Sex workers and clients
Documents
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 July 2024
This UNAIDS 2024 report brings together new data and case studies which demonstrate that the decisions and policy choices taken by world leaders this year will decide the fate of millions of lives and whether the world’s deadliest pandemic is overcome. Related links: Press release | Special web site | Executive summary | Fact sheet | Video playlist | Epidemiology slides | Data on HIV | Annex 2: Methods Regional profiles: Asia and the Pacific | Caribbean | Eastern Europe and Central Asia | Eastern and Southern Africa| Latin America | Middle East and North Africa | Western and Central Africa | Western and Central Europe and North America Thematic briefing notes: People living with HIV | Gay men and other men who have sex with men | Transgender people | Sex workers | People who inject drugs | People in prisons and other closed settings | Adolescent girls and young women | Other translations: German
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025




Press Statement
To protect sex workers’ health, protect their human rights
02 June 2024 02 June 2024GENEVA, 2 June 2024—On International Sex Workers’ Day, 2nd June 2024, and every day, UNAIDS stands in solidarity with sex workers in support of their health.
Intersecting forms of structural and societal stigma and discrimination, including punitive laws, policies and practices, widen inequalities and prevent sex workers from being able to protect their health, safety and well-being. Criminalization creates barriers to enabling access to and uptake of vital HIV prevention, testing and treatment, and to sexual and reproductive health services. For sex workers who are transgender, migrants or from racial and ethnic minorities, multiple and intersecting forms of discrimination create additional barriers to services and increase risks of facing violence and harassment.
A study in sub-Saharan Africa found that the likelihood of living with HIV was seven times higher for a sex worker in a country that criminalizes sex work compared with a country that decriminalized sex work. Another review found that criminalization of any aspect of sex work was associated with reduced condom access and use and increased rates of violence. Decriminalization of sex work could avert between 33% and 46% of HIV infections among sex workers and their clients over a ten-year period.
Among countries reporting to UNAIDS, 22% of sex workers had experienced stigma and discrimination in the past six months. 12% of sex workers had avoided accessing health-care services due to stigma and discrimination in the past 12 months. One in five sex workers experienced violence in the past 12 months.
Currently 168 countries have punitive laws that criminalize some aspect of sex work. But a growing number of jurisdictions are recognizing the need to decriminalize sex work to protect sex workers. In May this year Queensland in Australia became the latest jurisdiction to decriminalize sex work.
“To protect sex workers’ health, leaders need to accelerate action to tackle the stigma, discrimination and violence that sex workers face. This will require decriminalization. The evidence is clear: punitive laws hurt sex workers and need to be removed,” said Christine Stegling, Deputy Executive Director, UNAIDS.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Documents
The BBS-lite: A methodology for monitoring programmes providing HIV, viral hepatitis and sexual health services to people from key populations — UNAIDS–WHO 2024 Implementation Tool
22 May 2024
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
UNAIDS data 2024
02 December 2024
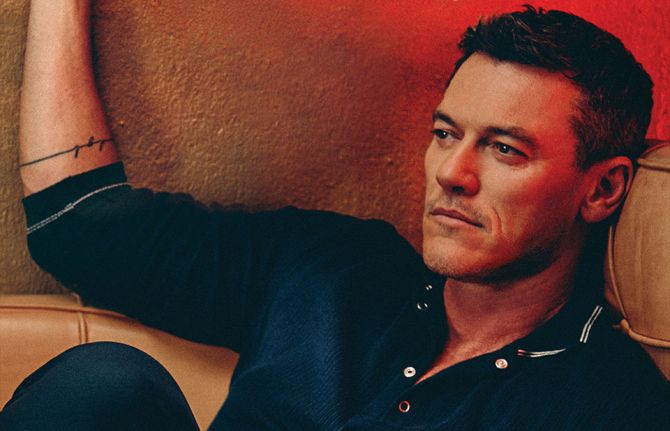
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
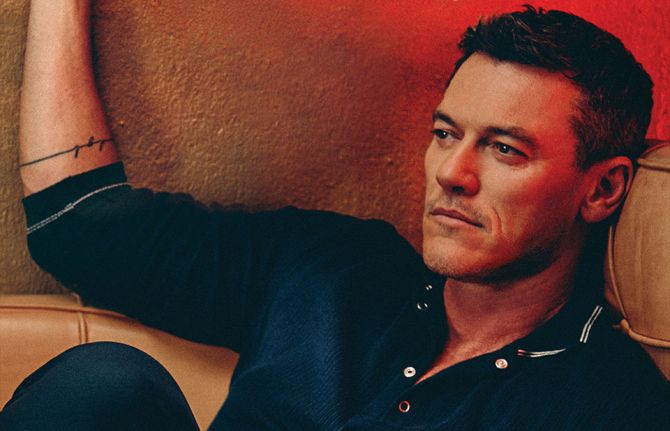
01 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
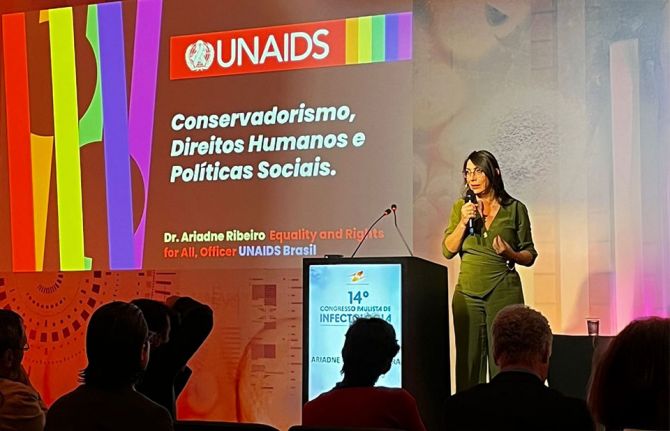
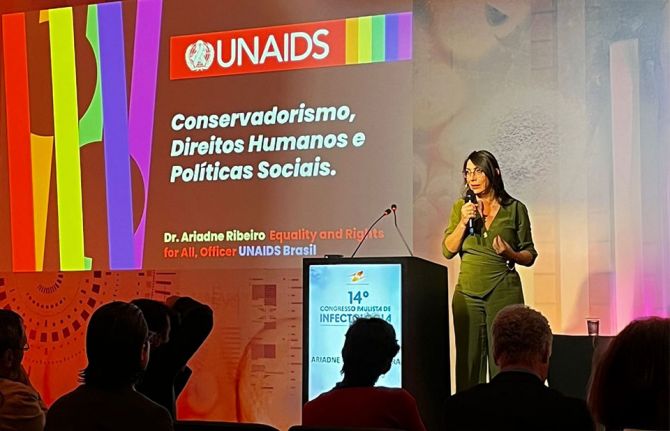 Upholding dignity for everyone: Ariadne Ribeiro Ferreira
Upholding dignity for everyone: Ariadne Ribeiro Ferreira
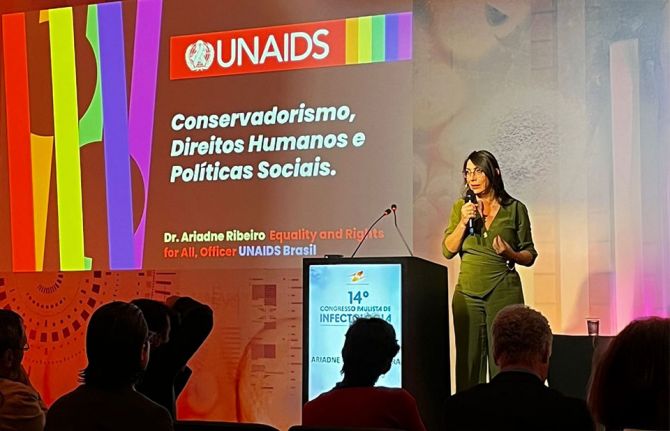
21 November 2024
Documents
New HIV infections data among key populations: proportions in 2010 and 2022
25 March 2024
The context of the HIV epidemics and total adult infection trends differ notably between sub-Saharan Africa and elsewhere. In sub-Saharan Africa, overall, the number of adult infections among people 15–49 years old fell markedly between 2010 to 2022, from 1.1 million to 510000 (54% decline). However, the rest of the world has not seen declines in new HIV infections among adults between 2010 and 2022, which stood at 580 000 in both years (1% increase using unrounded numbers).
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
01 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Upholding dignity for everyone: Ariadne Ribeiro Ferreira
Upholding dignity for everyone: Ariadne Ribeiro Ferreira
21 November 2024
Documents
Summary — Let Communities Lead — UNAIDS World AIDS Day report 2023
28 November 2023
This report is not only a celebration of the critical role of communities. It is a call to action to decision-makers to fully support the life-saving work of communities and to clear away the barriers that stand in their way. Press release | Full report | Fact sheet | World AIDS Day 2023
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025

Press Release
Ahead of World AIDS Day UNAIDS is calling for urgent support to Let Communities Lead in the fight to end AIDS
30 November 2023 30 November 2023A new report by UNAIDS demonstrates the critical role communities play, and how underfunding and harmful barriers are holding back their lifesaving work and obstructing the end of AIDS.
LONDON/GENEVA, 28 November 2023—As World AIDS Day (1 December) approaches, UNAIDS is urging governments across the world to unleash the power of grassroots communities across the world to lead the fight to end AIDS. A new report launched today by UNAIDS, Let Communities Lead, shows that AIDS can be ended as a public health threat by 2030, but only if communities on the frontlines get the full support they need from governments and donors.
“Communities across the world have shown that they are ready, willing and able to lead the way. But they need the barriers obstructing their work to be pulled down, and they need to be properly resourced,” said Winnie Byanyima, Executive Director of UNAIDS. “Too often, communities are treated by decision-makers as problems to be managed, instead of being recognised and supported as leaders. Communities are not in the way, they light the way to the end of AIDS.”
The report, launched in London during a World AIDS Day event organized by the civil society organization STOPAIDS, shows how communities have been the driving force for progress.
Community advocacy from the streets to the courtrooms to parliaments has secured groundbreaking changes in policy. Communities’ campaigning helped open up access to generic HIV medicines, leading to sharp, sustained reductions in the cost of treatment from US$ 25 000 per person per year in 1995 to less than US$ 70 in many countries most affected by HIV today.
Let Communities Lead shows that investing in community-led HIV programmes delivers transformational benefits. It sets out how programmes delivered by community-based organizations in Nigeria were associated with a 64% increase in access to HIV treatment, a doubling of the likelihood of HIV prevention service utilization, and a four-fold increase in consistent condom use among people at risk of HIV. It also notes how, among sex workers reached by a package of peer-based services in the United Republic of Tanzania, the HIV incidence rate was reduced to below half (5% vs 10.4%).
“We are the vehicle for change that can end systematic injustices that continue to fuel HIV transmission. We have seen groundbreaking developments with U=U, improved access to medicines, and have made great strides in decriminalisation," said Robbie Lawlor, Co-Founder of Access to Medicines Ireland. “Yet, we are expected to move mountains without being financially supported. We are supposed to fight for a more equitable world and are tasked with dismantling stigma yet are side-lined in crucial discussions. We are at a tipping point. Communities can no longer be relegated to the periphery. The time for leadership is now.”
The report highlights how communities are at the forefront of innovation. In Windhoek, Namibia, a self-funded project by the youth Empowerment Group is using e-bikes to deliver HIV medicines, food and adherence support to young people who often cannot attend clinics due to their schooling hours. In China, community organizations developed smartphone apps that link people to self-testing which contributed to a more than four-fold increase in HIV tests across the country from 2009 to 2020.
The report reveals how communities are also holding service providers to account. In South Africa five community networks of people living with HIV inspected 400 sites across 29 districts and conducted more than 33 000 interviews with people living with HIV. In the Free State province, these findings led provincial health officials to implement new appointment protocols to reduce clinic wait times and three- and six-month dispensing of antiretroviral medicines.
“I am extremely concerned about the exclusion from health services of key populations like the LGBT+ community,” said Andrew Mitchell, Minister of State for Development and Africa. “The UK champions the rights of such communities, and we will continue to protect them, working closely with our partners in civil society. I thank UNAIDS for keeping us focused on the inequities driving the pandemic and I look forward to working with our partners to champion the voice of people living with HIV and end AIDS as a public health threat by 2030.”
Despite the clear evidence of community-led impact, community-led responses are unrecognized, under-resourced and in some places even under attack. Crackdowns on civil society and on the human rights of marginalized communities are obstructing communities from providing HIV prevention and treatment services. Underfunding of community-led initiatives is leaving them struggling to continue operating and holding them back from expansion. If these obstacles are removed, community-led organizations can add even greater impetus to end AIDS.
In the 2021 Political Declaration on ending AIDS, United Nations member states recognized the critical role communities play in HIV service delivery, particularly to people most at risk of HIV. However, whereas in 2012, when over 31% of HIV funding was channelled through civil society organizations, ten years later, in 2021, only 20% of funding for HIV was available—an unprecedented backsliding in commitments which has cost and is continuing to cost lives.
“At this time, community-led action is the most important countermeasure in the AIDS response,” said Solange Baptiste, Executive Director of the International Treatment Preparedness Coalition. “Yet, shockingly, it isn’t a cornerstone of global plans, agendas, strategies, or financing mechanisms for improving pandemic preparedness and health for all. It is time to change that.”
Every minute, a life is lost to AIDS. Every week, 4000 girls and young women become infected with HIV, and out of the 39 million people living with HIV, 9.2 million do not have access to lifesaving treatment. There is a Path that Ends AIDS and AIDS can be ended by 2030, but only if communities lead.
UNAIDS is calling for: Communities’ leadership roles to be made core in all HIV plans and programmes; Communities’ leadership roles to be fully and reliably funded; And for barriers to communities’ leadership roles to be removed.
The report features nine guest essays from community leaders, in which they share their experience on the achievements they have secured, the barriers they face, and what the world needs to end AIDS as a public health threat.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaSophie Barton Knott
tel. +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
communications@unaids.org
UNAIDS Geneva
Michael Hollingdale
tel. +41 79 500 2119
hollingdalem@unaids.org
World AIDS Day message
World AIDS Day 2023
Watch the launch
World AIDS Day report
World AIDS Day videos



Feature Story
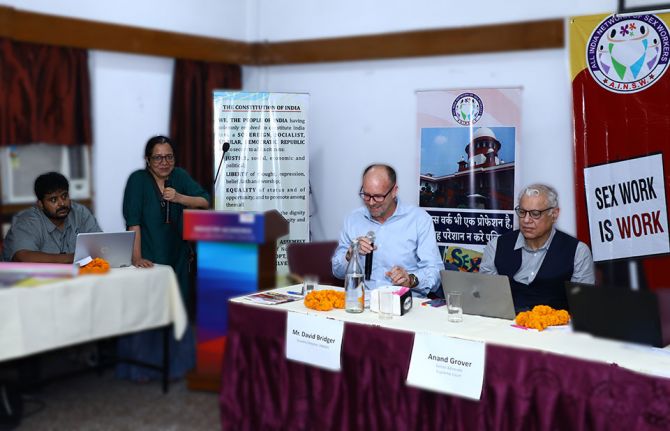
Indian partners reflect on a year after sex workers’ human rights affirmed
05 October 2023
05 October 2023 05 October 2023In 2022, the Indian Supreme Court ruled that sex workers were covered by Article 21 of the Constitution which assures every person the right to life. It recognized that sex workers are entitled to equal protection under the law.
The court instructed both central and state governments that sex workers should not be arrested, penalised, harassed or victimised during brothel raids. (Running a brothel is illegal in India. Individual sex work is not.) Nor should the possession of condoms and other safer sex commodities be treated as evidence of an offence. And the police should be sensitised to the community’s rights.
Moreover, the court also stressed the vital need to uphold the basic protection of human decency for the children of sex workers who, “bearing the brunt of social stigma… are removed to the fringes of the society, deprived of their right to live with dignity”. This ruling will help ensure that the children of sex workers can access essential services, including healthcare and education.
To commemorate this landmark judgment, the All-India Network of Sex Workers (AINSW) conducted a three-day National Consultation titled ‘Sisterhood and Solidarity with Sex Workers: One Year Since the Historic Supreme Court Ruling of 2022’. AINSW has been working on the issues of sex worker rights since 2011 across several states.
“Laws make a difference,” said David Bridger, UNAIDS Country Director to India in his keynote address. “The Supreme Court ruling was historic because with this, India joins a handful of countries like Canada and New Zealand that have explicitly instituted legal protection for sex workers. Recognizing the equal worth and dignity of every person is not only ethical, but also critical for ending AIDS.”
While giving an overview of the Supreme Court ruling, Senior Advocate, Anand Grover, noted that sex workers have taken steps which have contributed to the decline of HIV in India by negotiating condom use with their clients. A 2021 study found that 98% of sex workers used condoms. The work to educate and empower this community to have safer sex is paying off. HIV prevalence among female sex workers is now just under 2%. Protecting the safety and human rights of key populations expands their access to HIV services, accelerating progress in the response to HIV.
Mr Grover called for a full understanding of the law and how it impacts the lives of sex workers. He also stressed the importance of community participation in law and policy development, noting that the Court itself called for sex workers to be involved in decision-making processes linked to issues which affect them.
Shyamala Natraj, Executive Director of the South India AIDS Action Programme (SIAAP), briefed the audience about what went into making the 2022 ruling possible. She said the judgment was the result of strategic and consistent advocacy which centred on the lived experiences of sex workers.
In 2020, for example, the National Human Rights Commission issued an advisory recognising sex workers as entitled to the same social protection as other informal workers for the first time. Sex workers had been among the hardest hit during the COVID-19 pandemic. Not only did they experience an abrupt loss of income, but some were excluded from state social safety net responses. The fallout was extreme, including hunger, homelessness, debt, depression, and even suicide.
The SIAAP shared an example from Usha Ram (not her real name) from the town of Theni: “I did not have money to pay rent. The house owner forced me to vacate and humiliated me in front of my neighbours for doing sex work. I was on the streets with my children and did not even get the advance back.”
Ms Natraj encouraged the community to assert their human rights and secure access to the services that would ordinarily be provided to them under the law, including the issue of Aadhar (identification) cards, rations, poverty alleviation support and proof of residence documentation.
But despite the Supreme Court’s ruling that “sex work is a profession” with the same human rights as others, and that sex workers should not be harassed by the police, inequalities, stigma, and discrimination persist. Many sex workers are still reporting police harassment; some say they are still charged for soliciting clients.
To safeguard the human rights of sex workers, experts reiterated the need to implement the Supreme Court judgment at the grassroots level. UNAIDS and its cosponsors are committed to working with communities, policy makers and law enforcement to increase awareness and to ensure the universal upholding of sex workers’ human rights.
Our work
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025








Feature Story
Addressing violence against women sex workers in Peru
27 July 2023
27 July 2023 27 July 2023Ángela Villón Bustamante has been a sex worker and human rights activist for her community in Peru for almost 25 years. She has experienced first-hand the violence against sex workers. After she was beaten by a policeman in 1996, she began her activism.
"I don't want anyone else to end up almost dead like I did. The organization Miluska Vida y Dignidad (Miluska Life and Dignity, in English) is the organisation I created almost 30 years ago to find justice for those of us violated by public forces", recalls Ángela. "It was the first sex workers' organisation in Peru, and its name is in honour of my dear friend Miluska, who died after being beaten by one of them."
In the same years, transgender woman Alejandra Fang also was imprisoned for sex work, and a police officer asked her to have sex to be released. "I was forced into sex because, as a trans woman, I had no alternative. As a result of that traumatic situation, I decided to become an activist," says Alejandra.
Like Ángela, Alejandra also turned her negative experiences into opportunities for others so that no one would have to go through the same situations. She then became part of the Casa Trans Zuleymi and now leads Trans Organizacion Feminista (Feminist Trans Organization).
According to the Peruvian Ombudsman's Office, 95.8% of trans women have been victims of violence, 62.2% are engaged in sex work due to lack of employment opportunities, and only 5.1% have completed secondary education.
More than 10 cis and transgender sex workers have been murdered since the beginning of this year in Peru – four transgender sex workers in one week alone, by February 1. "This situation spread to other provinces in Peru, and sex workers had to go into hiding for weeks to protect their lives," says Ángela. "We have been unable to work and care for our basic personal and family needs."
The criminalisation of sex workers prevents them from seeking justice when they are harassed, physically harmed, or otherwise discriminated against. "We often do not report abuse to avoid further mistreatment and because of the stigma attached to our occupation," explains the activist.
"Whether they are living with HIV, migrants, Afro-descendants or indigenous– all these intersections generate exponential stigma and discrimination and place them in extreme vulnerability," says UNAIDS Director for the Andean Countries (Peru, Ecuador, Bolivia, and Colombia), Andrea Boccardi. "It puts them in such a precarious situation that it makes it difficult to access health services, food security, employment, education, and justice. Although self-employed sex work in Peru is legal, they have always been criminalized."
Given the situation of violence against sex workers in Peru, the organizations led by Angela and Alejandra, along with other organizations such as the Asociación Civil T.S. Rosas Mujeres de Lucha, are among those implementing a plan with the Peruvian Ministry of Women and Vulnerable Populations to address violence against sex workers in the country.
More than 100 police officers have already been trained by courses designed and facilitated by cis and transgender sex workers. The training provided knowledge on human rights, stigma, and discrimination, and their essential role as guarantors of justice to contribute to adopting a human rights-based approach in their work throughout the country.
Besides coordinating and facilitating a working group to fight violence and promote the fundamental rights of sex workers with several local and regional organizations and networks, UNAIDS has also partnered with the Public Defender's Office of the Ministry of Justice and Human Rights of Peru and with representatives of the sex workers' community to develop a protocol for the provision of legal assistance and victim advocacy services to sex workers.
"After so many years, I feel that our voice is now being heard," says Ángela.
Related resources
Find out more about HIV criminalization:
Region/country
Related


Press Release
New report from UNAIDS shows that AIDS can be ended by 2030 and outlines the path to get there
13 July 2023 13 July 2023GENEVA, 13 July 2023—A new report released today by UNAIDS shows that there is a clear path that ends AIDS. This path will also help prepare for and tackle future pandemics and advance progress towards achieving the Sustainable Development Goals. The report, ‘The Path that Ends AIDS’, contains data and case studies which highlight that ending AIDS is a political and financial choice, and that the countries and leaders who are already following the path are achieving extraordinary results.
Botswana, Eswatini, Rwanda, the United Republic of Tanzania, and Zimbabwe have already achieved the “95-95-95” targets. That means 95% of the people who are living with HIV knowing their HIV status, 95% of the people who know that they are living with HIV being on lifesaving antiretroviral treatment, and 95% of people who are on treatment being virally suppressed. A further 16 other countries, eight of them in sub-Saharan Africa, the region which accounts for 65% of all people living with HIV, are also close to doing so.
“The end of AIDS is an opportunity for a uniquely powerful legacy for today’s leaders,” said Winnie Byanyima, Executive Director of UNAIDS. “They could be remembered by future generations as those who put a stop to the world’s deadliest pandemic. They could save millions of lives and protect the health of everyone. They could show what leadership can do.”
The report highlights that HIV responses succeed when they are anchored in strong political leadership. This means following the data, science, and evidence; tackling the inequalities holding back progress; enabling communities and civil society organizations in their vital role in the response; and ensuring sufficient and sustainable funding.
Progress has been strongest in the countries and regions that have the most financial investments, such as in eastern and southern Africa where new HIV infections have been reduced by 57% since 2010.
Thanks to support for and investment in ending AIDS among children, 82% of pregnant and breastfeeding women living with HIV globally were accessing antiretroviral treatment in 2022, up from 46% in 2010. This has led to a 58% reduction in new HIV infections among children from 2010 to 2022, the lowest number since the 1980’s.
Progress in the HIV response has been strengthened by ensuring that legal and policy frameworks do not undermine human rights, but enable and protect them. Several countries removed harmful laws in 2022 and 2023, including five (Antigua and Barbuda, the Cook Islands, Barbados, Saint Kitts and Nevis, and Singapore) that have decriminalized same-sex sexual relations.
The number of people on antiretroviral treatment worldwide rose almost fourfold, from 7.7 million in 2010 to 29.8 million in 2022.
However, the report also sets out that ending AIDS will not come automatically. AIDS claimed a life every minute in 2022. Around 9.2 million people still miss out on treatment, including 660 000 children living with HIV.
Women and girls are still disproportionately affected, particularly in sub-Saharan Africa. Globally, 4,000 young women and girls became infected with HIV every week in 2022. Only 42% of districts with HIV incidence over 0.3% in sub-Saharan Africa are currently covered with dedicated HIV prevention programmes for adolescent girls and young women.
Almost one quarter (23%) of new HIV infections were in Asia and the Pacific where new infections are rising alarmingly in some countries. Steep increases in new infections are continuing in eastern Europe and central Asia (a rise of 49% since 2010) and in the Middle East and North Africa (a rise of 61% since 2010). These trends are due primarily to a lack of HIV prevention services for marginalized and key populations and the barriers posed by punitive laws and social discrimination.
Funding for HIV also declined in 2022 from both international and domestic sources, falling back to the same level as in 2013. Funding amounted to US$ 20.8 billion in 2022, far short of the US$ 29.3 billion needed by 2025.
There is an opportunity now to end AIDS by increasing political will by investing in a sustainable response to HIV through financing what matters most: evidence-based HIV prevention and treatment, health systems integration, non- discriminatory laws, gender equality, and empowered community networks.
“We are hopeful, but it is not the relaxed optimism that might come if all was heading as it should be. It is, instead, a hope rooted in seeing the opportunity for success, an opportunity that is dependent on action,” said Ms Byanyima. “The facts and figures shared in this report do not show that as a world we are already on the path, they show that we can be. The way is clear.”
In 2022, an estimated:
- 39.0 million people globally were living with HIV
- 29.8 million people were accessing antiretroviral therapy
- 1.3 million people became newly infected with HIV
- 630 000 people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Watch: roundtable discussion
Quote sheet for media
Social media assets




Feature Story
How to build stigma-free key population services
23 June 2023
23 June 2023 23 June 2023At his previous factory job, Tom Wang (not his real name) says coworkers gossiped about his sexuality and made fun of him. When he visited a public health facility for an HIV test, the nurse peppered him with questions like “Why do you need it? Have you been sleeping with many partners?”
Thailand is a country famed for its tolerance. It is among the world’s top locations for gender affirming care. Same-sex sexual activity hasn’t been criminalised since 1956. And the policy tide is turning on other key population issues. A 2021 Drug Law allows for harm reduction as opposed to automatic imprisonment, while a bill is in the pipeline to affirm the rights of sex workers. Yet stigma and discrimination persist. In homes, communities, schools, workplaces and—critically—healthcare settings, discriminatory attitudes can take their toll.
“Microaggressions—intentional or unconscious verbal or behavioural slights toward stigmatised groups—can drive people away from HIV prevention and treatment,” noted UNAIDS Regional Human Rights and Law Adviser, Quinten Lataire. “There are evidence-based approaches for measuring and lowering both overt and subtle stigma and discrimination in healthcare settings.”
It was this need for stigma-free services that led to the establishment of the Rainbow Sky Association of Thailand (RSAT). RSAT offers sexual healthcare for men who have sex with men, migrants, people who use drugs, sex workers and transgender people. It also advocates for the full rights and equity of lesbian, gay, bisexual and transgender (LGBT) communities. Tom Wang is amongst the clients who have benefited from their support.
This work is critical if HIV programmes are to reach and retain key population communities. In Thailand, as in the rest of Asia, these groups carry the heaviest HIV burden. Nationally HIV prevalence is 1% for sex workers, 8% for people who use drugs, 11% for transgender women and 12% for men who have sex with men.
A one stop shop for sexual health services
RSAT’s approach demonstrates how programmes can improve outcomes by implementing strategies to affirm and empower clients. They are jointly supported by PEPFAR, USAID, EpiC, the National Health Security Office (NHSO) and Thailand’s Institute of HIV Research and Innovation (IHRI).
There are no depressing charts or drab walls at their five key population clinics. At the Bangkok site the rainbow motif appears on the floors and walls. There are swarms of cut-out butterflies. Signs are either upbeat and multi-coloured or a soothing blue.
Most of the staff are themselves members of key population groups. All staff receive anti-stigma and discrimination training which even addresses the fine point of body language. Nothing about staff’s interactions should make a client feel judged or uncomfortable. The entire team is retrained annually. There is an internal complaint mechanism that allows clients to confidentially flag issues, as well quality assurance staff to ensure Standard Operating Procedures are followed. Every team member signs a confidentiality agreement.
RSAT’s service package includes on-site testing for HIV and other sexually transmitted infections, Hepatitis C, Tuberculosis and Covid-19. For transgender clients they offer hormone level monitoring. Mental health screenings which evaluate for depression, anxiety and stress have been integrated into the HIV service package. Where required, clients are referred for additional mental healthcare.
“Many of our clients engage in chem sex (recreational drug-use during intercourse). Some clients inject meth so we need to provide more than condoms. They also need clean syringes and needles which are part of our harm reduction package,” said Deputy Director, Kao Kierati Panpet.
Pre- and post-test counselling are critical. All counsellors are certified and accredited by the Ministry of Public Health according to Counsellor Supervisor, Sasiprapha Khamthi. Even before receiving HIV test results, clients know that treatment is available. Following a positive test, the counsellors reassure clients that with treatment they can live a normal life, explained Niphon Raina, Care and Counselling Supervisor.
“We also ask what their concerns are and give basic information about how HIV is and is not transmitted, using a picture book so they are clear on the facts,” Care and Counseling Officer, Bussarin Poonvisitkun added.
RSAT keeps a stock of antiretroviral therapy drugs onsite and can initiate new clients’ treatment on the day of diagnosis by giving them one month’s supply. Although HIV care is provided at the Ratchaphiphat Hospital, RSAT is able to dispense right away in accordance with instructions from a hospital doctor, delivered via telemedicine. Clients living with HIV receive help from the care and support team to navigate their next steps, including attending hospital visits.
RSAT also provides pre-exposure prophylaxis or PrEP services with hospital supervision. Mr. Tom Wang explains how this has protected his health: “I decided to get on PrEP because I am changing partners. To me PrEP is another means of protection in case you are intoxicated or the condom breaks. It’s a way to ensure I stay HIV-free.”
A redress mechanism for rights violations
The organisation advocates for structural changes to eliminate stigma and discrimination. For example, they are currently making recommendations for the Gender Recognition Draft Bill.
“But the reality is that policy and legal changes take a lot of time,” said RSAT Director, Tanachai Chaisalee.
While this longer-term work proceeds, a redress mechanism helps clients address current concerns. RSAT is tapped into the Crisis Response System (CRS) initiated by the Ministry of Public Health in collaboration with the Office of the Attorney General, Ministry of Justice. People with complaints about prejudice or rights violations in any sphere can scan a QR code and report their experience. Reports may also be sent via Facebook, email or LINE, Thailand’s answer to WhatsApp. A multi-disciplinary team conducts investigations and works with the client and other stakeholders to help.
The lion’s share of reports made via RSAT come from transwomen (78%) while gay men have lodged 17% of reports. The most common challenges relate to requirements for gender confirming attire, social exclusion (particularly during job application processes) and HIV status.
RSAT’s Human Rights Manger, Watcharawit Waraphattharanon, shares that they have been able to resolve some cases very quickly. For instance, if a person living with HIV is being forced to take an HIV test as a requirement for work, the Attorney General’s office does an emergency intervention.
“We can close these cases within one week,” he said.
“The work of key population-led, community-based organisations like RSAT is critical to reach those who most need HIV services,” UNAIDS Country Director, Patchara Benjarattanaporn stressed. “The Government’s progress in funding Community-led Health Services and building partnerships between these organisations and the public health system puts us on the path to end AIDS.”
A group of journalists visited the Ozone Foundation as part of the UNAIDS, UNDP, APN Plus and USAID/PEPFAR Southeast Asia Regional Workshop on HIV-related Stigma and Discrimination in Bangkok, Thailand on June 8, 2023. Learn more about this novel training
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025