Press Statement
UNAIDS welcomes landmark agreement between Medicines Patent Pool and Merck Sharp and Dohme
28 October 2021 28 October 2021GENEVA, 28 October 2021—UNAIDS welcomes the agreement between the Medicines Patent Pool (MPP) and the pharmaceutical company Merck Sharp & Dohme through which the intellectual property rights over an antiviral medicine to treat mild to moderate forms of COVID-19 in adult patients are shared with interested sub-licensees on a non-exclusive and transparent basis. The new medicine, molnupiravir, is still pending regulatory approval but has obtained optimal results in clinical trials.
“This agreement is a good first step, where public health has been prioritized over profits,” said the Executive Director of UNAIDS, Winnie Byanyima. “This new treatment promises to be a valuable addition in the response to COVID-19 and access to it will be considerably widened by allowing companies from around the world to produce more affordable versions of the medicine.”
This is the first licensing agreement on a COVID-19 tool to be established within a public health perspective. It is a significant development considering the lack of medicines to treat COVID-19. The initiative will allow the entry into market of more affordable generic versions of this medicine as soon as it is granted authorization from national and/or regional health regulatory bodies or included in the World Health Organization (WHO) list for emergency use.
According to the agreement, pharmaceutical companies based anywhere in the world that are interested and qualified to manufacture generic versions of the product will be allowed to commercialize the medicine in the 105 countries included in the geographic scope of the licensing agreement. Nevertheless, recognizing that COVID-19 knows no geographic boundaries, UNAIDS expects that all countries suffering the disease burden will have access to the generic market for this product. All health technologies should be considered global public goods.
This agreement includes all sub-Saharan countries, all low-income countries, the majority of lower-middle-income countries and 20 upper-middle-income countries.
Originally established to negotiate public health-oriented licensing agreements for HIV, tuberculosis and malaria products, the MPP has been an important player in the HIV response by promoting competition within the pharmaceutical market and helping to push down the prices of essential medicines. UNAIDS and MPP are both members of the steering committee of the WHO COVID-19 Technology Access Pool (C-TAP), an initiative that calls for the voluntary sharing of technologies, knowledge, data and intellectual property rights of health products to prevent, diagnose and treat COVID-19.
“It is high time that similar arrangements are also made for making COVID-19 vaccines. What works for medicines should also work for vaccines and diagnostics and other life-saving technologies,” said Ms Byanyima. “I call on the Group of Twenty and other governments to ensure that patent holders are obliged to share life-saving tools and technologies equitably.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work


Feature Story
A Dose of Reality: How rich countries and pharmaceutical corporations are breaking their vaccine promises
21 October 2021
21 October 2021 21 October 2021Developing countries have been hit with an endless tide of inadequate gestures and broken promises from rich countries and pharmaceutical companies, who are failing to deliver billions of doses they promised while blocking the real solutions to vaccine inequality, according to a new report published today by the People’s Vaccine Alliance.
The report, “A Dose of Reality,” found that of the 1.8 billion COVID vaccine donations promised by rich nations only 261 million doses – 14 per cent – have been delivered to date, while western pharmaceutical companies have delivered only 12 per cent of the doses they allocated to COVAX, the initiative designed to help low- and middle-income countries get fair access to COVID vaccines.
At the same time, the EU and other rich nations have refused to support the proposal of over 100 nations to waive patents on vaccines and COVID related technologies while leading pharmaceutical companies have failed to openly share their technology with the World Health Organisation to enable developing countries to make their own vaccines and save lives.
Winnie Byanyima, Executive Director of UNAIDS, said: “Rich nations and corporations are shamefully failing to deliver on their promises whilst blocking the actual solution; ensuring developing nations have the ability to make their own vaccines.
“It is painfully clear that the developing world cannot rely on the largesse and charity of rich nations and pharmaceutical companies, and hundreds of thousands of people are dying from COVID-19 as a result. This is beyond appalling.”
The UK Government, which has been actively blocking calls from countries like South Africa and India to be allowed to make their own vaccines, has only delivered 9.6 million – less than 10 per cent - of the 100 million doses it promised to poorer nations. Meanwhile it has itself taken half a million doses from COVAX, despite extreme vaccine shortages in developing countries and having already secured more than enough doses for British people from direct deals with the pharmaceutical companies. Canada has taken over 970,000 doses from COVAX, while delivering only 3.2 million – or 8 per cent – of the 40 million doses it promised. Germany, another country blocking the waiver, has delivered 12 per cent of the 100 million doses it promised and France has delivered just 9 per cent of the 120 million it promised. The US has delivered the most doses - nearly 177 million doses – however this is just 16 per cent of the 1.1 billion promised.
The Alliance said that while COVAX failed to acknowledge that relying on pharmaceutical companies may not deliver doses, the companies have undermined the initiative, first by not allocating it enough doses and second by delivering far less than they agreed. Of the 994 million doses allocated to COVAX by Johnson & Johnson, Moderna, Oxford/AstraZeneca, and Pfizer/BioNTech, only 120 million -12 per cent- have actually been delivered, which is fifteen times less than the 1.8 billion doses delivered to rich countries from these companies. Both Johnson & Johnson and Moderna are yet to deliver a single dose they promised to the initiative.
Oxfam’s Robbie Silverman said: “The failure of rich country donations and the failure of COVAX have the same root cause – we have given over control of vaccine supply to a small number of pharmaceutical companies, who are prioritising their own profits.
“These companies can’t produce enough to vaccinate the world, they are artificially constraining the supply, and they will always put their rich customers at the front of the line.
“The only way to end the pandemic is to share the technology, and know-how with other qualified manufacturers so that everyone, everywhere can have access to these lifesaving vaccines.”
During the UN General Assembly in September, President Biden rallied support for the goal to vaccinate 70 per cent of people in every country by September of 2022. While this target is rightly ambitious, the People’s Vaccine Alliance says it should be achieved much more quickly, and there is still no plan to achieve it.
The WHO stated that it must be a global priority to get doses to developing countries by the end of this year, but the Alliance says rich countries are not listening and working to a timetable of delivering an inadequate supply of doses by some time in 2022, which is likely to lead to countless unnecessary deaths.
Maaza Seyoum, of the African Alliance and People’s Vaccine Alliance Africa, said: “Across the world health workers are dying and children are losing parents and grandparents. With ninety-nine per cent of people in low-income countries still not vaccinated, we have had enough of these too little too late gestures.
“Governments must stop allowing pharmaceutical companies to play god while raking in astronomical profits and start delivering actual action that will save lives.”
To deflect growing pressure to share their vaccine technology free of intellectual property restrictions leading western pharmaceutical corporations have consistently over-exaggerated their projected production volumes, claiming there will soon be enough for everyone while delivering the overwhelming majority of their stock to rich nations. Collectively, the four companies claimed they would manufacture an estimated 7.5 billion vaccines in 2021, yet with less than three months until the end of the year, they have only delivered half of these. Forecasts suggest the companies will produce 6.2 billion vaccines by the end of the year, a shortfall on their projections of more than 1.3 billion doses.
With a week to go before leaders meet for the G20 summit in Rome, The People’s Vaccine Alliance - which has 77 members including ActionAid, the African Alliance, Global Justice Now, Oxfam and UNAIDS – is calling on them to stop breaking their promises to vaccinate the world and to:
- Suspend intellectual property rights for COVID vaccines, tests, treatments, and other medical tools by agreeing to the proposed waiver of the TRIPS Agreement at the World Trade Organisation.
- Demand, and use all their legal and policy tools to require pharmaceutical companies to share COVID-19 data, know-how, and technology with the WHO’s COVID-19 Technology Access Pool and South Africa mRNA Technology Transfer Hub.
- Invest in decentralised manufacturing hubs in developing countries to move from a world of vaccine monopolies and scarcity to one of vaccine sufficiency and fairness in which developing countries have direct control over production capacity to meet their needs.
- Immediately redistribute existing vaccines equitably across all nations to achieve the WHO target of vaccinating 40 per cent of people in all countries by the end of 2021 and 70 per cent of people in all countries by mid-2022.
Related




Feature Story
Getting unconditional cash to marginalized households during COVID-19
29 October 2021
29 October 2021 29 October 2021COVID-19 has underscored the crucial need for pandemic responses to include social protection measures that reach and benefit marginalized populations.
As the pandemic swept across western and central Africa in early 2020, the region was already grappling with socioeconomic distress and humanitarian crises. Social restrictions imposed to contain the pandemic exacerbated those challenges. Impoverished and vulnerable populations, including people living with HIV and key populations, were hit hard.
Surveys conducted between June and August 2020 in 17 countries in the region on the situation and needs of people living with HIV—with support from UNAIDS, in partnership with the Network of African People Living with HIV West Africa—revealed that up to 80% of people living with HIV were experiencing livelihood losses, and more than 50% of them needed financial and/or food assistance.
These findings convinced UNAIDS and the World Food Programme (WFP) to launch a pilot project on unrestricted cash transfers in July 2020 to help people living with HIV and key populations cope with the socioeconomic impact of HIV and COVID-19 in four priority countries: Burkina Faso, Cameroon, Côte d’Ivoire and Niger. The initiative was designed to capitalize on WFP’s existing arrangements with service providers and on UNAIDS’ community engagement and relationships with civil society networks in the four priority countries.
Cash transfers are increasingly recognized as an effective form of social protection, with positive social and economic effects. They provide income support and help households avoid selling off assets or removing children from school, and they have multiplier effects on local economies. They constituted approximately 40% of global social safety net expenditures in 2018, but less than 20% in western and central Africa.
As the pandemic spread across western and central Africa, only a few countries (Côte d’Ivoire and Senegal among them) allocated additional support for vulnerable households in the form of cash transfers or social grants.
The immediate objective of the pilot was to reach about 5000 households with one-off, unconditional cash transfers, which ranged from US$ 88 per beneficiary (in Côte d’Ivoire) to US$ 136 (in Cameroon).
“I am so grateful for this support. I used it to pay the fees for my sewing course and to buy a sewing machine to start my own business. I also helped my mother who lost her job due to the pandemic,” said a young woman living with HIV in Cameroon.
Civil society organizations and financial service providers were engaged during the planning of the pilot. Eligibility for the transfers was decided based on a variety of vulnerability criteria, and beneficiaries were identified with the support of community-led organizations. Additional steps involved sensitizing beneficiaries, distributing the cash transfers, troubleshooting and monitoring the process. Specific attention was made to ensure confidentiality and to mitigate any potential stigma for beneficiaries.
Across the four countries, almost 4000 beneficiaries were reached, and it is estimated that a further 19 000 household members also benefited from the cash transfers, most of which went towards food, health care, education and housing expenses, or for income-generating activities. Country experiences varied in terms of the depth of their collaboration with community partners and the extent to which government actors were involved.
The experience of the pilot demonstrated that delivering rapid cash transfers to marginalized people living with HIV and key populations in very difficult circumstances is possible, and that it provides valuable emergency support.
Critical lessons learned include the need for inclusive and flexible approaches, working in ways that are clear and transparent to community partners and systematically involving community partners throughout the process. Defining clear and unbiased eligibility criteria, applying them consistently and sensitizing beneficiaries and communities are also vital.
Capacity-building and other support (including funding) for community partners is another critical element. Community-level organizations, trusted counsellors and peer educators were essential for establishing trust, identifying and reaching the intended beneficiaries, minimizing stigma and assessing the impact of the cash transfers. Engaging with government structures from the beginning helps to create the potential for long-lasting improvements.
One-off cash transfers of this kind can help households withstand short-term shocks, but they do not do away with the need to fully integrate vulnerable and marginalized populations into crisis responses and comprehensive social protection systems. It is imperative that countries across Africa expand inclusive, multipurpose social protection that is accessible and sustainable. Enhancing the people-centredness of cash transfers and slotting them in with other forms of social provisioning and support that are not necessarily cash-based—such as free or subsidized primary health care, education, water and energy—is part of this process.
Following this pilot experience on the use of cash transfers to support the most vulnerable people living with HIV and key populations, UNAIDS and the Civil Society Institute for Health have further strengthened their collaboration on advancing HIV-sensitive and inclusive social protection in western and central Africa. Recently they organized, with the support of LUXDEV funding and in collaboration with several UNAIDS Cosponsors, a capacity-building workshop to mobilize and build the capacity of civil society and communities and to promote dialogue and collaboration among civil society organizations, partners and governments to advance inclusive, HIV-sensitive social protection in the region.
Building on the recommendations of the workshop, a number of follow-up activities were agreed to enhance the role and positioning of communities in advancing HIV-sensitive social protection within their countries and the region.
“The cash transfer initiative in Niger came at the right time. The cash transfers were used by the beneficiaries to stockpile food and pay rent, but most importantly to allow the children to continue their schooling. This initiative demonstrated the value and importance of working together with the communities and our Cosponsors to achieve a common goal,” said El Hadj Fah, the UNAIDS Country Director for Niger.
Video
Related


Feature Story
ASEAN cities protecting the gains of the HIV response during the COVID-19 pandemic
26 October 2021
26 October 2021 26 October 2021Fast-Track cities in South-East Asia have been stepping up efforts during the COVID-19 pandemic to ensure that HIV treatment and prevention services remain unaffected by the pandemic and to protect the gains made in the HIV response. The dynamic city-based infrastructures that have been built up around the HIV response are being leveraged to implement innovative programmes to safeguard people living with HIV and other vulnerable populations and contain the spread of COVID-19.
Jakarta, Indonesia, provides a clear example of how cities are accelerating their HIV responses, enabling continued progress while taking into account the effects of the COVID-19 pandemic. Since the first COVID-19 outbreak, Central Jakarta, with more than 10 000 people living with HIV on antiretroviral therapy, ensured treatment continuity with the implementation of multimonth antiretroviral therapy dispensing and community-led home-based delivery. In collaboration with partners, the Provincial Health Office of Jakarta developed the Jak-Anter service, which connects people living with HIV with health facilities across the metropolitan area, allowing for direct client-organized antiretroviral therapy delivery, benefiting nearly 30% of people living with HIV in the area.
This best practice was shared at an event, ASEAN Cities Getting to Zero: Protecting Fast-Track Cities’ Gains during the COVID-19 Pandemic, which brought together five cities from the Association of Southeast Asian Nations (ASEAN) on the margins of the Fast-Track cities 2021 hybrid conference in Lisbon, Portugal, on 21 October.
“Cities play a critical role in delivering on the United Nations Political Declaration on AIDS. As we make our collective steps towards the next phase of achieving the three zeroes, we must work in partnership to address the variety and complexity of HIV epidemics. Evidence-informed national regulations will ensure effective collaboration between national and subnational governments,” said Budi Gunadi Sadikin, the Minister of Health of Indonesia.
The event allowed ASEAN cities to share innovative practices in implementing HIV programmes amid the COVID-19 pandemic.
“ASEAN is committed to fast-tracking the HIV response to end AIDS by 2030. We must continue to work hand in hand and to ensure equitable access to HIV services and solutions, break down barriers and improve resource mobilization for efficient and sustainable HIV responses,” said Dato Lim Jock Hoi, the Secretary-General of ASEAN.
A recurring theme during the session was how quickly ASEAN cities utilized virtual platforms to scale up access to HIV services, especially during lockdowns. In the Philippines, Pasig City delivered quality services to key populations by increasing investments in HIV programmes and treatment facilities and the use of virtual platforms. Like Jakarta, Pasig City partnered with community-based organizations to deliver antiretroviral therapy, condoms and lubricants by establishing a service delivery network with service providers and health facilities to provide core packages of health-care services during the COVID-19 pandemic.
Can Tho, a city in Viet Nam, piloted a project to deliver self-test kits to key populations, in particular gay men and other men who have sex with men and people who use drugs, through virtual platforms. In collaboration with the World Health Organization and civil society partners, Can Tho quickly responded to COVID-19 by training community outreach workers to conduct community-based HIV rapid testing and by scaling up HIV self-testing.
Bangkok’s innovations included same-day delivery of antiretroviral therapy and the scale-up of key population-led health services. Bangkok, a regional leader in pre-exposure prophylaxis (PrEP) and a provider of specialized and holistic services for transgender people, expanded its PrEP services to 16 municipal public health centres and eight city hospitals during the COVID-19 pandemic.
Young people were noted as being at the forefront of the HIV response in ASEAN cities. In an effort to reduce the number of new HIV infections among young people in Langkawi, Malaysia, the Kedah State Health Department established the GLITZ project. The programme focuses on young people, including young key populations, through various outreach activities, mentor–mentee programmes and school and university visits to educate young people on HIV prevention.
As the Fast-Track cities network continues to grow in the ASEAN region, the complexity of HIV in urban areas is better understood. The network offers a way for cities to share best practices and experiences at a time of increasing urbanization and globalization.
“It has been 10 years since the ASEAN Cities Getting to Zero project was initiated. Since then, the project has successfully expanded to 76 cities in the region. As we see more participating cities and significant signs of progress in the HIV response, I encourage avenues for South–South collaboration. Together, in partnership, we can end AIDS as a global health threat by 2030,” said Taoufik Bakkali, the Director, a.i., of the UNAIDS Regional Support Team for Asia and the Pacific.
Our work
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa




Feature Story
Community mobilization and digital technologies accelerate the response to HIV and COVID-19 in Gabon
13 October 2021
13 October 2021 13 October 2021Gabon is one of the partnering countries involved in the Partnerships to Accelerate COVID-19 Testing (PACT) initiative in Africa. The project, developed under a partnership between UNAIDS and the Africa Centres for Disease Control and Prevention, aims at fostering collective action to respond to the colliding HIV and COVID-19 pandemics through strengthened community engagement, including the deployment of community health workers.
The UNAIDS Country Office for Gabon, in collaboration with other stakeholders, has chosen, as a starting point, to involve community actors to support the most vulnerable populations, in particular people living with HIV and the lesbian, gay, bisexual, transgender and intersex (LGBTI) community, in the context of COVID-19.
To increase coordination, ensure successful implementation and minimize the risks, all the stakeholders were involved from the design phase of the project. From the government, the Ministry of Health and the national steering committee of the pandemic response plan were involved at the highest level and appointed representatives to follow the development process and launch the project. In addition to a cabinet minister, representatives of Ministry of Health specialized national programmes joined the project, along with representatives of civil society and development partners.
The project will support the deployment of more than 70 people to accelerate the response to COVID-19 among vulnerable populations and to mitigate the impact of COVID-19 on the HIV response and services for other diseases, sexual and reproductive health and gender-based violence. In particular, it will contribute to supporting the continuity of services through increased community engagement. The project will cover four regions of Gabon, Libreville, Lambaréné, Port-Gentil and Franceville, that are severely impacted by COVID-19 and that have the highest HIV prevalence in the country.
Before the official launch of the project, UNAIDS signed an agreement with the Gabonese Red Cross, which in turn signed agreements with the selected community health workers, members of six associations and networks involved in the response to HIV and gender-based violence and that work with the LGBTI community and on sexual and reproductive health.
“The partnership with the Africa Centres for Disease Control and Prevention and support through UNAIDS has given a glimmer of hope to communities in Gabon that are often left to fend for themselves. It has shown that with even a little support, communities can innovate and make a difference. The involvement of communities should always be at the heart of the response to pandemics. We hope that this support can be sustained over time as the needs are still tremendous,” said the UNAIDS Country Director for Gabon, Françoise Ndayishimiye.
The project also has an innovative component in the monitoring of community actors. A mobile digital app was developed to support the community health workers with real-time data collection for monitoring and reporting on their activities. The app will ease reporting by allowing them to provide regular weekly reports on awareness and to support activities for people living with HIV and people living with tuberculosis, including on sexual and reproductive health, prevention of early pregnancies, HIV, gender-based violence, COVID-19 and discrimination.
Region/country
Related


Feature Story
Partnering to strengthen community engagement in the HIV and COVID-19 responses in Namibia
12 October 2021
12 October 2021 12 October 2021In the response to the colliding COVID-19 and HIV pandemics, communities continue to demonstrate resilience, agility and innovation. To empower, train and protect communities, UNAIDS, in collaboration with the Namibian Ministry of Health and Social Services and the Africa Centres for Disease Control and Prevention, is supporting civil society organizations to implement the Partnership to Accelerate COVID-19 Testing (PACT) initiative in Namibia. In addition, community sensitization activities to reduce the spread of COVID-19, and the associated stigma and discrimination, and to minimize its effects on people living with HIV, are being implemented.
In May 2021, Namibia experienced an exponential increase in community transmission of COVID-19 cases owing to the emergence of the delta variant, which derailed the country’s containment efforts and severely stretched its health system. The nation rose to the challenge with strong political leadership and commitment. Evidence-informed and high-impact interventions led to a marked decline in cases, positivity rates and deaths.
Through the PACT initiative, four civil society organizations with experience in working with vulnerable communities and networks of people living with HIV in informal settlements were supported by the Ministry of Health and Social Services and UNAIDS to implement the PACT project. The project focuses on COVID-19 prevention and contact tracing, mitigating the impact of COVID-19 on the HIV response and facilitating access to quality health care in all 14 regions of the country and will ultimately deploy 270 community health workers.
UNAIDS is partnering with three of the four civil society organizations, working in the three regions with the highest burden of HIV and COVID-19, Oshana, Erongo and Khomas, which account for 36% of people living with HIV, 52% of COVID-19 cases and 42% of COVID-19-related deaths nationally. These civil society organizations have done remarkable work to address the needs of key populations, adolescent girls and young women, and people living with HIV using existing HIV infrastructure and systems.
“Ending the two pandemics requires greater data-driven involvement of communities, partnerships, integration of COVID-19 and HIV services and reaching underserved and vulnerable communities. This is the approach that the PACT initiative has taken in Namibia to mitigate the spread of COVID-19,” said Alti Zwandor, UNAIDS Country Director for Namibia.
To adapt, harmonize and sustain the training of community health workers, UNAIDS has been working with the National Health Training Centre, which has adapted the Africa Centres for Disease Control and Prevention training curriculum on COVID-19 to include information on vaccines, HIV and sexual and reproductive health and rights. Forty senior trainers from the training centre were trained to deliver multiple trainings across the country. A further 250 community health workers and 25 supervisors were subsequently trained and deployed to implement community outreach activities. In addition to the house visits and community sensitization activities, one of the nongovernmental organizations, the Tonata people living with HIV network, has incorporated bulk text messages with COVID-19 information in local languages to support groups for people living with HIV, thus spreading awareness of the PACT initiative to a much larger audience.
“The community health-care workers in the field experienced situations where community members were aggressive when given information on COVID-19. In some hotspots, the population also complained of hunger and indicated that they would only engage with community health-care workers once provided with some food hampers so they could concentrate,” said Agatha Kuthedze, Director of the Namibia Planned Parenthood Association (NAPPA). She added that the organization had referred people in need of social welfare to the authorities for further help.
The initiative will continue to build on the successes and integrate critical HIV and sexual and reproductive health and rights programming while continuously exploring innovations for a sustained and comprehensive HIV response. The partner nongovernmental organizations involved are Tonata, the Walvis Bay Corridor Group, NAPPA and Project Hope.
Region/country
Related

Update
People living with HIV at higher risk of COVID-19 illness but have lower access to COVID-19 vaccines
11 October 2021
11 October 2021 11 October 2021An increasing body of evidence indicates that people living with HIV who acquire SARS-CoV-2 infection are at heightened risk of requiring hospitalization and having poor clinical outcomes.
Data from the United States of America show that people living with HIV who acquired SARS-CoV-2 infection were much more likely to require hospitalization and suffer severe illness than people who were HIV-negative, while studies from England and South Africa have found that the risk of dying from COVID-19 among people with HIV was double that of the general population. Advanced HIV disease and/or the presence of chronic comorbidities—which tend to be common in people living with HIV—appear to be strongly associated with poor COVID-19 outcomes in people living with HIV.
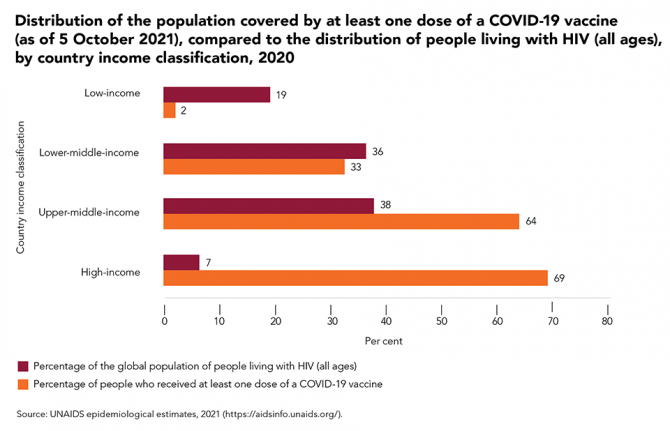
However, access to COVID-19 vaccines around the world remains exceedingly unequal and unjust. At the beginning of October 2021, there were still low levels of access to vaccines in the low-income and lower-middle-income countries that are home to more than half (55%) of people living with HIV globally.
Our work
Documents
Policy options to mitigate a drop in fiscal space for health and HIV following the COVID-19 pandemic — Case studies from the Democratic Republic of the Congo, Jamaica and Lesotho, November 2020
06 October 2021
To assess the impact of the COVID-19 pandemic on health and HIV expenditure, UNAIDS
carried out a modelling study on fiscal space for health and HIV. From a sample of
28 countries, three countries—the Democratic Republic of the Congo, Jamaica, and
Lesotho—were selected to capture health and HIV expenditure impacts across countries
with especially marked differences in burdens of disease (including HIV prevalence), HIV
donor dependency, level of economic development, and geographic location. While the
three-country sample is too small to permit findings to be generalized to other countries,
these analyses are useful for informing UNAIDS’ work to identify some policy positions to
minimize the COVID-19 pandemic’s impact on the HIV response.