Sex workers and clients
Documents
UNAIDS data 2024
02 December 2024
Suggested citation. UNAIDS DATA 2024. Geneva: Joint United Nations Programme on HIV/AIDS; 2024. Licence: CC BY-NC-SA 3.0 IGO. Related: The 2024 global AIDS report The Urgency of Now: AIDS at a Crossroads, released 22 July 2024, is available here.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Documents
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
The world’s decades-long response to HIV is at an inflection point. Despite successes, the world is currently not on track to end AIDS as a public health threat by 2030. Press release | Download full report | Download short version
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025




Feature Story
New Asia Pacific healthcare provider toolkit serves people having chemsex
13 November 2024
13 November 2024 13 November 2024Life became chaotic for Poon early. (Not his real name.)
As a gay teenager he was bullied at school by students and teachers. He moved in with his grandparents when his parents separated, but eventually left northern Thailand for Bangkok. There he survived through sex work.
Then Poon learned he was living with HIV. The weight of HIV prejudice merged with the stigma he already carried as a young gay man and sex worker. Some friends he made at a camp disclosed his HIV status online after an argument. He was diagnosed with major depressive disorder.
A partner introduced him to drug-use during sex. He went on to use multiple substances including methamphetamines and cocaine.
“Sex, drugs and alcohol are my escape,” he said.
This was one of the stories shared at the 6th Asia Pacific Chemsex Symposium (APCS). Held in Bangkok on November 6 and 7, the event brought together over 300 stakeholders from 27 countries. They shared their research and responses to a practice that remains largely hidden and not yet well understood. The event specifically explored pleasure as opposed to risk as an entry point for providing services.
Chemsex—also called High Fun in several Asian countries—refers to the use of stimulant drugs during sexual activity. It lowers inhibitions and may increase risk-taking. There are several public health implications including higher rates of HIV and sexually transmitted infections (STIs), lower adherence to treatment, overdose and the fallout linked with intoxication.
In Asia Pacific four of every five new HIV infections are among people from key population communities including men who have sex with men or MSM, people who use drugs, people in prisons or other closed settings, sex workers and transgender people. Young people make up a quarter of all new HIV infections and in some countries around half of new infections are among youth ages 15 to 24.
Several countries in the region are facing an HIV prevention crisis with new infections among MSM either increasing or decreasing far too slowly. In 2023, 43% of new infections in Asia-Pacific were among MSM. At the same time, there is evidence that the practice of chemsex in this community ranges from 3% to 31% depending on the country. But although chemsex is most visible in the MSM community, it is practiced by people from all populations.
“We are talking about sex and drugs—two topics that people call taboo,” said Brigitte Quenum, UNAIDS Regional Team Lead for Sciences, Systems and Services at the opening ceremony. “But as HIV has taught us, to reach people, we must confront the realities of their lives.”
Toolkit now available for Asia Pacific health workers
On day 2 of the symposium UNAIDS and UNODC launched the first-ever toolkit on chemsex for Asia Pacific clinical service providers. The toolkit was developed by the Australian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM). It is geared toward health workers in Asia and the Pacific working with men who have sex with men and transgender women.
"The increasing use of stimulant drugs in the region, including for ‘Chemsex’, poses significant health risks, including drug use disorders and various psychosocial challenges," said Masood Karimipour, Regional Representative of UNODC’s Office for Southeast Asia and the Pacific. "This UNAIDS-UNODC toolkit provides essential guidance for healthcare providers to address these challenges through evidence-based interventions. It emphasizes the importance of holistic, non-judgmental care that prioritizes the physical, psychological and social wellbeing of individuals, while ensuring access to harm reduction services and the prevention and treatment of drug use disorders within a comprehensive continuum of care."
The resource was created to support comprehensive clinical services in the region’s restrictive legal environments. Twenty-eight countries in Asia Pacific criminalise drug possession for personal use while 17 criminalise same-sex relations. Penalties for drug-related offences in the region are among the world’s harshest.
The toolkit was developed through consultation with clinicians, community representatives and government agencies. It covers chemsex basics as well as approaches to harm reduction, sexual health, and mental health services. It also covers different service delivery models including face-to-face, online and by communities. The toolkit offers guides and tools on topics such as initiating non-judgmental conversations and risk assessment.
“Stronger HIV prevention strategies tailored to chemsex are needed, along with expanded, inclusive services for sexual, physical and mental health,” said Suniya Taimour, UNAIDS’ Community-led Responses Advisor for Pakistan and Afghanistan.
Thia approach recognises that comprehensive health services can be lifesavers by using one point of contact to address multiple issues including physical, sexual and mental health as well as social issues. Poon is a living example. He has benefitted from a service package that has combined his HIV treatment with harm reduction interventions and psychiatric care. Today he is a 22-year-old university student with clear life goals who feels more empowered about his HIV status.
Our work
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Documents
HIV and sex workers — Thematic briefing note — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Sex workers are disproportionally affected by HIV. In 2022, the relative risk of acquiring HIV was nine times higher for sex workers than for people in the wider population globally, declining from 12 times higher in 2010. In sub-Saharan Africa, annual numbers of sex workers with newly acquired HIV dropped by 50% between 2010 and 2022 according to new modelled estimates. Numbers of new infections among sex workers remain the same outside sub-Saharan Africa and are increasing in some countries. Criminalization of any aspect of sex work, other punitive laws, interpersonal and institutional violence, and stigma and discrimination remain significant barriers to achieving social justice and equality for sex workers, and ensuring health for all through access to and uptake of HIV and sexual and reproductive health services. A median of 26% of sex workers have reported experiencing violence in the past 12 months (20 reporting countries). Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
Slide deck - 2024 global AIDS update
22 July 2024
Core epidemiology slides
22 July 2024
Documents
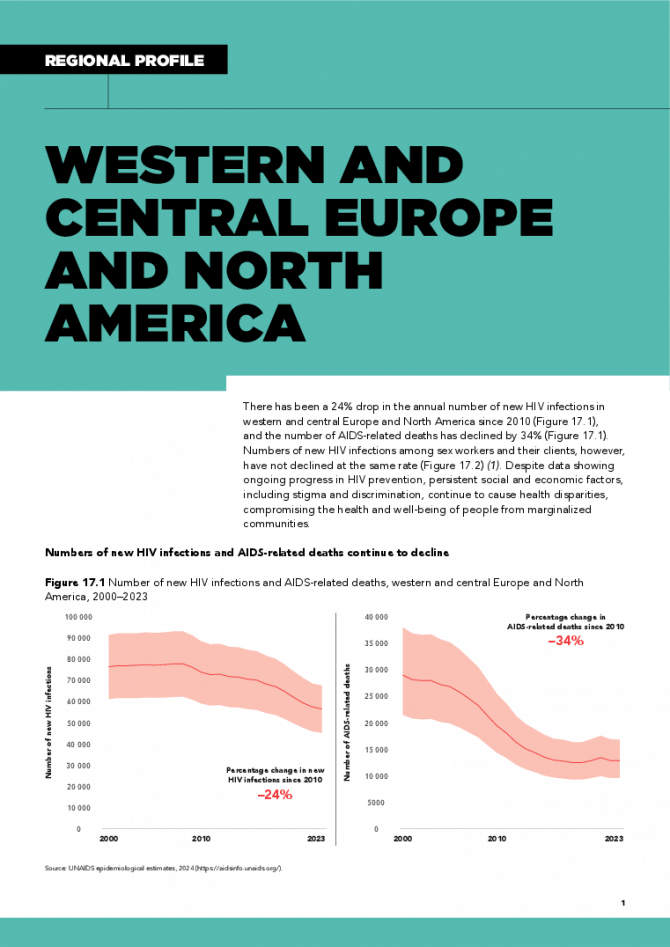
Western and Central Europe and North America regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
There has been a 24% drop in the annual number of new HIV infections in western and central Europe and North America since 2010, and the number of AIDS-related deaths has declined by 34%. Numbers of new HIV infections among sex workers and their clients, however, have not declined at the same rate. Despite data showing ongoing progress in HIV prevention, persistent social and economic factors, including stigma and discrimination, continue to cause health disparities, compromising the health and well-being of people from marginalized communities. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025
Documents
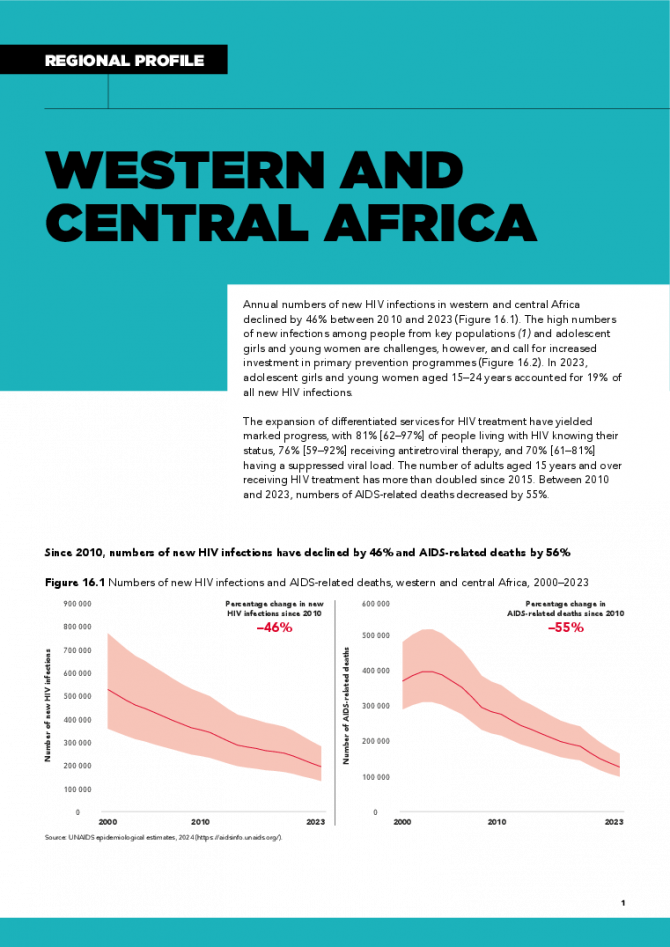
Western and Central Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Annual numbers of new HIV infections in western and central Africa declined by 46% between 2010 and 2023. The high numbers of new infections among people from key populations and adolescent girls and young women are challenges, however, and call for increased investment in primary prevention programmes. In 2023, adolescent girls and young women aged 15–24 years accounted for 19% of all new HIV infections. The expansion of differentiated services for HIV treatment have yielded marked progress, with 81% [62–97%] of people living with HIV knowing their status, 76% [59–92%] receiving antiretroviral therapy, and 70% [61–81%] having a suppressed viral load. The number of adults aged 15 years and over receiving HIV treatment has more than doubled since 2015. Between 2010 and 2023, numbers of AIDS-related deaths decreased by 55%. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
Documents
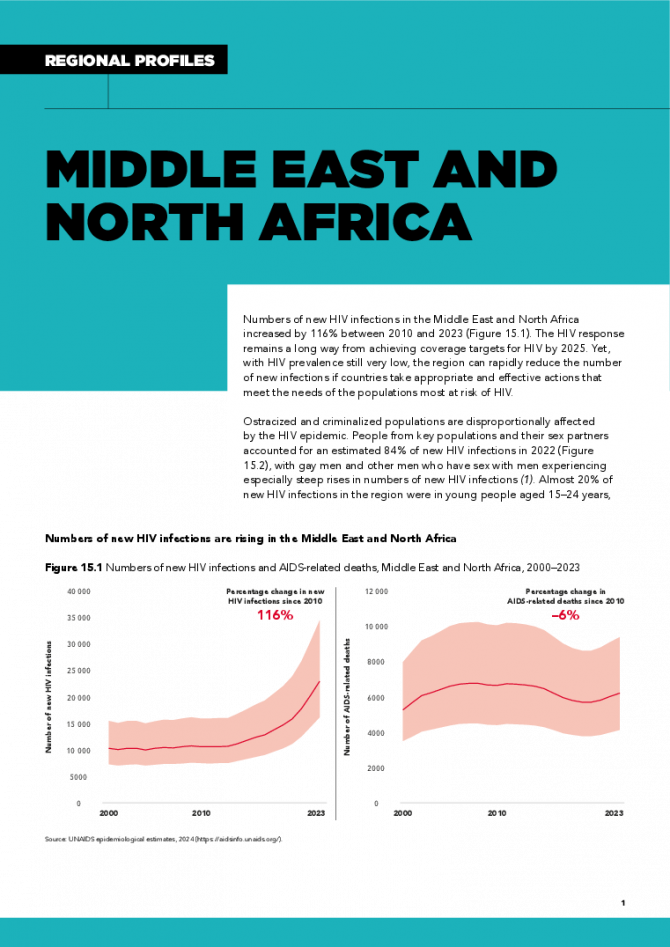
Middle East and North Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Numbers of new HIV infections in the Middle East and North Africa increased by 116% between 2010 and 2023. The HIV response remains a long way from achieving coverage targets for HIV by 2025. Yet, with HIV prevalence still very low, the region can rapidly reduce the number of new infections if countries take appropriate and effective actions that meet the needs of the populations most at risk of HIV. Ostracized and criminalized populations are disproportionally affected by the HIV epidemic. People from key populations and their sex partners accounted for an estimated 84% of new HIV infections in 2022, with gay men and other men who have sex with men experiencing especially steep rises in numbers of new HIV infections. Almost 20% of new HIV infections in the region were in young people aged 15–24 years, the majority of them male (55%). These epidemic patterns underscore the need for scaled-up HIV interventions for people from key populations and especially young people, and for reducing the societal and structural barriers that limit their access to needed services. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
Documents
Latin America — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
The annual number of new HIV infections in Latin America increased by 9% between 2010 and 2023, with eight countries experiencing increases since 2015. In 2022, a significant proportion (66%) of new HIV infections were among people from key populations and their sex partners. In 2022, numbers of new HIV infections were 20% higher than in 2010 among gay men and other men who have sex with men, 42% higher among sex workers, and 19% higher among transgender women. Numbers of AIDS-related deaths have decreased by 28% since 2010 overall, but increased among women in Costa Rica, El Salvador, Mexico, Panama, Paraguay and Peru. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 The critical impact of the PEPFAR funding freeze for HIV across Latin America and the Caribbean
The critical impact of the PEPFAR funding freeze for HIV across Latin America and the Caribbean
19 February 2025
Documents
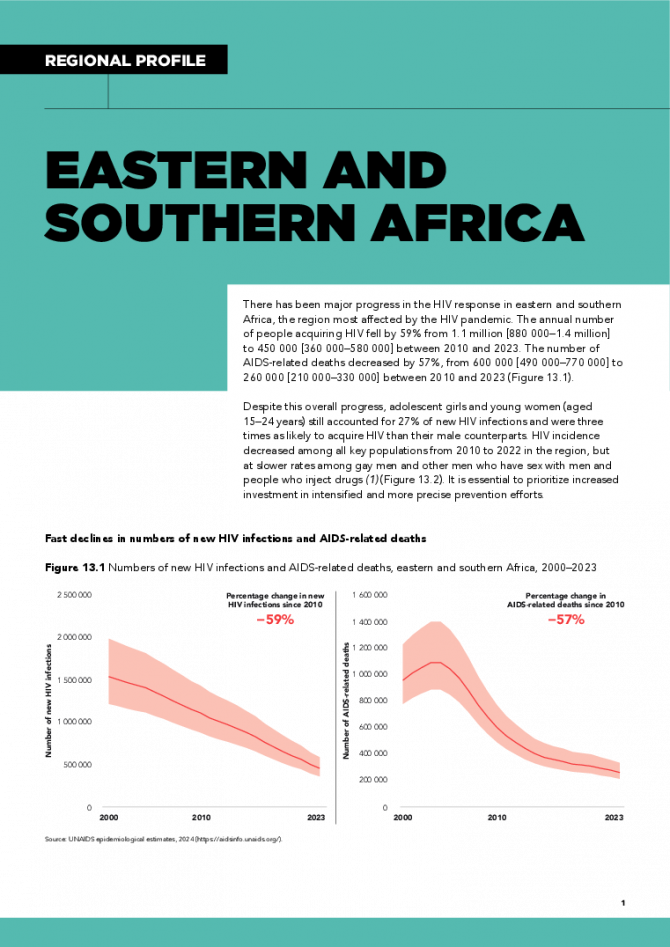
Eastern and Southern Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
There has been major progress in the HIV response in eastern and southern Africa, the region most affected by the HIV pandemic. The annual number of people acquiring HIV fell by 59% from 1.1 million [880 000–1.4 million] to 450 000 [360 000–580 000] between 2010 and 2023. The number of AIDS-related deaths decreased by 57%, from 600 000 [490 000–770 000] to 260 000 [210 000–330 000] between 2010 and 2023. Despite this overall progress, adolescent girls and young women (aged 15–24 years) still accounted for 27% of new HIV infections and were three times as likely to acquire HIV than their male counterparts. HIV incidence decreased among all key populations from 2010 to 2022 in the region, but at slower rates among gay men and other men who have sex with men and people who inject drugs. It is essential to prioritize increased investment in intensified and more precise prevention efforts. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025
Documents
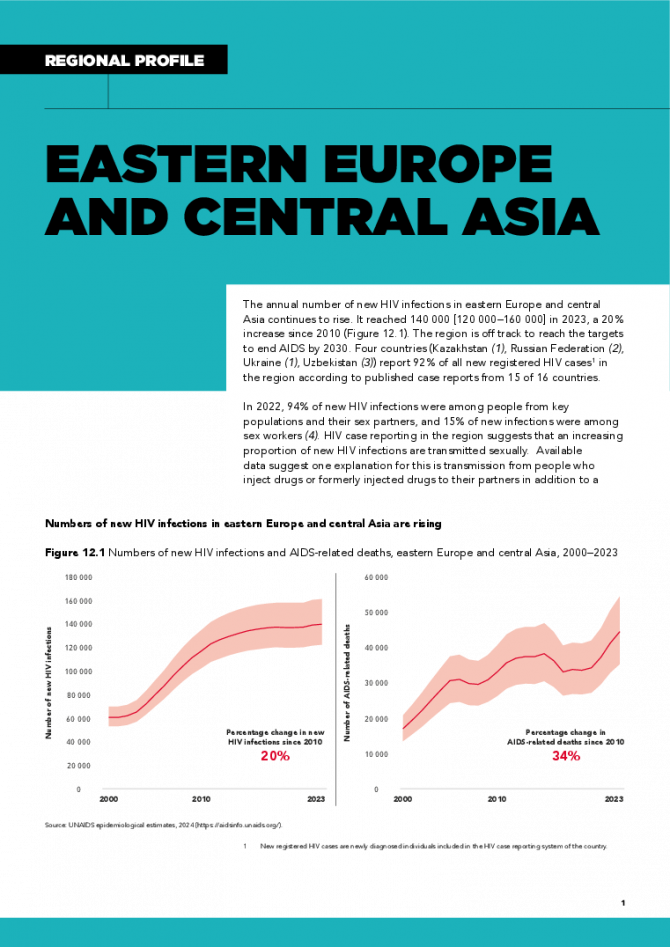
Eastern Europe and Central Asia regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
The annual number of new HIV infections in eastern Europe and central Asia continues to rise. It reached 140 000 [120 000–160 000] in 2023, a 20% increase since 2010 . The region is off track to reach the targets to end AIDS by 2030. Four countries (Kazakhstan, Russian Federation, Ukraine, Uzbekistan) report 92% of all new registered HIV cases in the region according to published case reports from 15 of 16 countries. In 2022, 94% of new HIV infections were among people from key populations and their sex partners, and 15% of new infections were among sex workers. HIV case reporting in the region suggests that an increasing proportion of new HIV infections are transmitted sexually. Available data suggest one explanation for this is transmission from people who inject drugs or formerly injected drugs to their partners in addition to a growing recognition of transmission among men who have sex with men. Unsafe drug injecting practices are a key factor in the region’s epidemic, representing 27% of new HIV infections. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025