Asia Pacific




Feature Story
Thailand partners develop community-led HIV care curriculum
23 February 2023
23 February 2023 23 February 2023For 20 years Kochaphan Wangtan has been a community health worker, serving other people living with HIV (PLHIV) in Thailand.
“I’ve seen many friends living with HIV come to care very late with opportunistic infections,” she said.
“I focus on helping to bring them in and provide support to start antiretroviral treatment right away and I also conduct home visits, counselling and psychosocial screening so I can link them to services they need,” Ms Wangtan explained.
Ms Wangtan is from the Jai-Prasan-Jai Comprehensive Continuum of Care Center (CCC) from the Phan District Hospital in Chiang Rai province. She is one of almost one thousand PLHIV health workers who are embedded in more than 230 Thai hospitals and serve almost 60,000 PLHIV annually.
For the first time, the country has rolled out a national community health worker certification for these volunteers. The initiative is called “A Comprehensive Continuum of HIV/AIDS Care and Support for and by People living with HIV.” The curriculum was developed by the Ratchasuda College of the Mahidol University through close collaboration with the Thai Network of People Living with HIV/AIDS (TNP+) as well as support from the Health Ministry’s Division of AIDS and STIs and the National Health Security Office. USAID-PEPFAR via the III Unify Collaboration Programme and UNAIDS provided technical and financial support.
“PLHIV volunteers have provided the first community engagement in the HIV response since the start of the epidemic in Thailand,” said UNAIDS Country Director, Patchara Benjarattanaporn. “Peer-led support boosts treatment initiation and retention and is central to the HIV response,” she said. This initiative ensures that PLHIV-led health services are standardized, recognized and valued.
Two modules are delivered over 90 hours. The first module focuses on theoretical training, including on holistic follow-up care, treatment adherence counselling and developing a comprehensive service plan. The second module is practical. Along with its HIV focus, the curriculum also integrates tuberculosis, sexually transmitted infections, Hepatitis C and non-communicable diseases. Earlier in the month the first cohort of 46 PLHIV health workers received their certification.
Dr. Wachara Riewpaiboon, a rehabilitation physician and former Ratchasuda College Dean, developed the curriculum.
“The health system is not only for health professionals… It belongs to everyone,” she said. “Getting an HIV diagnosis does not help clients understand what they are facing. When people living with HIV tell their story, it is very different knowledge they are imparting. The knowledge that helps people make decisions for themselves usually comes from peers, not doctors.”
For her, care goes beyond medicine.
“It is not only biology that we are dealing with, but also psychology and our interaction with our social environment—how people look at people living with HIV and how they perceive themselves,” Dr Riewpaiboon continued. “It is very important to help people see the positive side of their experience.”
According to Nurse Chulaporn SingPae, an HIV Coordinator at the Phan District Hospital, PLHIV volunteers help with counselling, adherence, missed appointment follow-up, home visits, treatment deliveries, overcoming stigma including self-stigma and promoting understanding of U=U, undetectable equals untransmittable. (An undetectable viral load means the virus is not transmittable aka untransmittable.) The training ensures that these contributions are recognized by the health system as meeting quality standards.
Now that the course has been developed and tested, the curriculum has been recognized by the National Health Security Office (NHSO). Thai civil society organizations, who provide HIV and STI services with certified community health workers have been accredited and are eligible to register as health service units in the Universal Health Coverage scheme. Having supported the development and pilot of the curriculum, UNAIDS is now supporting a study to cost these services. The office is also working to promote sufficient and sustainable financing for community-led health services for PLHIV and key populations.
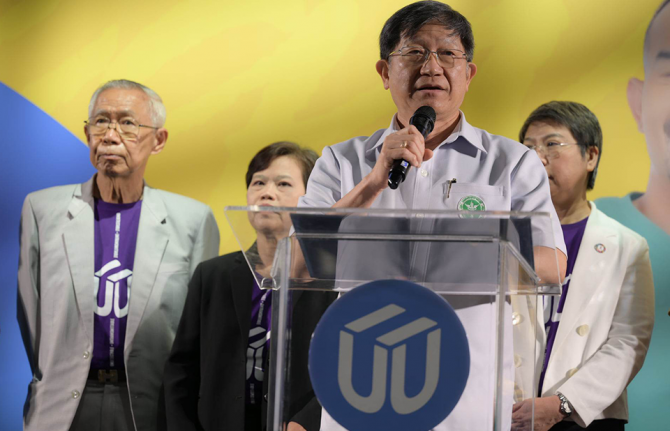
“This training is going to become the guarantee that a peer educator provides a high quality of service, in a holistic way, which encompasses not just the physical but also the mental, emotional and social aspects,” said Apiwat Kwangkeaw, Chairperson of the Thai Network of People living with HIV/AIDS. “As this becomes institutionalized, we are sending a message to the health system as a whole to let the community of peer educators be an equal partner,” he said. Mr Kwangkeaw hopes this will translate into sustainable domestic financing for community-led health services and better quality of life for PLHIV.
Region/country
Related



Feature Story
Preventing transmission and tackling stigma: The power of U=U
12 December 2022
12 December 2022 12 December 2022U=U, which stands for Undetectable = Untransmittable, is a vital public health message for the HIV response. Undetectable = Untransmittable means that people living with HIV who achieve an undetectable viral load through consistent antiretroviral treatment and monitoring cannot transmit HIV. As Thailand has shown, the message of U=U also helps in combatting the stigma which people living with HIV can face in healthcare settings and wider society.
U=U is a priority activity in Thailand’s 2017 – 2030 National Strategy to End AIDS. The approach has already been tested in the capital city, Bangkok. A same-day treatment initiation programme there has resulted in more than 95% of people on treatment achieving viral suppression after just six months of antiretroviral therapy. The national initiative brings together Thailand’s Institute for HIV Research and Innovation (IHRI), the Department of Disease Control, the Ministries of Public Health, Education and Labor, the National Health Security Office, and the Subcommittee on the Promotion and Protection of AIDS Rights, supported by UNAIDS.
Thailand’s wider HIV response has achieved strong results, with an estimated 94% of people living with HIV aware of their status, 91% of diagnosed people on treatment and 97% of those on treatment virally suppressed. But despite these successes, barriers remain as a result of stigma. There are too many late diagnoses, and some people remain fearful about accessing HIV services. To increase use of HIV services, to achieve U=U for all people living with HIV, it is vital to ensure that every person is treated with respect and dignity by the healthcare system.
Dr. Nittaya Phanuphak, Executive Director of the IHRI, emphasized that knowing one’s HIV status is the critical first step to enrolling in antiretroviral treatment.
“People at risk of contracting HIV and people living with HIV from all groups in Thailand must have equal and convenient access to HIV testing and, if positive, to antiretroviral treatment as soon as possible, which will lead to U=U,” said Deputy Minister of the Public Health Ministry, Dr. Sopon Makthon.
Thailand’s U=U initiative embraces a community-led approach which enables people living with HIV to support others who are newly diagnosed to start and stay on antiretroviral treatment. “Community leadership is vital to communicate U=U effectively,” said Patchara Benjarattanaporn, UNAIDS Country Director for Thailand. “This will help tackle stigma and self-stigma, and help boost positive health-seeking behavior.”
Apiwath Kwangkaew, president of the Thailand HIV/AIDS Network, urged all health workers to amplify the message of U=U: “Today's medical personnel must confidently explain U=U to enable social understanding. Health services must be brave and speak up. New understanding will bring change,” Mr. Kwangkaew said.
“UNAIDS welcomes amplification of the message that U=U. It is key to reaching the goal of zero new HIV infections, zero discrimination and zero AIDS-related deaths,” concluded Taoufik Bakkali, UNAIDS’ Regional Director.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Thailand’s Mplus: HIV services delivered in style
13 December 2022
13 December 2022 13 December 2022“This isn’t your mother’s clinic!” said one amazed visitor.
From banners to brochures, all promotional materials are slick and cheerful. Smiling faces and toned torsos are everywhere. A purple colour scheme covers the whole building. Even files and staff face masks are colour coordinated. A pair of Facebook Live hosts have the good looks and energy of K-pop stars. And the organization’s slogan is decidedly upbeat: “where community fulfills your happiness”.
Over almost two decades, Thailand’s Mplus Foundation has refined a unique approach to providing comprehensive HV services to key population clients including men who have sex with men and transgender women.
Their method goes far beyond a cool brand identity. Mplus has leveraged domestic and international partnerships to create a key population-led health service with impressive results. They dispense more than half of the PrEP in Thailand’s Chiang Mai province.
This year they tested 95% of the almost 8000 people they reached with face-to-face services. Of those who tested positive, 91% were placed on treatment while the other 9% are in follow-up case management. And 100% of their clients who received viral load testing were found to be virally suppressed.
“Community organizations can best reach key populations to receive services. We find that people who do not want to get tested at the hospital are comfortable with peers who they know understand their life,” explained Pongpeera Patpeerapong, Director of the Mplus Foundation.
Since its formation in 2003 Mplus has evolved to deliver a full range of services. They now have health centres in four provinces, while their mobile testing units serve clients in another five districts. They support a local hospital in each province, linking people to care and helping them with adherence. Mplus provides rapid testing, CD4 and viral load monitoring, and is also authorized to dispense medication. A small fleet of motorcycles even makes PrEP deliveries to clients in remote areas.
Both their online and offline engagements are anchored by a peer-led strategy. Their social media presence is commanding—everything from Twitter to Tik Tok. There are closed Facebook groups and special applications for clients to connect with community. Offline, they go beyond information booths to host parties and sport meet-ups. These aren’t just bonding exercises. Clients book appointments online and face-to-face interactions usually result in receiving an HIV test.
Mplus also provides technical assistance to other countries. It has supported an organization in Laos with online interventions and helped community groups in Cambodia develop campaigns to promote PrEP.
They played a key role in advocating nationally for the accreditation of community health workers. All Mplus staff are certified by the Department of Disease Control following a rigorous programme of study, evaluation and practice.
The programme continues to progress. Mplus is strengthening their mental and emotional health support offering, and is working towards becoming certified to provide HIV and sexually transmitted infection (STI) treatment.
While in the past the programme was more heavily funded by the U.S. President's Emergency Plan for AIDS Relief through the United States Agency for International Development, today half of their investments come from branches of the National Health Security Office.
“Domestic funding is very important to develop our systems,” Mr. Patpeerapong said. “Community-based organizations have to be able to access domestic funding to cover more issues, including stigma and discrimination.”
Empowering key population-led health services has been crucial in improving Thailand’s HIV programme results. One of five people living with HIV in Thailand were identified and referred by a key population-led health service under the domestic health financing scheme. Four out of five people on PrEP in the country are served by community-led organizations. These services play a critical role in Thailand’s strategy of Reach, Recruit, Test, Treat, Prevent, Retain.
“Thailand is well-positioned to be a leader in addressing the need for a sustainable community-led response as a critical part of the health infrastructure,” said UNAIDS Country Director for Thailand, Patchara Benjarattanaporn. “By creating an enabling system for health outreach we can address the challenge of late diagnosis and better reach key population communities with services.”
Thailand has integrated HIV services into its Universal Health Coverage scheme and increased investments in key population- and community-led health services. UNAIDS Programme Coordinating Board (PCB) members visited Mplus and other community-led health services ahead of the 51st PCB meeting in Chiang Mai, Thailand.
Region/country
Related



Feature Story
The power of bringing together government and community HIV services
15 December 2022
15 December 2022 15 December 2022The Sanpatong Hospital in North Thailand has reinvented and refined its HIV programme for more than three decades. It began attending to people living with HIV in 1989, and in 1996 started offering antiretroviral treatment.
“We have patients who have been with us for 30 years,” says Dr Tawit Kaewprasert, Deputy Director of Provincial Public Health Office and Director of Sanpatong Hospital.
In the last five years the hospital has not had a single case of mother-to-child HIV transmission. An impressive 96% of people on treatment who received viral load tests there this year were virally suppressed, with 98% of those patients being undetectable. Management speaks about the 92% retention rate for clients who were on treatment in 2022 in terms of how those results can be improved.
“We have not achieved that target just yet,” Dr Manusin Kongka says, referring to the proportion of people who stayed on antiretroviral therapy. “But we can reach the target and even achieve beyond 95%.”
The team even aims to achieve 100% viral suppression among people who have been on treatment for at least five years. The current 96% result isn’t considered to be good enough.
This ambitious goal-setting flows from the National HIV Policy and Thailand’s commitment to end AIDS by 2030 through a well-articulated strategy to reach, recruit, test, treat and retain people in care, while also working to prevent new infections.
Of course the strategy relies heavily on Sanpatong and institutions like it. This 130-bed facility boasts a central lab that serves surrounding hospitals in Chiang Mai, Lamphun and Mae Hong Son with HIV diagnosis, CD4, viral load monitoring and some opportunistic infections testing.
Their approach includes the adoption of HIV response best practices including PrEP, index testing and same-day treatment initiation.
“Patients can start treatment before they even get their CD4 result,” Dr Kongka explained.
All staff have received anti-stigma training as well as orientation around the U=U, undetectable = untransmittable, initiative. The facility uses a differentiated approach for antiretroviral treatment delivery. Depending on their health status, some clients can collect multiple month dispensing at district health promoting hospitals while others can receive their medicine by mail.
But a major key to Sanpatong’s success is the linkages it has made with groups of community-led organizations to drive case detection, linkage to care, psychosocial support and the monitoring of services. The Hospital works with Mplus, CAREMAT and FHI360 on prevention, testing and retention in care. Organizations of people living with HIV run support groups. The Community Led Monitoring team even helps primary care nurses to contact patients who have been lost to follow up and conduct home visits. The people living with HIV network collaborated with key community-based organizations in Chiang Mai to conduct community-led monitoring to improve the quality of HIV services at the Sanpatong hospital.
“Our collaboration with community organizations increases awareness about HIV, improves quality of care and access to care, decreases the waiting in community clinics and increases continuity of care for HIV patients,” said Ms Sineenuch Suwansre, HIV Coordinator.
This close collaboration with communities is enhanced by the Thailand Government’s move to integrate HIV services into the Universal Health Coverage scheme. Now certified organizations and lay HIV service providers can access domestic financial support within the national health infrastructure.
“Universal Health Coverage is a mechanism for the sustainable financing of HIV prevention as well as sustainable financial support to key population- and community-led health services. The Thai government’s move to fund Community-led Health Services as an element of the mainstream public health system is a win for people living with HIV, for HIV prevention and for sustainability,” said UNAIDS Thailand Country Director, Patchara Benjarattanaporn.
Our work
Region/country
Related


Press Release
Thailand hosts global HIV meeting this week, showcases AIDS response leadership
11 December 2022 11 December 2022BANGKOK, 11 December 2022—The 51st meeting of the UNAIDS Programme Coordinating Board (PCB) will be held from December 13 - 16 in Chiang Mai, Thailand. The meeting is hosted by the Government of Thailand as Chair of the 2022 PCB. It is the first time in 14 years that the board will meet outside Geneva, Switzerland and the second time it will be in Chiang Mai.
“We are grateful to Thailand for its global AIDS response leadership. The country has taken significant strides toward ending its HIV epidemic and is setting an example for the world of translating political will into action,” said Taoufik Bakkali, Director a.i. of the UNAIDS Regional Support Team for Asia and the Pacific.
Hosting this meeting in Thailand helps sustain momentum in the Asia Pacific region to fulfill commitments made by the community of nations in the 2021 political declaration on HIV, Mr. Bakkali said.
The UNAIDS Programme Coordinating Board meeting demonstrates an inclusive approach. Civil society organizations, including associations of people living with HIV, will sit around the table with member states and UN agencies. The attendees will go together to visit and learn from programmes supporting affected people. “This inclusivity is at the heart of the effectiveness of the UNAIDS approach,” said Mr Bakkali. “Increasingly, it is being asked of international processes where are they being held, who is participating, and how is the process connecting with experiences of the most affected people. This meeting is being held in a country which has so many lessons to share from its AIDS response.”
The UNAIDS Programme Coordinating Board provides oversight and strategic direction for the Joint United Nations Programme on HIV and AIDS, which guides and supports the HIV response globally.
The 22nd PCB meeting in 2008 was also held in Chiang Mai under the auspices of former Public Health Minister, Chavarat Charnvirakul. This meeting will be chaired by his son, Deputy Prime Minister and Minister of Public Health, Anutin Charnvirakul.
The Thailand HIV response
There were an estimated 520,000 people living with HIV in 2021.
Thailand has made considerable progress against AIDS, especially in providing life-saving testing and treatment to people living with HIV. The country was first in the region to be validated as having eliminated mother-to-child HIV transmission in 2016. It has also joined the Global Partnership to Eliminate all Forms of HIV-related Stigma and Discrimination.
Since 2010, AIDS-related deaths have declined by almost two-thirds (65%) while new infections fell by 58%. Last year an estimated 94% of people living with HIV in Thailand were aware of their status. Ninety-one percent of diagnosed people were on treatment and 97% of those on treatment achieved viral suppression.
Ahead of the PCB, delegates will learn about notable Thailand HIV response successes. The country has been a trailblazer for integrating HIV services into the Universal Health Coverage scheme. This has become a mechanism for sustainable HIV response financing by significantly increasing investments in key population- and community-led health services.
Thailand has leveraged several best practices to end AIDS, including legalizing over-the-counter sales of HIV self-test kits, scaling up same-day treatment initiation for newly diagnosed people and successfully rolling-out a pre-exposure prophylaxis (PrEP) programme. (PrEP is a daily medicine taken by an HIV negative person to prevent contracting the virus.) Thailand’s focus on public health, and its efforts in tackling stigma and discrimination, have been key to progress made.
“Thailand is on-track to meet and exceed the 2025 95% testing and treatment targets. To do so it must reach those still not accessing HIV prevention, testing, treatment and care services,” said UNAIDS Country Director for Thailand, Patchara Benjarattanaporn. She noted that a key priority now is for Thailand to get people diagnosed earlier and further reduce new infections. Last year there were an estimated 6500 new HIV infections in Thailand. Critically, half of all new infections occur among young people between ages 15 and 24, most of them among people in key population communities.
“Thailand provides excellent HIV services. Unfortunately, too many young people do not get the prevention information, services and support they need. And some people living with HIV become aware of their status late, with already advanced illness. As we work to reach those being left behind, we must address inequalities in access to information, services and support and continue to innovate and scale up effective, community-led approaches,” Ms. Benjarattanaporn said. “Through bold action to tackle inequalities, we can end AIDS by 2030.”
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Press Statement
Australia and UNAIDS strengthen partnership to advance the end of AIDS
02 December 2022 02 December 20222 December 2022
UNAIDS and the Australian Government have signed a new five-year strategic partnership agreement to advance efforts to respond to HIV in the Asia-Pacific region. The agreement will help to intensify efforts to get back on track to end AIDS by 2030, by addressing the inequalities that hamper the global HIV response.
As part of the agreement, Australia will commit AUD 25 million from 2022 to 2027 to support the global effort to ending AIDS, and to improve HIV outcomes for people in Asia-Pacific.
While Asia-Pacific has seen remarkable progress, many challenges remain. The COVID crisis interrupted vital services across the region, hurting progress. New HIV infections in the region are rising again for the first time in a decade. Key populations, LGBTQI communities, and people with disabilities continue to face unequal access to medicine and healthcare, along with enduring stigma. These inequalities have hindered the HIV response.
The agreement will assist communities and countries to tackle those inequalities, advancing proven approaches which help equalize access to HIV prevention, testing, treatment and care. The agreement recognizes the role of UNAIDS in providing international leadership and coordination to guide the HIV response. It builds on the strengths and experiences of Australia and UNAIDS to ensure strong partnership engagement.
The partnership will enable a robust and sustainable response to HIV which is integrated into the wider context of health and sustainable development in the Asia–Pacific region.
“Australia is a longstanding and valued partner of UNAIDS, said Winnie Byanyima, Executive Director of UNAIDS. This new agreement will help us to build on this partnership and draw on our collective expertise to end AIDS by 2030.”
“The Australian Government is investing in our long-standing partnership with UNAIDS,” said Senator the Hon Penny Wong, Minister of Foreign Affairs. “Our five-year partnership builds upon our efforts to recover lost ground during the COVID pandemic and set our region, and the world, back on the path to ending HIV/AIDS.”
In 2021, 650 000 people were lost to AIDS and 1.5 million people newly acquired HIV. Through bold international action to tackle the inequalities which drive it, the world can end AIDS by 2030.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Region/country


Press Statement
UNAIDS welcomes the decriminalisation of same sex relations by Singapore's Parliament
01 December 2022 01 December 2022Responding to the scrapping of the colonial era law which had criminalised gay men, UNAIDS Regional Director for Asia and the Pacific region Taoufik Bakkali said:
“Everyone benefits from decriminalisation. The end of the criminalisation will save lives.
In all countries which have criminalised gay men, it has had the consequence of obstructing access to vital services. Laws which punish consensual same sex relations, as well as contravening the human rights of LGBT people, are a major barrier to improving health outcomes, including in the HIV response. Punitive legislation embeds stigma and discrimination against LGBT people, and deters LGBT people from seeking healthcare for fear of being denounced to the authorities and facing punishment and detention.
The international momentum to scrap colonial punitive laws will inspire other countries to follow. The evidence is clear: if we are to protect the health of everyone, such harmful laws have no future."
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Region/country




Feature Story
Ahead of World AIDS Day, ASEAN countries recommit to ending inequalities and accelerating progress to end AIDS
25 November 2022
25 November 2022 25 November 2022Member States of the Association of Southeast Asian Nations (ASEAN) have reaffirmed their commitment to accelerate progress toward ending AIDS as a public health threat by 2030.
At the 40th and 41st ASEAN Summits under the Chairmanship of the Kingdom of Cambodia, Member States pledged to strengthen community-led responses and increase financing for the HIV response. Echoing the World AIDS Day call to “equalize” the AIDS response, country leaders also agreed to a comprehensive agenda to end the inequalities stalling progress.
The ASEAN Leaders’ Declaration on Ending Inequalities and Getting on Track to End AIDS by 2030 is aligned with the 2021 UN Political Declaration on HIV and AIDS and the 2021–2026 Global AIDS Strategy and targets.
"We are now in an era where treatment and various options on HIV prevention can be made available and accessible, and it is important to shine a light on where inequalities and gaps continue to persist if ASEAN is to sustainably accomplish these targets,” said H.E. Ieng Mouly, Senior Minister and Chair of Cambodia’s National AIDS Authority.
In 2021 there were an estimated 1.9 million people living with HIV in ASEAN countries and an estimated 78,000 new HIV infections. In most ASEAN countries there are now rising epidemics among young gay men and other men who have sex with men and transgender people.
“Wherever communities are being left behind, ASEAN remains vulnerable to the social and economic fallout of HIV,” said UNAIDS Asia Pacific Regional Director, Taoufik Bakkali. “This Declaration is important and timely. It paves the way for countries to comprehensively address the large gaps in service coverage that remain in several countries, particularly for key populations.”
The ASEAN Declaration calls for focus on key and marginalized populations and explicitly addresses the needs of people living with HIV, men who have sex with men, transgender people, people who inject drugs, sex workers and their partners. It contains wide-ranging commitments, including concrete strategies to achieve the 95-95-95 testing and treatment targets. (By 2025, 95% of people living with HIV in all countries and communities to be aware of their status, 95% of all diagnosed people on treatment and 95% of those on treatment achieving viral suppression.)
End inequalities
ASEAN states have committed to better facilitate the participation of people living with HIV. They pledged to remove barriers to HIV services by improving policy and legal environments. This includes taking steps to reform discriminatory and punitive laws such as those that criminalize key populations and block adolescents from accessing HIV prevention, testing and treatment, and restrict the entry, stay, and residence of people living with HIV. Countries further agreed to take steps to eliminate stigma and discrimination against people living with HIV and key populations in healthcare, education, and workplace settings, as well as in communities.
Strengthen, support and sustain community-led responses
Governments said they would ensure the inclusion of people living with HIV, and communities most affected by HIV, in AIDS response planning, implementation and evaluation. Community organizations, and particularly community- and peer-led interventions, should be strengthened and scaled-up. States agreed to continue investing in community-led service delivery, including by adopting and implementing social contracting policies. They also promised to support community-led monitoring and research.
Finance and sustain the AIDS response
The alliance agreed to address HIV response financing shortfalls by raising sufficient domestic and international financial resources to fill gaps. At the same time, they committed to developing and implementing plans to transition from external to domestic funding. They promised to work to improve efficiency in the use of existing financial resources, including through integration with health and humanitarian responses and universal health coverage mechanisms. They also agreed to regional cooperation for research, sharing good practices, joint interventions and to strategize for improved access to health commodities.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Asia-Pacific youth demand robust action to lower the HIV risk of young key populations
25 October 2022
25 October 2022 25 October 2022Youth advocates from 14 countries have called on governments and development partners in the Asia-Pacific region to adopt a comprehensive approach to addressing the high HIV risk now borne by young key populations. (Key populations are groups that are particularly vulnerable to HIV. They include men who have sex with men, people who use drugs, sex workers and transgender people.)
Held on October 20 and 21 in Bangkok, the 2nd Asia Pacific Youth Forum was co-organized by the Thailand Ministries of Public Health and Foreign Affairs, the UNAIDS Regional Office for Asia and the Pacific and Youth LEAD. Among other priorities, delegates advocated for more youth leadership, equitable access to quality and youth-friendly healthcare services, stronger strategies to tackle stigma and discrimination and increased access to funding for youth-led and key population programming.
UNAIDS data reveal that in 2021 there were an estimated 260 000 new HIV infections in Asian and Pacific countries. According to a recent report by UNAIDS, UNICEF, UNFPA and Youth LEAD, young people aged 15–24 years accounted for 26% of these cases. In some countries including Cambodia, Indonesia, Laos, the Philippines and Thailand, more than 40% of new infections were among youth. HIV transmission to young people rose for seven countries in the region since 2010—Afghanistan, Fiji, Malaysia, Pakistan, Papua New Guinea, the Philippines and Timor-Leste. Strikingly, in the 15 - 24 age-group, almost all (99%) new infections regionally were among people from key populations and their partners.
“Preventing HIV, STIs and all emerging diseases among young people requires addressing the root causes that put young people at risk, including gender-related, socio-economic inequalities, and stigma and discrimination,” said Mr. Satit Pitutacha, Thailand’s Deputy Minister of Public Health.
Ms Eksiri Pintaruchi, Director-General of the Department of International Organizations in the Thailand Ministry of Foreign Affairs highlighted the work of the Thai Network of Young People Living with HIV including providing peer support for young key populations, linking them to services, offering life skills training, mental health support and psychosocial care.
UNAIDS Asia and Pacific acting Regional Director, Mr Taoufik Bakkali said: “We need to address the inequalities that create vulnerability. By investing in youth today we will not only achieve a win for the HIV response, but also significant progress for the Sustainable Development Goal agenda.”
Youth LEAD’s Project and Networking Officer, Legee Tamir, noted the crucial need to increase spaces for youth leadership, especially as young key populations are still left behind in national, regional and global decision-making spaces where their voices would make a difference.
On day one of the forum youth delegates convened to share experiences. They noted legal and policy barriers including the age of consent, concerns about privacy and confidentiality and stigma and discrimination among healthcare providers. The opening hours of public clinics are not convenient for young people and services are not tailored to meet their needs.
The consultation resulted in nine recommendations which were presented to government and development stakeholders on the forum’s second day. They are as follows:
- Strengthen the leadership and meaningful engagement of young people, including young key populations and young people in all their diversity, within the HIV response
- Increase awareness about existing HIV and sexual and reproductive health and rights programmes for young key populations
- Engage and collaborate with stakeholders (including governments, the private sector, communities, media) in advocacy campaigns
- Ensure equitable and convenient access to HIV services, including for youth in rural areas, and modernise HIV services
- Tackle harmful stigma and discrimination in household, education and healthcare settings through funding and partnering with efforts led by young key populations that address deeply rooted traditional beliefs and practices
- Review and reform laws and policies that affect young key populations and ensure they are aligned with international human rights norms and recommendations
- Ensure the availability and accessibility of quality, youth-friendly and non-discriminatory programmes and services that ensure the mental wellbeing of young key populations
- Invest in the organisational strengthening and sustainability of youth-led organisations at different capacities
- Empower youth-led organisations and create more conducive, flexible and simpler processes to access opportunities for external and domestic funding
UNAIDS and its regional partners through the Asia Pacific Inter Agency Task Team on Young Key Populations will use this set of recommendations to inform future initiatives for young key populations in the region.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Indonesia: Helping one family at a time through Lentera Anak Pelangi’s One Child One life program
10 October 2022
10 October 2022 10 October 2022Estimates indicate that in Indonesia in 2021, only 25% of the 19,000 children living with HIV received life-saving antiretroviral therapy and 2,400 children died from AIDS-related causes.
Despite global scientific breakthroughs providing more effective treatment for adults and children, for many children living with HIV in Indonesia access to antiretroviral therapy remains elusive. Exacerbating the situation is the entrenched societal and gender inequalities that present barriers to women, adolescents and children to access quality prevention and care services.
With many competing priorities, national and local commitment of resources to scale-up efforts to eliminate vertical transmission of HIV and increase ARV coverage among children living with HIV remain limited. This has resulted in insufficient investment in community-based services for women, adolescents and children living with HIV.
To reduce AIDS-related deaths among children, and ensure children and adolescents living with HIV have access to high quality comprehensive care and support, Indonesia must expand community-based services and community-led programmes tailored to the needs of these very vulnerable yet often left-out groups.
Lentara Anak Pelangi (LAP), an organization that provides HIV services, including psychosocial support, for children and adolescents living with HIV in Jakarta has seen some successes through their One Child One Life program.
“We want these adolescents to be the next generation of positive leaders and influencers who inspire other teens living with HIV” said Prof. Irwanto, founder of Lentera Anak Pelangi.
The One Child One Life program provides disclosure and post-disclosure support, mental health assessment and care as well as education.
“Lentera Anak Pelangi has supported my daughter since she was very young. LAP’s in-person and online activities have been very helpful for her. Through Sekolah LAP, my daughter has started to learn how to build her self-confidence and open her mind to learn more things. I also learned the meaning of this illness and find friends facing the same struggle and fight to continue to be healthy,” Explained the mother of one LAP beneficiary.
“My son and I have been greatly helped by LAP’s education support. During the pandemic, we often received sembako (staple foods). My son loves to be part of LAP because he gets to meets other teens who share similar circumstances. We also receive information on how to provide care for our family,” another mother said.
Through the One Child One Life program, children living with HIV have been supported to suppress their HIV viral load, return to school and participate in youth support groups. LAP also supports children with special needs and supplemental nutritional support when required. However, their coverage remains small due to funding and human resource constraints.
“Science has made it possible to diagnose and treat HIV. We have come a really long way in 40 years. In Indonesia, we must eliminate vertical transmission of HIV and ensure that all children living with HIV access life-saving antiretroviral therapy and quality care including psychosocial support when needed.” said Krittayawan Boonto, the UNAIDS Country Director for Indonesia.”
UNAIDS Indonesia together with Lentera Anak Pelangi and other implementing partners continue to call for optimized investments in community-based services and community-led programmes for women, adolescents and children living with HIV.



