Feature Story
Countries in eastern Europe and central Asia agree to expand access to a range of medicines
26 November 2018
26 November 2018 26 November 2018On 22 November, at a meeting held in Minsk, Belarus, countries from across eastern Europe and central Asia signed the Statement on Expanding Access to Affordable and Quality Assured Medicines and Diagnostic Technologies for HIV, Tuberculosis and Viral Hepatitis (Minsk 2).
In Minsk 2, countries in eastern Europe and central Asia commit to make urgent use of the best global practices and available tools to ensure the quality, safety and efficacy of health products and reduce the prices of essential HIV, tuberculosis and hepatitis C medicines and diagnostics in the region. The statement, among other things, envisages the revision of procurement mechanisms, the use of international and joint procurement and consultations and negotiations on price policy with medicine suppliers.
“In Minsk, the countries of eastern European and central Asia adopted a set of new, tangible, urgent actions. The countries will learn and share many lessons while implementing the Minsk 2 statement, which will help to lower prices, improve quality and save lives,” said Tim Martineau, UNAIDS Deputy Executive Director, Programme, a.i.
During the meeting, the Mayor of Minsk signed the Paris Declaration to end the AIDS epidemic in cities, becoming the fourth city in eastern Europe and central Asia to join the network of more than 300 cities and regions worldwide that are committed to Fast-Track their local HIV responses and to reach the 90–90–90 targets by 2020.
“The signing of the Paris Declaration by Minsk gives a boost to our capital’s goal to stop the spread of HIV by mobilizing officials, the workforce and public associations,” said Valery Malashko, Minister of Health, Belarus.
Belarus continues to make progress in its AIDS response. In 2016, Belarus was validated by the World Health Organization as having eliminated mother-to-child transmission of HIV and congenital syphilis. Belarus implements a full range of HIV policies and programmes with government support and funding, including harm reduction programmes for injecting drug users and antiretroviral therapy for people living with HIV. In 2017, Belarus rolled out HIV self-testing, selling self-testing kits in pharmacies.
“As civil society we believe that the simplest universal solution to ensure access to resources is to change political principles and priorities. People’s lives must be a priority,” said Dmitry Sherembey, from the All-Ukrainian Network of People Living with HIV.
Also during the meeting, eight international organizations signed an agreement to establish a regional interagency group to support the coordinated efforts and implementation of Minsk 2, focusing on results and impact at the country and regional levels.
“Closing the gap to cost-effective, equitable and sustainable access to quality medicines and diagnostic technologies requires further effective collaboration and political leadership in eastern European and central Asian,” said Zsuzsanna Jakab, Regional Director for Europe, World Health Organization.
Region/country
Related





Feature Story
Access to quality medicines and gender-based violence discussed in Ethiopia
22 November 2018
22 November 2018 22 November 2018In order to highlight the need for sustainable and affordable access to quality medicines, the Executive Director of UNAIDS, Michel Sidibé, spoke about the necessity of implementing the African Union Pharmaceutical Manufacturing Plan. Speaking at the opening ceremony of Africa Industrialization Week 2018 in Addis Ababa, Ethiopia, he called for close cooperation with regional economic communities in order to build production cooperation hubs and lead pharmaceutical regulatory harmonization in Africa.
Commitments on gender-based violence and the rights of women made at an event held on the margins of the United Nations General Assembly in September entitled Eliminating Sexual and Gender-Based Violence and Protecting the Health and Rights of Women and Children in Humanitarian Settings were discussed during meetings Mr Sidibé held with Smail Chergui, the Africa Union Commissioner for Peace and Security, and the African Union Special Envoy on Women, Peace and Security, Bineta Diop.
During the meetings, discussions were held on how to increase efforts in responding to HIV in conflict and humanitarian settings and the need to increase awareness on HIV testing and on sexual and gender-based violence. Mr Sidibé and Mr Chergui agreed to conduct a high-level joint mission to South Sudan to highlight the needs of people facing a higher risk of HIV in the country owing to gender-based violence and the protracted conflict.
Also during his visit to Ethiopia, which took place from 17 to 20 November, Mr Sidibe’s met with Ethiopia’s Prime Minister, Abiy Ahmed, who said, “I am committed to change the narrative of Africa and Ethiopia through ongoing reforms and agree to strengthen efforts on people-centred health development for Ethiopia.”
“Thank you for agreeing to champion ending AIDS in Ethiopia and across the continent,” said Mr Sidibé.
The President of Ethiopia’s agenda on gender and peace and the rehabilitation of street children was the topic of conversation in a meeting between the President, Sahle-Work Zewde, and Mr Sidibé.
During a discussion Mr Sidibé had with the Minister of Health of Ethiopia, Amir Aman, a collaborative project was developed that will be centred around strengthening resource mobilization, enhancing and sustaining a multisectoral response across all sectors, engaging young people and enhancing HIV programmes following the location–population approach.
Region/country
Related





Feature Story
Learning from city-level approaches to putting the HIV response on the Fast-Track
09 November 2018
09 November 2018 09 November 2018The Paris Declaration to end the AIDS epidemic in cities has gained political momentum among city leaders to commit to ending AIDS and to address disparities in access to health and social services. To date, about 300 cities and municipalities around the world have signed the declaration.
Sponsored by USAID through the United States President's Emergency Plan for AIDS Relief, a joint UNAIDS and International Association of Providers of AIDS Care Fast-Track cities project was designed to provide essential and strategic technical support to priority high-burden cities to accelerate the AIDS response and deliver on the commitment of the Paris Declaration. Ten cities, represented by local governments, civil society organizations and development and other partners, gathered in Johannesburg, South Africa, on 2 November to reflect on experiences and lessons learned during the first year of implementation of the project.
In all 10 cities, political leadership of the HIV response has been mobilized and city health departments are actively engaged in leading the response to HIV. In addition, the projects are receiving high-level support from local and national governments, as well as national AIDS councils. In Yaoundé, Cameroon, the project has provided an opportunity to convene partners on a regular basis, under the leadership of the seven city mayors, to improve coordination of activities, address potential overlap and review progress.
The project is contributing to innovation in cities. In Jakarta, Indonesia, concept testing of mobile solutions has identified an effective and relevant approach to reaching young people and a mobile application is being developed to reach young gay men and other men who have sex with men with key messages related to HIV testing, prevention and support.
“Cities present their own unique advantages to building a multisectoral approach to HIV and can benefit from social transformation opportunities associated with a strong AIDS response. Equity, inclusiveness, resilience and sustainability are not only key to a successful health-care strategy, they are also the building blocks to a thriving city,” said Catherine Sozi, Director of the UNAIDS Regional Support Team for Eastern and Southern Africa.
Civil society is actively engaged in the 10 cities. In Kinshasa, Democratic Republic of the Congo, civil society has been active in the implementation of the project, in advocacy meetings with political leaders, national authorities and other partners, on issues related to stigma, discrimination and human rights. The Kigali, Rwanda, team highlighted the support by the project to the strategic outreach activities to provide HIV services to key populations, including distribution of more than 10 000 condoms in three different locations.
“Through the condom kiosk project with the city government, we were able to successfully reach key populations in Kigali,” said Uwase Nadège, Programme Manager of the Kigali Hope Association. “People who access these services trust others from the community, and we see this as a way to meaningfully engage with the government to Fast-Track the response.”
In Durban and Johannesburg, South Africa, the project is receiving high-level political support from local as well as national governments. In Johannesburg, the project will support the establishment of a city AIDS council, with the key goal of coordinating the HIV response in the city.
Durban, Jakarta, Johannesburg, Kigali, Kinshasa, Lusaka, Maputo, Mozambique, Nairobi, Kenya, Windhoek, Namibia, and Yaoundé are the first 10 cities participating in the project.
Resources
Region/country


Feature Story
UNAIDS Programme Coordinating Board sees South Africa’s AIDS response first-hand
07 November 2018
07 November 2018 07 November 2018Ahead of its 43rd meeting in December, the UNAIDS Programme Coordinating Board (PCB) conducted a four-day visit to South Africa between 15 and 18 October. During the visit, the delegates met with a wide range of national and development partners working on the AIDS response and conducted a number of site visits in order to experience the support of the Joint Programme to the national AIDS response in a high-burden country.
South Africa has the largest HIV epidemic in the world, with 7.2 million people living with HIV. In the past 10 years, it has made significant progress in its AIDS response, with 4.4 million people living with HIV on treatment. The country also invests heavily, with approximately 75% of the response funded by the government—just over US$ 2 billion in 2017. However, new HIV infections are high, at 270 000 in 2017.
The PCB delegation, led by the UNAIDS Deputy Executive Director, Gunilla Carlsson, and Danny Graymore, from the United Kingdom of Great Britain and Northern Ireland, the Chair of the PCB, comprised seven representatives of Member States, one civil society representative and a number of participants from the Joint Programme.
“The strength of the UNAIDS Programme Coordinating Board is its unique multistakeholder representation, which includes civil society and United Nations cosponsoring organizations, in addition to Member States,” said Mr Graymore. “The United Kingdom has put a particular focus on prevention for 2019. Coming to South Africa, we wanted to see how to get better results on HIV prevention in the context of a conducive environment and a significant investment in the national response.”
During a meeting with the South African National AIDS Council’s (SANAC) civil society forum, Valeria Rachinska, a PCB delegate from civil society, encouraged members of civil society in South Africa to use their voice in the UNAIDS PCB through the two African region representatives.
“The UNAIDS Programme Coordinating Board is unique in that civil society are members and our voice is heard. We can influence the global agenda in this way. I encourage you to get in touch with your African representatives and make your voices heard,” she said in response to concerns about the financing and sustainability of civil society organizations in South Africa.
During the visit, PCB delegates met with other representatives of SANAC, national and local government, civil society and the private sector and visited community-based initiatives in the KwaZulu-Natal and Gauteng Provinces.
“I am delighted to visit South Africa with such a broad and knowledgeable Programme Coordinating Board delegation. It is clear that the support of the Joint Programme is appreciated and important. We need to focus more on HIV prevention and ensure that we reach people being left behind by the AIDS response and find ways to deliver effective prevention services for young women and adolescent girls,” said Ms Carlsson.
Region/country


Feature Story
Call for a broader vision for harm reduction
09 November 2018
09 November 2018 09 November 2018In 2016, more than 11 million people in the Unites States of America abused prescription opioids and nearly 1 million used heroin, according to the United States Government. Although millions of people in the country are addicted to opioids, only 1 in 10 get treatment.
In 2017, at least 64 000 people died from drug overdose in the Unites States. The misuse of, and addiction to, opioids—including prescription pain relievers, heroin and synthetic opioids such as fentanyl—is a serious national crisis that affects public health as well as social and economic welfare, with devastating consequences.
It is against this backdrop that the Harm Reduction Coalition—a national advocacy and capacity-building organization in the United States that works to promote the health and dignity of people and communities affected by drug use—convened its 12th National Harm Reduction Conference in New Orleans from 18 to 21 October.
At the conference, the Harm Reduction Coalition called for the creation of spaces for dialogue and action to heal the harms caused by racialized drug policies. It also announced that it will move beyond traditional core activities in training, capacity-building and policy.
The participants heard a call for a broader vision of harm reduction that extends beyond prevention and risk reduction to strategies to address trauma, social division, injustice and inequities.
“We cannot end AIDS if we do not end it among people who inject drugs. UNAIDS is committed to harm reduction. Harm reduction works. Harm reduction saves lives,” said Ninan Varughese, Senior Adviser, UNAIDS.
In the lead-up to the ministerial segment of the sixty-second session of the Commission on Narcotic Drugs, to be held in March 2019, the United Nations is discussing the issue of the world drug problem at the highest level. The United Nations Secretary-General will discuss the issue at his biannual meetings with the heads of United Nations entities and hopes to adopt a common position that will underscore the strong commitment of the United Nations to strengthen the implementation of the outcome document of the 2016 United Nations Special Session on the World Drug Problem through interagency collaboration.
Region/country
Related

Feature Story
Ecuador innovates around HIV prevention in its cities
07 November 2018
07 November 2018 07 November 2018Surrounded by the stately centuries-old buildings of Quito’s Old City, a group of men are playing a modified game of Jenga. Each wooden brick they carefully extract from a tower corresponds to a sexual health lesson. There’s rapt attention while the peer educator demonstrates how a female condom is used. One table over, young people are gathered around for a male condom demonstration. People might stop by the tents for blood pressure or blood sugar tests, but they stay for the lively safer sex education.
This hands-on engagement is a result of collaboration between the Directors of Health and Social Inclusion for the Municipality of Quito and civil society organizations, including the Kimirina Corporation. Two years after becoming the first Andean city to sign the Paris Declaration to end the AIDS epidemic in cities, Quito has dramatically scaled up HIV testing and prevention programmes. Four hundred kilometres away, the city of Guayaquil is following suit, expanding HIV prevention and community testing.
Over the past year there has been a renewed emphasis on community testing, with concrete results. The proportion of newly diagnosed people being linked to health services has increased by a quarter in Quito and a third in Guayaquil.
“You are not just talking about the epidemic, but also using practical approaches,” UNAIDS Executive Director Michel Sidibé said during a visit to Ecuador on 30 October. “We are seeing people being educated, accessing services and getting tested. Anything we do with the support of the community is sustainable.”
This emphasis on community involvement is a key feature of the new Ecuador Multisectoral National Strategic Plan on HIV. During the plan’s symbolic launch on 30 October, Ecuador’s Public Health Minister, Veronica Espinosa, emphasized that the missions to end AIDS and to build a better society were one and the same.
“We are working to ensure a life without prejudice and the right to health for all without discrimination,” said Ms Espinsosa.
And the human rights-based approach to HIV services does not end with citizens of Ecuador. Ecuador has shown great leadership with regard to migrants, including guaranteeing health care for refugees and migrants living with HIV.
“You have opened your hands and heart to people coming from other places,” said Mr Sidibé. “By giving treatment access to people who could be left behind you are demonstrating that you set a high standard, not only for yourselves but for the world.”
Region/country




Feature Story
New commitment to primary health care
01 November 2018
01 November 2018 01 November 2018Countries reaffirmed the fundamental right of every human being to the enjoyment of the highest attainable standard of health and committed to strengthen primary health-care services at the Global Conference on Primary Health Care. The Declaration of Astana, unanimously endorsed at the conference by all World Health Organization Member States, makes pledges in four key areas: making bold political choices for health across all sectors; building sustainable primary health care; empowering individuals and communities; and aligning stakeholder support to national policies, strategies and plans.
HIV disproportionately affects populations that are in many countries marginalized, stigmatized, discriminated against and criminalized. The new commitment to primary health care presents a timely and unique opportunity to step up efforts to address the many barriers that those populations face in accessing HIV and primary health-care services. Addressing such barriers requires having the courage to respond to issues that are often considered sensitive or taboo—around gender, sexuality, identity, exclusion and power.
“UNAIDS is proud to be leading on community and civil society engagement, as part of our contribution to the Global Action Plan for Healthy Lives and Well-Being for All. Only by taking AIDS out of isolation can we can save lives holistically, not disease by disease, issue by issue,” said Vinay P. Saldanha, Director of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
UNAIDS’ contribution to the event, The AIDS response and primary health care: linkages and opportunities, sets out examples of how to integrate HIV services into primary health care and, conversely, how to use the AIDS response to further leverage primary health care. It calls for urgent attention to be given to the structural and root causes of ill health and for sexual and reproductive health and rights to be central to primary health care.
The Global Conference on Primary Health Care took place in Astana, Kazakhstan, on 25 and 26 October.
Read the declaration
Region/country
Related

Feature Story
Civil society cooperation network for the Americas and the Caribbean launched
02 November 2018
02 November 2018 02 November 2018A new regional civil society cooperation network for the Americas and the Caribbean to support nongovernmental organizations working to end AIDS was launched on 30 October in Quito, Ecuador. Launched by Coalition PLUS, the initiative will support coordination and capacity-building among community organizations involved in the AIDS responses of North, Central and South America and the Caribbean.
“Although we have HIV services available, people do not have access because they are criminalized and stigmatized. The community movement is helping us to end the conspiracy of silence about discrimination. We need civil society to increase efforts to achieve the progressive policies that will clear the way for us to end AIDS,” said Michel Sidibé, UNAIDS Executive Director.
Since 2014, Coalition PLUS—an international alliance of more than 100 nongovernmental organizations contributing to the AIDS response—has been building and strengthening mechanisms for regional collaboration. Such networks already exist in western Africa, central Africa, the Middle East and North Africa, the Indian Ocean and Europe.
The President of Coalition PLUS, Hakima Himmich, said that the network will increase access by organizations to new resources and approaches relevant to their local contexts. She noted that it was especially important to strengthen civil society’s capacity around addressing the needs of the most vulnerable.
“We have huge challenges around stigma and discrimination against entire populations. In order to achieve epidemic control, we must also address human rights,” said Ms Himmich.
UNAIDS data show that in 2017 key populations and their sexual partners accounted for three quarters of new HIV infections in Latin America and two thirds of new infections in the Caribbean. Gay men and other men who have sex with men and transgender women are disproportionately affected, with a few countries reporting HIV rates of above 15% among those communities.
The activities of the network in the region will be coordinated by the Kimirina Corporation, a Ecuadorian organization focused on people-centred combination prevention and advocacy. Amira Herdoiza, Director of the Kimirina Corporation, explained that the platform will place strong emphasis on coordinated research, skills-building and advocacy, particularly around issues affecting young people and key populations.
“We need more multicountry research to show the nuances of our epidemics,” Ms Herdoiza said. “Through this network our organizations’ capacities to share and analyse data will be strengthened. We will also focus on sharing experiences and planning joint programmes.”
At present, there are three other members of the regional network: the Coalition of Quebec Community Organizations against AIDS in Canada; AIDES in the French Caribbean; and the Institute for Human Development in the Plurinational State of Bolivia. Other regional organizations are invited to be part of the initiative.
Region/country
Related


Feature Story
New data dashboard launched in the Asia and the Pacific region
02 November 2018
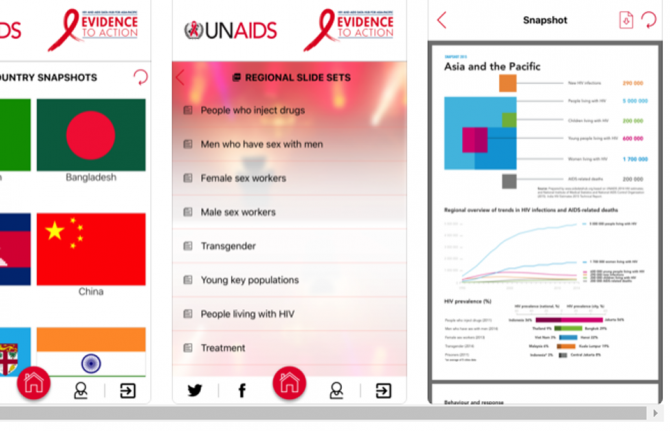
02 November 2018 02 November 2018A new data dashboard to enhance the HIV strategic information products that were already available on the AIDS Data Hub for the Asia and the Pacific region was launched on 30 October.
Developed by UNAIDS, the platform allows users to visualize data and indicators related to HIV epidemiology and the AIDS response in the region through customizable maps, graphs, tables and fact sheets by indicator, country and key population. It also facilitates integrated analysis and gives access to granular data. The data dashboard is a one-stop shop that offers HIV-related strategic information, data analysis products and reference documents.
“With concrete targets to be met on the way to end the AIDS epidemic by 2030, it is vital to have the right data tracking whether the Asia and the Pacific region is on course to meet the commitments made in the 2016 United Nations Political Declaration on Ending AIDS. Data show us how far we have come and how far we have to go,” said Eamonn Murphy, Director of the UNAIDS Regional Support Team for Asia and the Pacific.
Accurate and credible data on the HIV epidemic are the cornerstone of the AIDS response. Over the years, a detailed understanding of the HIV epidemic has been built up through the collection, analysis and dissemination of data, helping programmes to reach the right people in the right place and at the right time. Having high-quality data on the AIDS response coupled with cutting-edge analysis has been critical for countries to track their progress towards ending the AIDS epidemic.
UNAIDS and the Data Hub team work with all the countries in the region to collect and analyse data on their AIDS responses and to help build their capacity to generate and use strategic information. In the region, no major report, speech or policy initiative on HIV is launched or made without referring to data collected and released by UNAIDS.
The Data Hub team works closely with civil society, particularly on strengthening the capacity of young community members on data literacy and the interpretation and use of data. “Research and data, coupled with the lived experience of our community, provide the evidence we need for an effective response to HIV. The AIDS Data Hub is an essential tool for helping community-based HIV workers across the Asia–Pacific region access relevant research and data to amplify their advocacy for better services, more funding and the scaling up of programming,” said Midnight Poonkasetwattana, the Executive Director of APCOM.
Asia Pacific AIDS Data Hub
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
HIVR4P 2018 highlights new possibilities for HIV prevention
31 October 2018
31 October 2018 31 October 2018The possibilities for new and improved HIV prevention options were showcased at the recent HIV Research for Prevention (HIVR4P) conference, although the participants heard that many new tools are still several years from being ready for implementation.
The importance of pre-exposure prophylaxis (PrEP), including PrEP delivered by a vaginal ring and long-acting PrEP, including injectable PrEP, was featured in many presentations. Vaginal ring PrEP offers better female-controlled prevention options that can protect women without their partner’s knowledge, while injectable PrEP would mean that daily pill-taking and the risk of forgetting to take the pill would be history. Both vaginal ring PrEP and long-acting PrEP are still some way from being available, however, with the vaginal ring currently being reviewed for regulatory approval by the European Medicines Agency and trials for long-acting PrEP not due to deliver results until 2021 or later.
If antibodies and engineered molecules that mimic them can be shown to prevent HIV infection, the way to six-monthly injections for either prevention or treatment could be opened up, along with the possibility of a vaccine that made people develop their own similar antibodies. The participants heard that much progress had been made in discovering and developing such antibodies. The first proof of principle trials showing their effectiveness will report their results in 2020.
“Science has delivered us extraordinary advances in technologies for the diagnosis, treatment and monitoring of HIV infection. There is now real excitement that over the next years it will also lead to effective affordable prevention tools,” said Peter Godfrey-Faussett, Science Adviser, UNAIDS.
The participants heard that there are high levels of sexually transmitted infections (STIs) among the populations at higher risk of HIV and that, as we have known for decades, STIs lead to increased HIV acquisition. The rates of the major treatable bacterial STIs have been rising steadily and are at alarming levels among gay men and other men who have sex with men and young people in eastern and southern Africa, in part due to declining condom usage. The high rates of the major treatable STIs have become particularly evident with the advent of increased screening accompanying the roll-out of PrEP.
Many STIs have no symptoms and can only be diagnosed with modern diagnostic tests—these are simple, but still far too expensive for the countries that need them the most. Along with geography and age group, STIs are among the strongest indicator of risk of HIV. An integrated STI and HIV prevention approach could offer PrEP to people who are HIV-negative but have an STI and live in an area where HIV is prevalent.
New prevention technologies are likely to be relatively expensive and hence will need to be focused on populations at higher risk in order to be affordable and cost-effective. Mathematical modelling shows that these new HIV prevention technologies may have only a limited impact on new HIV infections in eastern and southern Africa. For example, modelling of the impact of the dapivirine ring—a vaginal ring with a slow release of an antiretroviral medicine that protects against HIV infection—shows that only 1.5–2.5% of HIV infections would be averted over the next 18 years in Kenya, Uganda, Zimbabwe and South Africa. With the cost of averting one HIV infection through the use of the dapivirine ring varying from US$ 10 000 to US$ 100 000, many of the participants argued for integrating and combining both HIV treatment and prevention, and the responses to HIV and other diseases, for maximum effect.
The biennial HIVR4P conference was held in Madrid, Spain, from 21 to 25 October.