model drug law promotes, among other things, the availability of harm reduction services as well as the decriminalization of possession of drugs for personal use, which have long been called for by UNAIDS.
As the model drug law is, by design, a long and technical document, UNAIDS supported the West Africa Drug Policy Network and the International Drug Policy Consortium to develop and disseminate two important new tools for civil society: a shorter and more accessible resource that summarizes the key points of the model drug law and a short guide for local nongovernmental organizations to explore how to use the model drug law in their work. In other words, the first advocacy explainer is about the key “ingredients” of the model drug law and the second contains a list of methods and strategies on how to use these ingredients to better integrate the law in their advocacy and to advance drug policy reform, based on experiences from the region.
The documents were launched on 27 September during a virtual webinar live on Facebook and can be found in English, French and Portuguese at https://www.wadpn.org/resources.
“These new tools will directly support and empower civil society advocacy for more health- and rights-based drug policies in western Africa and, in turn, strengthen the response to HIV among people who use drugs,” said Patrick Brenny, the Director of the UNAIDS Regional Support Team for West and Central Africa.
Adeolu Ogunrombi, a West Africa Commission on Drugs Commissioner, underlined that the needs and demands for drug dependence treatment and harm reduction are high, but service provision is low in the region, and specified that the law provides guidance on this. He also noted that criminalizing the possession of equipment and materials, such as needles, syringes and other paraphernalia, has been demonstrated to undermine harm reduction service provision and uptake and to have a damaging impact on public health.
A case study was presented by Chinwike Okereke, a civil society organization representative and focal point for the West Africa Commission on Drugs in Nigeria, on the use of the model drug law. In 2020, a coalition of civil society organizations made presentations on the model drug law to key policymakers, including the Federal Ministry of Justice, the Drug Law Reform Commission and the National Drug Law Enforcement Agency. “The model drug law presented an opportunity to have face-to-face discussions and drive a buzz on the reform that led to a drug law reform round table where all key federal, criminal justice and state actors and civil society made a case for the adoption of the law as a template for reform,” he said. Further engagement with the Drug Law Reform Commission then led to the setting-up of a working group that is actively working on reshaping drug laws in the country. He also encouraged civil society to use the new explainers and urged technical and funding partners to invest more funding for this effort across western Africa, as law reform takes some time to achieve.
Our work
Region/country




Feature Story
Small steps towards a big goal
21 June 2021
21 June 2021 21 June 2021On 29 June, one of the largest non-profit organizations based in Saint Petersburg, Russian Federation, is celebrating its twentieth anniversary. Humanitarian Action provides comprehensive medical and social assistance to people who use drugs, including services for the prevention of HIV, viral hepatitis and tuberculosis, following the principle of working with everyone, regardless of their lifestyle.
Humanitarian Action is the successor to Doctors of the World, which worked in the Russian Federation in the 1990s during an economic crisis that saw an increase in drug use and HIV and other infections.
Today, the main mission of Humanitarian Action is to improve the lives and health of people who use drugs, restore their dignity and raise public awareness about drug use. Its vision is, “A world in which people who use drugs do not die from an overdose, HIV, hepatitis, tuberculosis or suicide, have equal rights and opportunities, are not stigmatized and discriminated against and do not experience self-stigma.”
A converted tourist bus, known as the Blue Bus owing to its colour, and a converted minibus, the Little Bus, allow Humanitarian Action to work as close as possible to where people who use drugs live and congregate. A joint project with the Saint Petersburg AIDS centre provides home visits via mobile units to seriously ill people living with HIV, many of whom are former drug users who have been left behind by mainstream services.
The organization offers personal protective equipment against bloodborne and sexually transmitted infections, including sterile syringes and needles, condoms, etc., and exchanges syringes. In its medical centre—a first of its kind in the Russian Federation, since it provides help through low-threshold programmes—doctors provide anonymous and free medical services in a range of specialities for people who use drugs, sex workers, homeless people and migrants.
People also can also get psychological services from Humanitarian Action. Legal advice on the restoration of documents, guardianship or problems with the law and medical and social support for HIV, hepatitis or tuberculosis diagnosis and treatment are also available.
“Not everyone is ready to change their life immediately. We help people learn to take responsibility for their health and change gradually, moving from one tiny victory to another,” said Alexey Lakhov, the Development Director of Humanitarian Action. “We are a kind of bridge between people who use drugs and various government and nongovernment services. It’s just that with us, it becomes easier to get such help thanks to partnerships with multiple social and medical services.”
The process of helping people who use drugs is based on the principle of taking small steps and is aimed at gradually introducing safer behaviours: do not start using drugs; if you have started, stop; if you use drugs, stop injecting them; if you do inject drugs, always use a sterile syringe; if it is not possible to use a sterile needle every time, at least never use someone else’s; if using someone else’s syringe, always disinfect it.
Some of Humanitarian Action’s employees are themselves former drug users, who share their stories with clients, helping those who wish to quit by referring them to appropriate services.
“We congratulate Humanitarian Action on its twentieth anniversary. We hope that by its thirtieth anniversary we will also be able to celebrate the end of AIDS and the elimination of all forms of stigma and discrimination against people affected by HIV,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025


Feature Story
Pioneers of the harm reduction response in Uganda
07 May 2021
07 May 2021 07 May 2021The drop-in centre of the Uganda Harm Reduction Network (UHRN) looks lonely from the deserted suburban pavement. It is a non-descript house, hidden behind an imposing solid pink steel gate, in an equally non-descript neighbourhood.
It looks like so many other drop-in centres in eastern Africa that serve key populations—anonymous and low-key. Necessary characteristics, perhaps, in a region that mostly criminalizes people who use drugs, gay men and other men who have sex with men, sex workers and transgender people.
Once through the gate, visitors are greeted with a hive of activity that belies the quiet exterior. Clients and staff are buzzing around, setting up chairs under the makeshift gazebo in the verdant garden. In a few minutes, a group of people who use drugs will take part in a harm reduction workshop run by one of the centre’s staff. There is also a consulting room at the front of the drop-in centre; and at the back, is the office of Wamala Twaibu.
Mr Twaibu is the founder and chairperson of the Eastern Africa Harm Reduction Network and UHRN. A self-styled “former drug user with roots in Uganda and the pioneer of the harm reduction movement in eastern Africa,” Mr Twaibu has a kind face and a penetrating gaze that tells a story of adversity, resilience and triumph.
In the consulting room, 25-year-old Kemigisa Sandriano, a heroin user and sex worker, is taking an HIV test conducted by the centre’s resident doctor, Mukiibi Grace Nickolas. The night before, Ms Sandriano was assaulted by a client after he took off the condom during sex. She protested, telling him to leave. Her swollen, bloodshot right eye attests to what happened after that. She is smiley and talkative, seemingly unbothered by yet another instance of violence at the hands of a client. She is happy that in his battle to get his money back, she won.
Ms Sandriano was introduced to heroin by her ex-husband, who she says “ruined” her life. Nevertheless, she is upbeat about her recovery.
“I have the hope that I can stop. I even went to rehab for three months. When I saw my days of rehab coming to an end, I saw no plan and I started again,” she says.
“I am ready to go to rehab again,” she continues. “But when I come out, I don’t want to be idle. When they take us out of rehab, we need a job. They can say to us, “Work in a supermarket, work in this shop, so you can stabilize.””
Employment aside, Mr Twaibu says medically assisted treatment for people with opioid dependence is critical for rehabilitation. And, since, December 2020, with advocacy from UHRN and financial support from the United States President’s Emergency Plan for AIDS Relief and the Centers for Disease Control and Prevention, the first medically assisted treatment services in Uganda have been available at the Butabika National Mental Referral Hospital in Kampala.
UHRN screens and provides initial preparation for eligible clients and refers and links them to the hospital and provides them with ongoing psychosocial support services. In December 2020, there were 81 people who use drugs enrolled in medically assisted treatment.
Besides medically assisted treatment, through its drop-in centre UHRN offers a comprehensive package of health services, including behaviour change communication, a needle–syringe programme, psychosocial support, overdose management, HIV testing and counselling and sexually transmitted infection screening.
The COVID-19 pandemic posed a major challenge to UHRN’s clients, who even under normal circumstances face high levels of stigma and discrimination, police abuse and harassment, alienation and limited access to health and social services.
Sex workers, transgender men and women, people who use drugs and gay men lost livelihoods and faced even more violence and detention under the guise of lockdown measures. Movement was severely limited as motor vehicles required a special permit to operate.
UHRN rose to the challenge. A team of 25 peer educators used bicycles, funded by Frontline AIDS, and motorcycles to reach their clients where they were, providing antiretroviral medicine refills and condoms to clients who could not reach health facilities.
The organization rolled out virtual counselling services on risk reduction and addiction management through phone calls and WhatsApp. As part of personal protective equipment procurement, UNAIDS, through the National Forum of People Living with HIV/AIDS Networks in Uganda, provided soap and bleach to prevent COVID-19 infection among the drop-in centre’s dedicated staff, who worked right through the pandemic.
Despite the constraints of the pandemic, UHRN’s needle–syringe programme reached 287 clients in 2020, providing more than 15 000 clean needles and syringes, tourniquets, cotton balls, swabs, water ampoules, condoms, lubricant and safe-injecting information notes.
“I’m proud that harm reduction issues are taking a centre stage in Uganda,” says Mr Twaibu. “Community-led means ownership. Usually when the community is at the centre, accountability and community needs are prioritized,” he says.
Our work
Resources
Region/country
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025




Feature Story
Specialized medical waste management equipment for Republic of Moldova’s harm reduction programme
06 May 2021
06 May 2021 06 May 2021The Union for HIV Prevention and Harm Reduction is a nongovernmental organization located in Balti, in the Republic of Moldova. It provides integrated services to people who use drugs and other affected populations throughout the north of the country.
Each year, more than 3000 people benefit from its services, which including mobile testing for HIV, sexually transmitted infections and hepatitis, harm reduction services, including a needle–syringe programme, the distribution of condoms and psychological and social support. The organization’s outreach and medical workers work closely with state clinics and hospital departments that offer opioid substitution therapy to people who use drugs.
However, the organization has faced a long-time logistical problem with regard to the collection of used needles and syringes generated by the harm reduction programme. Medical waste disposal in the Republic of Moldova, especially in the north of the country, is problematic. Ala Iatco, the nongovernmental organization’s head, explained that destruction of used equipment was only possible by contracting medical institutions to do the work and that the union had to send boxes with contaminated waste to Chisinau, the capital of the country.
“For the approximately 20 years of the harm reduction programme in the country, this problem was always present and solved through burning needles and syringes or other non-environmentally-friendly ways. We had to find a solution to increase the effectiveness of the comprehensive package of services and enhance the safety and security of personnel and volunteers while operating the needle–syringe programme,” said Svetlana Plamadela, UNAIDS Country Manager for the Republic of Moldova.
The UNAIDS Country Office for the Republic of Moldova, together with the United Nations Office on Drugs and Crime and the union, came together and suggested a solution. In July 2017, specialized modern medical waste management equipment was procured from the Russian Federation and installed within a Union for HIV Prevention and Harm Reduction facility. The total cost of US$ 23 000 was funded with resources from the One UN Joint Action to Strengthen Human Rights in the Transnistrian Region of the Republic of Moldova project, financed with the support of the Swedish Embassy and co-funded by the Center for Health Policies and Studies (PAS Center), which is a Principal Recipient of the Global Fund to Fight AIDS, Tuberculosis and Malaria.
“The availability of the one-stop disposal system provided by the needle smelters and syringe cutters significantly reduces the risk of accidental exposure and contamination with bloodborne diseases by the volunteers and medical personnel,” added Ms Plamadela.
So far, three organizations—the Union for HIV Prevention and Harm Reduction, Young Women Cernoleuca and Adolescent!—have benefited from the needle–syringe destruction equipment. Partner organizations usually make monthly shipments of needles and syringes for destruction, which are collected by field workers in eco-boxes.
According to Ms Iatco, the equipment is easy to use and maintain. “The machine transforms the contaminated syringes and needles into biologically safe waste. We save almost 50% of the cost of destruction. And, most importantly, we face much fewer risks as we avoid transportation, storage and transfer of hazardous material. For our organization, located in a remote area where no such equipment is available in medical institutions, it’s a cost-effective and less risky solution,” she said.
The needle–syringe programme in the Republic of Moldova started in 1999. Its main goal is to prevent the transmission of HIV and other infections among people who inject drugs by avoiding the sharing of injecting equipment and ensuring enhanced access to health-care services and psychosocial support. The programme also aims to curb the sexual transmission of HIV among people who inject drugs and their sexual partners by promoting the use of condoms and raising awareness about the link between drug use and risky sexual behaviours.
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025


Feature Story
High rates of hepatitis C and HIV coinfection among key populations
26 April 2021
26 April 2021 26 April 2021Viral hepatitis infection is a major global public health problem causing approximately 1.4 million deaths per year—more than the annual number of AIDS-related deaths. Ninety-six per cent of these deaths are from cirrhosis and hepatocellular carcinoma due to hepatitis B and C viruses, which are transmitted via blood and body fluids.
People living with HIV and hepatitis B or hepatitis C coinfection have a more rapid progression to cirrhosis. Liver disease has emerged as an important cause of death among people living with HIV coinfected with either hepatitis B or hepatitis C.
Hepatitis C coinfection with HIV is reported across all key populations at higher risk of HIV, especially among people who inject drugs. This is due to the ease with which both viruses are spread through the sharing of non-sterile drug preparation and injecting equipment.
Our work


Feature Story
Commission on Narcotic Drugs discusses how COVID-19 is impacting the world drug problem
15 April 2021
15 April 2021 15 April 2021The 64th regular session of the Commission on Narcotic Drugs—the policymaking body of the United Nations with prime responsibility for drug-related matters—is being held from 12 to 16 April, at which the anniversaries of the 1961 Single Convention on Narcotic Drugs and the 1971 Convention on Psychotropic Substances are being marked.
In addition to the opening, operational and normative segments, more than 100 side events are taking place addressing various aspects of drug programmes and policies, including the impact of COVID-19. Five resolutions are being debated, including one on the impact of the COVID-19 pandemic on the implementation of Member States’ joint commitments to address and counter the world drug problem.
The normative session is looking at the implementation of the international drug control treaties, including the follow-up to the implementation at the national, regional and international levels of all commitments, as reflected in the ministerial declaration of 2019, as well as the inter-agency coordination of efforts in addressing and countering drugs.
In addition, the session will see deliberation on the contributions by the Commission on Narcotic Drugs to the work of the United Nations Economic and Social Council, including follow-up to and review and implementation of the 2030 Agenda for Sustainable Development.
The opening segment included a message from the United Nations Secretary-General, who noted that the COVID-19 crisis has shown the world how much the world needs solidarity, shared responsibility and international cooperation to improve health coverage.
Speaking for UNAIDS at the opening plenary, Ninan Varughese, a UNAIDS Senior Adviser, noted that the new global AIDS strategy calls for the intensification and redoubling of efforts to scale up comprehensive harm reduction for people who inject drugs in all settings and commits to promote and support community-led responses. He added that the engagement of key populations, including people who inject drugs, is critical to a successful HIV response everywhere and reminded the plenary of UNAIDS’ call on all leaders to come together to support the High-Level Meeting on AIDS from 8 to 10 June 2021.
Documents
Legal and policy trends impacting people living with HIV and key populations in Asia and the Pacific 2014–2019
14 January 2021
This report provides a summary of key developments in the legal environment for HIV responses in Asia and the Pacific. It is the product of a desk review conducted for UNAIDS and the United Nations Development Programme (UNDP) in 2019. The report highlights key trends and developments in laws affecting people living with HIV and key populations in Asia and the Pacific over the five-year period 2014–2019. It updates the legal and policy review conducted in 2016 for UNAIDS, UNDP and the United Nations Economic and Social Commission for Asia and the Pacific (ESCAP). A database of laws of the 38 Member States of ESCAP was created as part of this review. The database identifies laws that are either punitive or enabling for people living with HIV and key populations in Asia and the Pacific. A summary of the findings is presented in Annex 1. An overview poster is also available.
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024


Feature Story
Dakar addiction centre reaches out to women
04 December 2020
04 December 2020 04 December 2020The Centre de Prise en Charge Intégrée des Addictions de Dakar (CEPIAD), which opened in December 2014, is an addiction reference centre in Dakar for Senegal and the wider region. To date, it has cared for 1200 people, including approximately 250 people currently enrolled on its opioid substitution therapy programme.
In Senegal, HIV prevalence among people who inject drugs is 3.7%, well above the average of 0.4% among the general population. HIV prevalence is higher among female drug users (13%) than among men (3%), but women represent less than 10% of CEPIAD’s active caseload. In response, CEPIAD has reached out to women who inject drugs. With the support of UNAIDS, and in collaboration with the Conseil National De Lutte Contre le Sida, CEPIAD organized a week of activities around World AIDS Day to address the specific needs of women.
“Women were at the heart of the organization of this week. We want to remove the misrepresentations and misunderstandings that hinder their attendance at the centre,” said Ibrahima Ndiaye, Deputy Coordinator of CEPIAD.
Women were able to access HIV and hepatitis C screening services, gynaecology consultations, including cervical cancer screening, and addiction counselling. Talks with female drug users and a debate on harm reduction were organized on 1 December, World AIDS Day.
A three-day training on making soap, using honey, aloe vera, shea butter, palm oil and mbeurbeuf, and a batik workshop were also offered. More than 50 women participated and the products were sold on the closing day of the week of activities.
Ndeye Khady, the founder of the batik workshop, is a former crack smoker who is currently accessing opioid substitution therapy and antiretroviral therapy at CEPIAD, where she met her husband, also a former drug user. “My dream now is to have a child. I am so grateful that I have been able to take advantage of the services offered. I encourage more women to use them,” she said.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025

Press Release
UNAIDS calls on countries to step up global action and proposes bold new HIV targets for 2025
26 November 2020 26 November 2020As COVID-19 pushes the AIDS response even further off track and the 2020 targets are missed, UNAIDS is urging countries to learn from the lessons of underinvesting in health and to step up global action to end AIDS and other pandemics
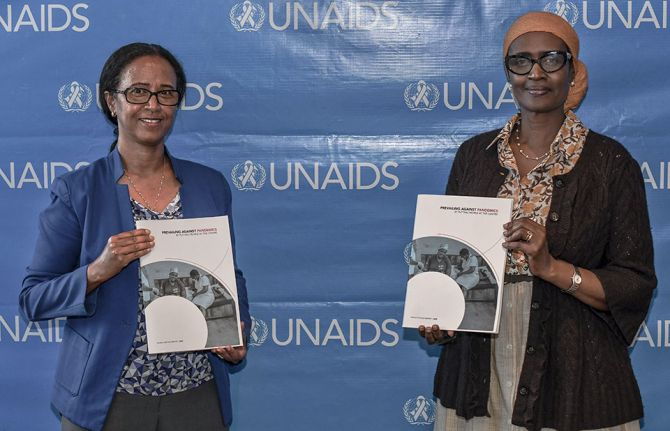
GENEVA, 26 November 2020—In a new report, Prevailing against pandemics by putting people at the centre, UNAIDS is calling on countries to make far greater investments in global pandemic responses and adopt a new set of bold, ambitious but achievable HIV targets. If those targets are met, the world will be back on track to ending AIDS as a public health threat by 2030.
The global AIDS response was off track before the COVID-19 pandemic hit, but the rapid spread of the coronavirus has created additional setbacks. Modelling of the pandemic’s long-term impact on the HIV response shows that there could be an estimated 123 000 to 293 000 additional new HIV infections and 69 000 to 148 000 additional AIDS-related deaths between 2020 and 2022.
“The collective failure to invest sufficiently in comprehensive, rights-based, people-centred HIV responses has come at a terrible price,” said Winnie Byanyima, Executive Director of UNAIDS. “Implementing just the most politically palatable programmes will not turn the tide against COVID-19 or end AIDS. To get the global response back on track will require putting people first and tackling the inequalities on which epidemics thrive.”
New targets for getting back on track
Although some countries in sub-Saharan Africa, such as Botswana and Eswatini, have done remarkably well and have achieved or even exceeded the targets set for 2020, many more countries are falling way behind. The high-performing countries have created a path for others to follow. UNAIDS has worked with its partners to distil those lessons into a set of proposed targets for 2025 that take a people-centred approach.
The targets focus on a high coverage of HIV and reproductive and sexual health services together with the removal of punitive laws and policies and on reducing stigma and discrimination. They put people at the centre, especially the people most at risk and the marginalized—young women and girls, adolescents, sex workers, transgender people, people who inject drugs and gay men and other men who have sex with men.
New HIV service delivery targets aim at achieving a 95% coverage for each sub-population of people living with and at increased risk of HIV. By taking a person-centred approach and focusing on the hotspots, countries will be better placed to control their epidemics.
The 2025 targets also require ensuring a conducive environment for an effective HIV response and include ambitious antidiscrimination targets so that less than 10% of countries have punitive laws and policies, less than 10% of people living with and affected by HIV experience stigma and discrimination and less than 10% experience gender inequality and violence.
Prevailing against pandemics
Insufficient investment and action on HIV and other pandemics left the world exposed to COVID-19. Had health systems and social safety nets been even stronger, the world would have been better positioned to slow the spread of COVID-19 and withstand its impact. COVID-19 has shown that investments in health save lives but also provide a foundation for strong economies. Health and HIV programmes must be fully funded, both in times of plenty and in times of economic crisis.
“No country can defeat these pandemics on its own,” said Ms Byanyima. “A challenge of this magnitude can only be defeated by forging global solidarity, accepting a shared responsibility and mobilizing a response that leaves no one behind. We can do this by sharing the load and working together.”
There are bright spots: the leadership, infrastructure and lessons of the HIV response are being leveraged to fight COVID-19. The HIV response has helped to ensure the continuity of services in the face of extraordinary challenges. The response by communities against COVID-19 has shown what can be achieved by working together.
In addition, the world must learn from the mistakes of the HIV response, when millions in developing countries died waiting for treatment. Even today, more than 12 million people still do not have access to HIV treatment and 1.7 million people became infected with HIV in 2019 because they did not have access to essential HIV services.
Everyone has a right to health, which is why UNAIDS has been a leading advocate for a People’s Vaccine against COVID-19. Promising COVID-19 vaccines are emerging, but we must ensure that they are not the privilege of the rich. Therefore, UNAIDS and partners are calling on pharmaceutical companies to openly share their technology and know-how and to wave their intellectual property rights so that the world can produce successful vaccines at the huge scale and speed required to protect everyone.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton-Knott
tel. +41 79 514 68 96
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 4237
communications@unaids.org
Press centre
Download the printable version (PDF)


Update
Key populations have suboptimal knowledge of their HIV status
26 October 2020
26 October 2020 26 October 2020There are significant gaps in HIV testing among key populations at higher risk of HIV infection, resulting in suboptimal levels of knowledge of their HIV status. HIV testing is a critical gateway to HIV prevention and treatment services. Without knowledge of HIV status, people cannot access life-prolonging HIV treatment services.
Analysis of data from special surveys shows that, on average, about two thirds of sex workers and gay men and other men who have sex with men globally either had taken an HIV test and received the results within the past 12 months or had previously tested positive for HIV—meaning that about one third did not know their HIV status. This testing gap was even larger for people who inject drugs. These surveys are often conducted where key population-friendly services are available and may overstate overall testing coverage.